Kewal Krishan Gupta, MD1, Amanjot Singh, MD1, Gurpreet Singh, MD2, Haramritpal Kaur, MD1
1Assistant Professor; 2Associate Professor
Department of Anesthesiology and Intensive Care, GGS Medical College & Hospital, Faridkot, Punjab (India)
Correspondence: Dr. Kewal Krishan Gupta, House No. 204, Medical Campus, Faridkot 151203, Punjab (India); Tel: +91-9988316306; E-mail: doc_krishan31@yahoo.co.in
ABSTRACT
Klippel-Fiel syndrome is one of the common congenital causes of difficult airway which is characterized by failure of normal segmentation of cervical vertebra resulting in short neck with restricted movement and cervical instability. This anomaly increases the risk of neurological damage during airway instrumentation like laryngoscopy and positioning for surgery. We report a case of 60 year old female patient with Klippel-Fiel syndrome posted for ear surgery under general anesthesia. She was successfully managed by using awake fibreoptic technique for endotracheal intubation.
- Keywords: Klippel-Fiel syndrome; Klippel-Feil Syndrome/complications; Klippel-Feil Syndrome/pathology; Difficult airway; Fiberoptic intubation; Intubation, Intratracheal/adverse effects; Fiber Optic Technology
.
Citation: Gupta KK, Singh A, Singh G, Kaur H. Klippel-Fiel syndrome and anesthetic challenges – A case report and review of literature. Anaesth Pain & Intensive Care 2015;19(4):510-513
INTRODUCTION
Klippel-Feil syndrome (KFS) is known by the classic triad of short neck, limitation of neck movements, and a low posterior hairline. Maurice Klippel and Andre Feil described it independently in 1912.1 KFS has an incidence of 1:42,000 births and is one of the common congenital causes of difficult airway.1,2 The main anesthetic challenge with these patients is a potential spine abnormality prone to an increased risk of neurological damage during airway management.3 Hence their anesthetic management should be carefully planned keeping in mind the other abnormalities associated with this syndrome. We report successful anesthetic management in patient with KFS with associated anomalies. We also review the literature regarding the various methods used for airway management in these cases.
CASE REPORT
A 60 year old female was planned for recannaliztion of ear for external auditory canal stenosis under general anesthesia. On preanesthetic checkup, she was found to be short statured with 145 cm height and 65 kg weight. On airway examination, she had short, webbed neck and limited neck extension and flexion movements and a low-lying posterior hair line (Figure 1).
Figure 1: KFS features including short neck with low lying posterior hair line
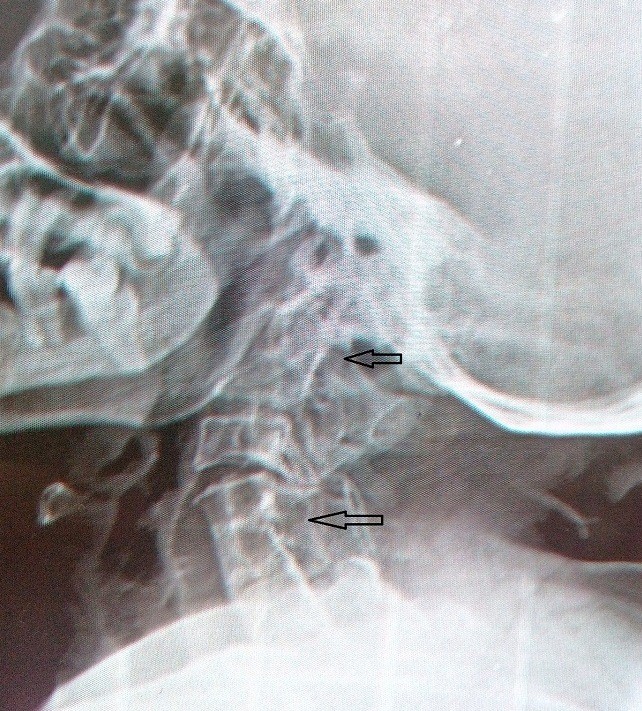
All these features suggested that she was a case of KFS. She had Mallampati grade III with adequate mouth opening and a thyromental distance of 6 cm. Systemic examination revealed no abnormality except Sprengel’s deformity of shoulder. All routine investigations including echocardiography were within normal limits, except fused cervical spines at upper and lower levels with failure of complete segmentation on cervical spine x-ray films (Figure 2). Ultrasound abdomen showed a solitary kidney on right side. Due to cervical abnormality and restricted movement of neck, difficult airway was anticipated and an awake fiberoptic intubation (FI) was planned to secure airway for general anesthesia. After explaining all the risks in her operation and chance of tracheostomy, a written informed consent was obtained before surgery. On the day of surgery IV access was secured and monitors were attached. A plan to secure her airway with local anesthesia was made and the maximum dose of local anesthetic was calculated. The patient was given 4 ml of 2% xylocaine viscous gargles and was allowed to swallow it to coat the posterior surface of the epiglottis. Then two aliquots of a 10% xylocaine spray were instilled posteriorly into the mouth during deep inspiration.. After 10 min patient was shifted in operating room with monitors, inj. glycopyrrolate 0.2 mg was given to reduce secretion and inj. fentanyl 50 µg to make the patient comfortable. Through transtracheal approach, an injection of 2 ml of 2% xylocaine was given at inspiration to anesthetize the trachea and vocal cords. Then Berman airway lubricated with xylocaine jelly was inserted in the mouth. After threading a 7.0 mm ID cuffed endotracheal tube over the bronchoscope, the scope was carefully maneuvered through airway. As we tried to negotiate bronchoscope through the vocal cords, patient had a bout of cough. So 2 ml of 2% xylocaine solution was injected through the side port of the fiberoptic bronchoscope, using the ‘say go’ technique (spray as you go) to anesthetize the vocal cords. Then fiberoptic bronchoscope was introduced into the trachea, and the tracheal rings with carina identified. Immediately inj. propofol 100 mg was given and endotracheal tube threaded over the bronchoscope into trachea. Correct position of tube was confirmed after removal of bronchoscope with 5 point auscultation and capnography. Then anesthesia was maintained on isoflurane with 60%: 40% ratio of N2O and oxygen with IPPV. Inj. vecuronium was used as muscle relaxant. Surgery proceeded uneventfully and inj. atropine 20 µg/kg with inj. neostigmine 50 µg/kg was used for reversal of neuromuscular blockade. Patient was extubated after return of spontaneous breathing and recovery of adequate muscle power. Postoperative period was uneventful.
DISCUSSION
KFS is one of the common congenital causes of difficult airway which occurs due to abnormal segmentation of the cervical somites in the 3rd to 8th week of gestation.4 Out of three variants of KFS, Type I is an extensive abnormality in which several cervical and upper thoracic vertebrae are fused into a single block. In Type II variant, failure of complete segmentation occurs at one or two cervical interspaces. Type III variant includes Type I or II deformities with coexisting segmentation defects in the lower thoracic or lumbar spine. Most common form is Type II and it commonly involves C2-3 and C5-6 interspaces. Other common anomalies associated with KFS include kyphoscoliosis, deafness, renal abnormalities, synkinesia, Sprengel’s deformity, and congenital heart disease.5, 6 Ventricular septal defect is the most common cardiac anomaly, occurring in 14 – 29 % of these patients.7
In our case, it is most likely type II variant with involvement of C2- C3 and C5 – C7 interspaces. Associated anomalies were sprengel’s deformity and deafness. Patients with KFS may present for various surgical procedures at different ages. Commonly involved surgical procedures are cervical spine surgery, scoliosis correction, spinal canal stenosis surgery, renal surgery, cesarean section and eye or ear surgery.
The main anesthetic concern with these patients is the airway management during general anesthesia due to potential unstable cervical spine and abnormal atlanto-occipital junction, and an increased risk of neurological damage.8 Although, several methods of securing airway have been reported in these patients but a specific standard recommendation on airway management doesn’t exist. An awake fiberoptic intubation seems to be the most effective and safe method by Daum and Jones but sometimes found difficult and time consuming also.9 Direct laryngoscopy with manual cervical stabilization has also been used successfully but even slight extension at atlantoaxial joint can cause damage to spinal cord.10 On the other hand, traction maneuver may limit the orolaryngeal alignment and make intubation more difficult. Neurological worsening following intubation under manual neck stabilization has not been reported.8 Cricothyroidotomy is considered to be a good alternative, but an obstruction in to the operative field remains a concern. Bullard laryngoscopy has been proposed to be safe by some authors, but limited availability has made it less popular.11 The intubating LMA has also been used successfully for intubation without head and neck manipulation.12 But posterior displacement of the normal cervical spine due to cervical pressures generated by the laryngeal mask devices was also observed.13 O’Conner and Moysa reported that airway control can be temporarily lost after induction and an LMA might be required to secure the airway.14
Due to earlier anticipation of difficult airway in these patients, it is indispensable to secure the airway before induction of general anesthesia especially in emergent cases. So we used awake fiberoptic intubation for airway management in our case. This technique has a number of advantages, e.g. (1) an awake, spontaneously breathing patient, who maintains own airway, (2) no spinal movement during intubation, (3) allows confirmation of tracheal tube placement, (4) a high success rate (5) a lower rate of complications, and (6) better patient acceptance.15 Despite numerous advantages, failure of fiberoptic intubation with complications like massive subcutaneous emphysema or airway injury have been reported.16, 17
In conclusion, a thorough airway assessment and adequate preparation is a critical component for airway management in these cases. After considering all the modes of airway management, we advise awake fiberoptic intubation is the safest option for securing the airway in a patient with KFS.
REFERENCES
- Klippel M, Fell A. Un cas d’absence des vertebres eervieales. Soc Anat Paris Bull ET Mem 1912; 14:185.
- Gunderson CH, Greenspan RH, Glaser GH, Lubs HA. The Klippel-Feil syndrome: genetic and clinical reevaluation of cervical fusion. Medicine 1967; 46: 491-512.
[PubMed]
- Khawaja OM, Reed JT, Shaefi S, Chitilian HV, Sandberg WS. Crisis resource management of the airway in a patient with Klippel‑Feil syndrome, congenital deafness, and aortic dissection. Anesth Analg 2009; 108:1220‑
[PubMed]
- Kaplan KM, Spivak JM, Bendo JA. Embryology of the spine and associated congenital abnormalities. Spine J 2005; 5:564‑
- Nagib MG, Maxwell RE, Chou SN. Identification and management of high-risk patients with Klippel-Feil syndrome. J Neurosurg 1984; 61:523-30.
[PubMed] [Free full text]
- Chattopadhyay A, Shah AM, Kher A, Bharucha BA,Karapurkar AP. Craniosynostosis and Klippel-Feil syndrome: Its association. Indian J Paediatr 1996; 63:819-22.
[PubMed]
- Singh M, Prasad R, Jacob R. Anaesthetic challenges in a patient with Klippel-Feil syndrome undergoing surgery. Indian J Anaesth 2005; 49:511-4.
- Whittle IR, Besser M. Congenital neural abnormalities presenting with mirror movements in a patient with Klippel-Feil syndrome. Case report. J Neurosurg 1983; 59:891-4.
[PubMed] [Free full text]
- Daum RE, Jones DJ. Fibreoptic intubation in Klippel-Feil syndrome. Anaesthesia 1988; 43:18-21.
[PubMed] [Free full text] DOI: 10.1111/j.1365-2044.1988.tb05416.x
- Stallmer ML, Vanaharam V, Mashour GA. Congenital cervical spine fusion and airway management: a case series of Klippel-Feil syndrome. J Clin Anesth, 2008; 20:447-451.
[PubMed] doi: 10.1016/j.jclinane.2008.04.009.
- Baraka A, Muallem M, Sibai AN, Louis F. Bullard laryngoscopy for tracheal intubation of patients with cervical spine pathology. Can J Anaesth 1992; 39:513-4.
[PubMed]
- Al Zahrani T. Reverse LMA insertion in a neonate with Klippel-Feil syndrome–case report. Middle East J Anesthesiol 2007; 19:625-9.
[PubMed]
- Keller C, Brimacombe J, Keller K. Pressures exerted against the cervical vertebrae by the standard and intubating laryngeal mask airways. Anesth Analg 1999; 89:1296-1300.
[PubMed]
- O’Connor PJ, Moysa GL, Finucane BT. Thoracic epidural anesthesia for bilateral reduction mammoplasty in a patient with Klippel‑Feil syndrome. Anesth Analg 2001; 92:514‑
[PubMed]
- Cohn AI, Zornow MH. Awake endotracheal intubation in patients with cervical spine disease: a comparison of the Bullard laryngoscope and the fiberoptic bronchoscope. Anesth Analg 1995; 81:1283-6.
[PubMed]
- Richardson MG, Dooley lW. Acute facial, cervical, and thoracic subcutaneous emphysema: a complication of fiberoptic laryngoscopy. Anesth Analg 1996; 82:878-80.
[PubMed]
- Maktabi MA, Hoffman H, Funk G, From RP. Laryngeal trauma during awake fiberoptic intubation. Anesth Analg 2002; 95:1112-4.
[PubMed]