Rajendra Kumar Sahoo, MD, CIPS, ASRA-PMUC, Pain Fellowship1,
Abhijit S Nair, MBBS, MD, PGCC 2, Usha R Badole, MD3, Rajesh Kar, MD, PDCCA1, Ashok Jadon, MD, DNB, MNAMS, FIPM, FIPP, FAMS4
1Senior Consultant, Anesthesiology & Pain Management,
Healthworld Hospitals, Durgapur, West Bengal, India, 713216
2Consultant Anesthesiologist
Indo-American Cancer Hospital, Banjara Hills, Hyderabad, India
3Professor, Dept of Anesthesiology and Critical Care
Grant Medical College and Sir J.J Group of Hospitals, Mumbai, India
4Chief Consultant / HoD, Anesthesiology & Pain
Tata Motors Hospital, Jamshedpur, India
Correspondence:
Dr. Rajendra Kumar Sahoo
Senior Consultant, Anesthesiology and Pain Management
Healthworld Hospitals, Durgapur, West Bengal, India, 713216; E-mail: sss.raaj@gmail.com
ABSTRACT
Pain is a major problem in patients admitted in the Intensive Care Units (ICU). Untreated pain has significant impact on the outcome of these patients, especially surgical patients. There is enough evidence in the literature which has demonstrated that inadequately treated pain in ICU leads to prolonged ventilation, longer ICU stay, morbidity and other issues like development of post-traumatic stress disorder (PTSD) and chronic post-surgical pain (CPSP). Regional anesthesia and analgesia (RA) techniques like epidural analgesia, paravertebral blocks, and other peripheral nerve blocks (PNB) play a great role in providing significant pain relief, thus, limiting the use of opioids. They facilitate in earlier weaning from ventilation, reducing respiratory morbidity, and faster rehabilitation. These RA techniques are most useful in polytrauma patients, major thoracoabdominal and orthopedic surgeries, as many of them require post-surgical ICU care. However, these RA techniques are underutilised in many ICUs. Many a times, ICU physicians are not well versed with these RA techniques, and sometimes have fixed misconceptions with regards to these blocks. In this review, we will discuss on the need of these RA techniques and make a quick presentation on the technical aspect of frequently used blocks. The review will only focus on Ultrasound-guided regional analgesia (USRA) techniques as USG is commonly available in ICUs.
Keywords: Analgesia, Regional; Anesthetics, Local/therapeutic use; Critical Care; Intensive Care Units; Ketamine/therapeutic use; Lignocaine/therapeutic use; Pain Management; Pain, Postoperative/therapy; Anesthetics, Local; Dexmedetomidine
Abbreviations: PTSD (Post-traumatic stress disorder), CPSP (Chronic post-surgical pain), RA (Regional anesthesia and analgesia), USRA Ultrasound-guided regional analgesia), PNB (Peripheral nerve block), IFPB (Interfascial plane blocks), ASRA (American Society of Regional Anesthesia and Pain Medicine),
Citation: Sahoo RK, Nair AS, Badole UR, Kar R, Jadon A. Role of regional analgesic techniques in ICU. Anaesth Pain & Intensiv Care 2018;22 Suppl 1:S73─S82
Received: 8 Sep 2018, Reviewed: 16 Sep 2018, Accepted: 15 Oct 2018
INTRODUCTION
Pain is a very common problem in patients admitted to ICU. It has been found that as many as 50-70% patients admitted to the ICU suffer from moderate to severe intensity pain.1-5 This is despite recent advances in technology like USG, newer drugs, varieties of opioids, and better understanding of pain pathophysiology. In a study of traumatic critically ill patients admitted to ICU, 74% of patients reported their pain as moderate or severe. Interestingly, 95% physicians and 81% nurses felt that the patients’ analgesic regimen has been adequate.6 This clearly demonstrates that pain is highly neglected in ICU patients.
In the ICU setting, the source of pain can be from multiple sources. In trauma patients, it can be from rib fractures, to major axial skeleton or long bone fractures. Similarly, in post-surgical ICU patients (major orthopedic, thoracoabdominal, vascular or spine surgery), the pain from surgical site is moderate to severe in intensity. Apart from that, many patients have chest drains, multiple catheters, need frequent physiotherapy and position change adds up to the existing pain. It is imperative to provide effective pain relief which not only reduces pain intensity but also facilitates earlier recovery and rehabilitation. Adequate pain relief in trauma patients with multiple rib fractures helps in early weaning from ventilation, maintenance of effective oxygenation, rehabilitation and shorter ICU stay. There is accumulating evidence to suggest that development of chronic pain can be prevented if acute pain is managed effectively.5-7
Pain management in postoperative patient as well as ICU setting should always be multimodal as it helps in reduction of opioid use, lesser opioid related side effects, and better analgesia. High dose and long-term opioid use can lead to nausea, vomiting, respiratory depression, urinary retention, tolerance, dependence, ileus, delirium and difficulty in assessing neurological function because of sedation. Hence, an appropriately used regional anesthesia and analgesia (RA) technique reduces most of the opioid related side effects to a great extent. RA techniques range from commonly used epidural analgesia (for thoraco-abdominal surgery or trauma, pelvic or major limb reconstructive surgery), paravertebral blocks, intercostal blocks, to recent interfascial plane blocks (IFPB) for chest or abdomen, and extremity nerve or plexus blocks. With growing popularity and wide availability of USG in ICU, many of these peripheral nerve blocks (PNB) can be performed safely and accurately for many patients. In this review, we’ll discuss on these PNBs, and briefly describe USG guided technique to help clinicians utilize RA technique for the larger benefit of patients.
UNIQUE PROBLEMS IN ICU AND IMPLICATIONS FOR RA
- The Problem of Chronic Post-ICU Pain:
Majority of ICU patients experience pain during their hospital stay. Some of them unfortunately end up with persistent post-ICU pain. A recent trial found that the 6 months post-ICU chronic pain prevalence rate was 33% out of 202 surgical and medical ICU patients.8 Studies have found that a great majority of post-surgical patients (10-50%) develop CPSP.9 There are patient and procedure-specific risk factors for development of CPSP. All cardiac, aortic, major orthopedic, thoracotomy, and major abdominal surgeries require post-operative ICU stay and are individualized risk factors for development of CPSP.9-11 Younger age, female sex, patient’s genetic endogenous analgesic system, preoperative and postoperative pain intensity, level of opioid exposure in pre-surgery period and untreated severe pain in post-operative period are all recognized as risk factors.10-12 Out of all the modifiable risk factors, perioperative RA improve patient’s status and outcomes.5,13,14 The mechanism for development of CPSP in ICU is because of peripheral and central sensitization that can occur after persistent acute pain or input of triggering factors.
- Coagulopathy and Anticoagulation:
Coagulopathy is a big hurdle for performing RA procedures in ICU patients, especially epidural analgesia or deep peripheral nerve blocks or catheters. Many patients in ICU receive anticoagulation to reduce the possibility of deep vein thrombosis. Moreover, some patients develop bleeding diathesis during the course of their treatment in ICU. Thrombocytopenia or other clotting disorders are not uncommon in ICU patients. However, same principle applies for epidurals or PNBs as that of a surgical patient on anticoagulant. Recently, American Society of Regional Anesthesia and Pain Medicine (ASRA) published its 4th guidelines on anticoagulant and regional anesthesia management, and readers are requested to read and adhere to the guidelines for patient safety.15 At the end, benefit-risk-ratio should be taken into consideration and an individualized approach should be followed.
- Infection:
Presence of serious infection also poses a problem for safe performance of RA technique. However, this holds true if there is significant systemic infection or infection at the site of injection. Neuraxial blocks are relatively contraindicated in patients with systemic infection. However, single shot PNB is not an issue if there is no infection at the injection site. But, sterile precautions should be followed while performing single shot or continuous PNBs.
- Hemodynamic Instability:
In hemodynamically unstable patients, neuraxial blocks are contraindicated as it causes further sympatholysis and can increase the dose of vasopressors and inotropes. However, a PNB can be offered to such patients because once analgesia is provided, patient will not need other drugs like narcotics which can further cause hemodynamic compromise.
- Heavy Sedation or use of Neuro-muscular Blocking Agents (NMBA)
Often patients in ICU are on sedatives or may be paralysed with NMBA when getting ventilated. Performing RA techniques in them is a very controversial topic itself. Neuraxial techniques like epidurals, especially thoracic epidurals should be done by experts as patient will not provide any feedback in case of trauma of spinal cord with inadvertent puncture. However, PNBs using ultrasound can be performed safely in trained hands. Needle tip should always be visualized, and appropriate volume and concentration of LA should be used. A heavily sedated patient cannot give consent for a regional anesthesia procedure. In such situations, family members should be explained the pros and cons and the procedure could still be performed once consent is available.
- Multiorgan dysfunction
Multiorgan dysfunction leads to coagulopathy, renal insufficiency/ failure, hepatic dysfunction, altered mentation, thus limiting use of many systemic analgesics. This can make decision making complicated. Therefore, the decision has to be taken based on the severity of each organ and plan has to be made to make the patient pain free. In fact, RA techniques can be a boon in these patients. However, the dose, concentration, and volume of the LA should be taken into consideration as they get metabolized or excreted through liver or kidney.
COMMON RELEVANT RA TECHNIQUES UNDER USG IN ICU
- Thoracic Paravertebral Block (TPVB):
Indications: Rib fractures, thoracotomy, major thoracic and cardiac surgical patients
Thoracic epidural analgesia (TEA) is considered gold-standard to provide analgesia following multiple rib fracture, chest wall trauma, and major thoracic surgery. However, hypotension, leading to hemodynamic instability, urinary retention, and technical challenge to perform at mid-thoracic level are the limitations. But, they have been found to prevent and reduce the incidence of CPSP following major open lung surgery.14 Hence, TPVB is an alternative to TEA, and has been found to provide similar analgesia.
Technique: A linear array high frequency US probe is used for the TPVB. In ICU patients, this could be performed in lateral decubitus position. The desired spinous process should be identified counting down from C7. A point can be marked with a marker pen at 2.5-3 cm from the spinous process. Perform a scout scan with the probe in sagittal (craniocaudal) orientation 2-3 cm from midline and identify TP, pleura and superior costotransverse ligament (SCTL) just above the pleura. TP and ribs are visualized as hyperechoic structures with acoustic shadowing below them (Figure 1). A Tuohy’s needle or a block needle is inserted in-plane from cranial to caudal direction or vice versa. The needle can be inserted in out-of-plane as well. The needle should be seen throughout the procedure as pleural puncture and pneumothorax is a known complication of this procedure. In cases where the structures are not identifiable easily, it is suggested not to perform this block. Once SCTL is entered, LA (usually 20 ml for a single level injection) can be injected.
Another approach, is transverse scan to identify the apex of thoracic paravertebral space (TPVS). With this approach, spinous process is identified in the midline, and as the probe is moved laterally, lamina with erector spinae muscle on the top and then transverse process is identified. Further moving the probe in cephalo-caudad direction, the space below the rib and internal intercostal membrane (IIM) along with moving pleura is identified (Figure 2). The block needle is inserted in-plane from lateral to medial and IIM is punctured to deliver LA in the apex of TPVS. In both the approaches, deepening of pleura is observed and that is considered as the tell-tale sign of successful blockade.
- Erector Spinae Plane (ESP) block:
Indications: Rib fractures, chest wall trauma, and post-thoracotomy pain.
ESP block is a recently described IFPB technique and the first literature was for thoracic neuropathic pain.16 In recent times, this simple block has become very popular and has been used for many conditions, including thoracic pain, thoracic trauma, rib fracture, thoracic or abdominal surgical patients either by single shot block or continuous technique.17-19 However, majority are case reports/ series. We have to wait for formal randomized trials to find out the benefits when compared with standard techniques like TEA or TPVB. But, it is quite promising from the initial cadaveric studies showing dye spread up to somatic nerves or even sympathetic chain and intercostal space.20
Technique: Appropriate thoracic spinous process is identified by counting from C7 spinous process which is easily palpable. Injection is usually performed at T3-T5 level, but, it can be done even at mid-to-lower thoracic levels. Spinous process can be identified and marked as well. A linear high frequency probe is usually used for an ESP block which should be placed in cranio-caudal orientation in midline at the spinous process level and then moved laterally to identify transverse process (TP). TP is approximately at 2.5-3 cm distance from spinous process. Erector spinae muscle (ESM), rhomboidus major and trapezius muscle should be identified from deep to superficial when the block is done at T3-5 level (Figure 3). Under aseptic technique and after skin infiltration with 2% lidocaine, a 18G Tuohy needle or block needle is introduced in-plane craniocaudally to contact with TP. Hydrodissection with NS should be done to confirm separation of ESM from TP. Once confirmed, 20 ml LA can be injected in aliquots of 5 ml. Once the drug is injected, an epidural catheter can be threaded and secured in ESP plane for continuous block.
- Intercostal Block (ICB):
Indications: Rib fractures, post-thoracotomy pain.
Technique: USG guidance helps in accurate deposition of LA in the right place and decreases the chance of intravascular injection, and pneumothorax. With USG, the block can be performed before the division of the lateral branch which is essential for blocking an entire intercostal dermatome. To begin with, the individual ribs needs to be identified and marked as done with the landmark technique. In a sagittal plane, the USG probe is placed about 6-7 cm lateral to the spinous process at the level of angle of rib before branching of thoracoabdominal nerve. The ribs are identified as a round shaped superficial hyperechoic structure with acoustic shadow and shimmering pleura further down. In between two ribs, the layers of intercostal muscles (from superficial to deep: external intercostal, internal intercostal and innermost intercostal when scanned at the angle of the rib) are identified (Figure 4). The needle can then be inserted in or out of a plane until the tip is just below the inferior border of the rib between internal and innermost intercostal muscle. In-plane approach is preferred, and the needle tip should always be under vision to avoid inadvertent vascular or pleural puncture. Though, the intercostal vessels and nerves are classically described to have a subcostal location, there is anatomical variation, and the nerve can be well below the subcostal groove.21 Colour doppler should be employed to identify these vessels and needle insertion should be done accordingly. After negative aspiration, 2-4 mL of LA is injected which will push the pleura away. Unlike TPVB, or ESP block, ICB has to be done at multiple levels depending on the dermatome, myotome that needs to be covered.
- Serratus Anterior Plane (SAP) block:
Indications: Fracture ribs, ICD pain.
Technique: SAP block is performed by abducting the patients arm and the USG probe is placed at around 5th rib in coronal plane.22-24 The belly of latissimus dorsi (LD) is visualised followed by a muscle over the ribs which is serratus anterior muscle(SAM). Thoracodorsal artery can sometimes be identified in the fascial plane between LD and SAM. There are two approaches for the SAP- superficial and deep SAP block. In the superficial SAP, the LA is injected in this fascial plane between LD and SAM, whereas, in deep SAP, the LA is deposited under the SAM. The sonoanatomy shows hyperechoic ribs, SAM on the top and pleura further down (Figure 5).
- TAP block:
Indications: Fracture ribs, Laparotomies, Hermia repairs, Laparoscopic abdominal procedures, Obstetric surgery
Technique: For posterior TAP block, a high frequency linear probe or curvilinear probe in obese patients is placed at the midpoint of subcostal margin and iliac crest in mid-axillary line. The probe is moved to visualise 3 abdominal muscles: external oblique (EOM), internal oblique (IOM) and transversus abdominis (TAM) from superficial to deep (Figure 6). With an in-plane approach, a block needle is inserted from antero-medial to postero-lateral side till it reaches the fascial plane between IOM and TAM.25-27 After hydrodissection with saline to confirm the correct needle tip position, local anesthetic is injected after negative aspiration of blood. For a subcostal TAP block, the US probe is placed along the subcostal margin to identify rectus abdominis muscle (RAM).26 The probe is then moved laterally to identify TAM below RAM. The LA is injected in the fascial plane between these 2 muscles with the needle entering in-plane from medial to lateral side. Usually 15-20 ml of long acting LA is injected for analgesia. In recent times, many systematic reviews and meta-analysis on TAP block has been published and interested readers can are requested to read those papers.27-29
- Femoral Nerve Block:
Indications: fracture shaft femur, injuries at anterior aspect of thigh and knee
Technique: A linear array high frequency probe is placed transversely in groin just below the inguinal ligament and femoral vessels are identified. Femoral nerve is lateral to the vessels and deep to fascia iliaca (FI). It appears as a hyperechoic, oval or triangular structure (Figure 7). Usually 15-20 ml LA can be deposited around the nerve after negative aspiration. This is a simple and basic level block.30 The needle is usually inserted in-plane from lateral to medial. This block provides analgesia to anterior and medial aspect of thigh up to knee including hip fractures.
7, Fascia Iliaca Compartment Block (FICB):
Indications: Injuries to anterior thigh/ knee/ hip, and simple and complex hip fracture
Technique: This is a compartment block targeting all 3 nerves of the lumbar plexus, namely femoral (FN), obturator (ON) and lateral femoral cutaneous nerve (LFCN) of thigh just below the FI. Earlier description was the standard technique of doing it below the inguinal ligament in a transverse axis scanning approach. However, in recent times, the longitudinal supra-inguinal approach has been described in the literature which provides better analgesia for hip fracture or even hip arthroplasty patients.31 Below, we have described both the approaches.
Classic approach: A linear array high frequency probe is place transversely close to the femoral crease and then moved lateral to femoral artery. FI is identified above the oval or triangular shaped FN. More laterally, triangular shaped Sartorius muscle is identified on top. In a lateral to medial orientation, the needle is inserted in-plane to enter the plane between FI and iliopsoas muscle and deposit 30-40 ml LA which tends to spread cranially to cover the branches of the lumbar plexus. However, the blockade of ON, and LFCN is inconsistent and variable in this approach.
Supra-inguinal Longitudinal FICB: In this approach, high frequency linear probe is placed over anterior superior iliac spine (ASIS) in a longitudinal manner (Figure 8). Then the probe is moved medially till the typical “bow-tie pattern” is appreciated in the ultrasound. The iliacus muscle, with FI covering it is appreciated, and subsequently internal oblique and sartorius muscle as cephalad and caudad to the FI respectively. This forms a classic bow-tie appearance (Figure 9). Another sonographic finding is deep circumflex iliac artery (DCIA) lying just above the FI. The needle is inserted from caudad to cephalad to deposit the LA below FI in its supra-inguinal part (Figure 10). Similarly, around 40 ml of LA is deposited where LA is expected to spread proximally to block all 3 branches of lumbar plexus. While inserting the needle, care has to be taken to make sure that over zealous proximal insertion is avoided as bowel can be found further proximally beyond IOM.
Desmet et al. found sensory blockade in FN, ON, LFCN territory after 1 hour following surgery in 93%, 76%, and 95% patients respectively in the above described approach.31 Similarly, they found motor blockade in FN, and ON in 88% and 86% respectively. This appears better and promising than previously described classical approach.
- Brachial plexus block (BPB):
Indications: Trauma to upper limb, burns of upper limb.
Technique: Various approaches to BPB has been described, viz: interscalene (ISB), supraclavicular (SCB), infraclavicular (IC) and axillary approaches which blocks the plexus at the level of roots/trunk, trunks/division, cords and individual nerves respectively.
Interscalene Block (ISB): A high frequency linear probe is used and placed transversely over neck. The scanning can start beginning from above clavicle by identifying subclavian artery (SCA) or from midline at cricoid level. After identifying SCA, the probe is moved cranially to identify anterior scalene muscle (ASM) medially and middle scalene muscle (MSM) laterally. Similarly, from cricoid level, the probe is moved laterally, and the same muscles can be easily identified.
The roots of C5,6 and C7 can be identified sandwiched between these muscles arranged in what is described as a traffic light (Figure 11). The needle is inserted in-plane from lateral to medial targeting the area just next to brachial plexus, which is popularly known as peri-plexus approach.32, 33 Care should be taken avoid injuring other small nerves like dorsal scapular and long thoracic nerve passing through MSM.34
Supraclavicular (SCB): In supraclavicular approach, the trunks and/or divisions can be identified as a characteristic bunch of grapes appearance anterolateral to SCA (Figure 12). The block needle is inserted in-plane from lateral to medial targeting corner pocket first for lower trunk and then needle is redirected to finish the block.35
The cords of brachial plexus can be blocked by IC approach which is by placing the transducer medial to coracoid process just below the clavicle with the arm abducted and face turned to other side. The axillary vessels are identified. The cords: lateral, medial and posterior are identified here in same relation to the axillary artery and LA is injected after negative aspiration of blood.
Axillary block: With the extremity in the same position as described for ICB, the probe is positioned in short axis orientation and axillary artery is identified.36 The median, radial and ulnar nerves are identified as hypoechoic round-to-oval structures at 11-12 o’clock, 5-6 o’clock, and 1-2 o’clock to axillary artery respectively (Figure 13). A separate injection is required around musculocutaneus nerve which is a bright, hyperechoic flat structure located between coracobrachialis and biceps muscle.
CONCLUSION
Providing pain relief to patients admitted in ICU is of paramount importance. RA techniques when utilized in ICU patients reduce surgical and trauma stress response. It facilitates faster weaning from ventilation and reduces morbidity. RA techniques are under-utilised for managing pain in ICU setting because of poor training and perceived myths about risks among ICU physicians. Pain relief makes patients’ more comfortable, reduces use of opioids and other drugs which can have negative impact on other organs. Once adequate analgesia is provided using RA techniques, the patient can sleep well, perform chest physiotherapy and incentive spirometry adequately, thus can recover faster. With the increasing use of US in performing PNB, the blocks have not only become safer but have become very effective with lesser volume of drug. Anesthesiologist ICU physicians should take the lead and make these RA techniques popular and better utilized in ICU setting.
Conflict of interest: Nil
Authors’ contribution: All authors took equal part in preparation of this manuscript
REFERENCES
- Gelinas C, Johnston C. Pain assessment in the critically ill ventilated adult: Validation of the critical care pain observation tool and physiologic indicators. Clin J Pain. 2007;23(6):497–505. DOI: 10.1097/AJP.0b013e31806a23fb [PubMed]
- Dolin SJ, Cashman JN, Bland JM. Effectiveness of acute postoperative pain management: I. Evidence from published data. Br J Anaesth. 2002;89(3):409–23. [PubMed]
- Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003;97(2):534–40. DOI: 10.1213/01.ANE.0000068822.10113.9E [PubMed]
- Puntillo KA, White C, Morris AB, Perdue ST, Stanik-Hutt J, Thompson CL, et al. Patients’ perceptions and responses to procedural pain: results from Thunder Project II. Am J Crit Care. 2001;10(4):238–51. [PubMed]
- Capdevila M, Ramin S, Capdevila X. Regional anaesthesia and analgesia after surgery in ICU. Curr Opin Crit Care. 2017;23(5):430–9. DOI: 10.1097/MCC.0000000000000440 [PubMed]
- Schulz-Stübner S, Boezaart A, Hata JS. Regional analgesia in the critically ill. Crit Care Med.2005;33(6):1400-7. [PubMed]
- De Pinto M, Dagal A, O’Donnell B, Stogicza A, Chiu S, Edwards WT. Regional anaesthesia for management of acute pain in the intensive care unit. Int J Crit Illn Inj Sci. 2015;5(3):138–143. DOI: 10.4103/2229-5151.164917 [PubMed]
- Baumbach P, Gotz T, Gunther A, Weiss T, Meissner W. Prevalence and characteristics of chronic intensive care-related pain: the role of severe sepsis and septic shock. Crit Care Med. 2016;44(6):1129–37. DOI: 10.1097/CCM.0000000000001635 [PubMed]
- Fletcher D, Stamer UM, Pogatzki-Zahn E, Zaslansky R, Tanase NV, Perruchoud C, et al. Chronic postsurgical pain in Europe: an observational study. Eur J Anaesthesiol. 2015;32(10):725-34. DOI: 10.1097/EJA.0000000000000319 [PubMed]
- Gerbershagen HJ, Pogatzki-Zahn E, Aduckathil S, Peelen LM, Kappen TH, van Wijck AJ, et al. Procedure-specific risk factor analysis for the development of severe postoperative pain. Anesthesiology. 2014;120(5):1237–45. DOI: 10.1097/ALN.0000000000000108 [PubMed]
- Montes A, Roca G, Sabate S, Lao JI, Navarro A, Cantillo J, et al. Genetic and clinical factors associated with chronic postsurgical pain after hernia repair, hysterectomy, and thoracotomy: a two-year multicenter cohort study. Anesthesiology. 2015;122(5):1123–41. DOI: 10.1097/ALN.0000000000000611 [PubMed]
- Kampe S, Geismann B, Weinreich G, Stamatis G, Ebmeyer U, Gerbershagen HJ. The influence of type of anaesthesia, perioperative pain, and preoperative health status on chronic pain six months after thoracotomy-a prospective cohort study. Pain Med.2017;18(11):2208-13. DOI: 10.1093/pm/pnw230 [PubMed]
- Po¨pping DM, Elia N, Van Aken HK, Marret E, Schug SA, Kranke P, et al. Impact of epidural analgesia on mortality and morbidity after surgery: systematic review and meta-analysis of randomized controlled trials. Ann Surg. 2014;259(6:1056–67. DOI: 10.1097/SLA.0000000000000237 [PubMed]
- Khoronenko V, Baskakov D, Leone M, Malanova A, Ryabov A, Pikin O, et al. Influence of regional anaesthesia on the rate of chronic postthoracotomy pain syndrome in lung cancer patients. Ann Thorac Cardiovasc Surg. 2018;24(4):180-6. DOI: 10.5761/atcs.oa.18-00044 [PubMed]
- Horlocker TT, Vandermeuelen E, Kopp SL, Gogarten W, Leffert LR, Benzon HT. Regional anaesthesia in the patient receiving antithrombotic or thrombolytic therapy: American Society of Regional Anaesthesia and Pain Medicine Evidence-Based Guidelines (Fourth Edition). Reg Anesth Pain Med.2018;43(3):263-309. DOI: 10.1097/AAP.0000000000000763 [PubMed]
- Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med.2016;41(5):621-7. DOI: 10.1097/AAP.0000000000000451 [PubMed]
- Adhikary SD, Pruett A, Forero M, Thiruvenkatarajan V. Erector spinae plane block as an alternative to epidural analgesia for post-operative analgesia following video-assisted thoracoscopic surgery: A case study and a literature review on the spread of local anaesthetic in the erector spinae plane. Indian J Anaesth. 2018;62(1):75-8. DOI: 10.4103/ija.IJA_693_17 [PubMed]
- Singh S, Chowdhary NK. Erector spinae plane block an effective block for post-operative analgesia in modified radical mastectomy. Indian J Anaesth. 2018;62(2):148-50. DOI: 10.4103/ija.IJA_726_17 [PubMed]
- Nair AS, Seelam S, Naik V, Rayani BK. Opioid-free mastectomy in combination with ultrasound-guided erector spinae block: A series of five cases. Indian J Anaesth. 2018 Aug;62(8):632-4. DOI: 10.4103/ija.IJA_314_18 [PubMed]
- Chin KJ, Malhas L, Perlas A. The erector spinae plane block provides visceral abdominal analgesia in bariatric surgery: a report of 3 cases. Reg Anesth Pain Med. 2017;4(3)2:372–6. DOI: 10.1097/AAP.0000000000000581 [PubMed]
- Peng PW, Narouze S. Ultrasound-guided interventional procedures in pain medicine: a review of anatomy, sonoanatomy, and procedures: part I: nonaxial structures. Reg Anesth Pain Med.2009;34(5):458-74. DOI: 10.1097/AAP.0b013e3181aea16f [PubMed]
- Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013;68(11):1107-13. DOI: 10.1111/anae.12344 [PubMed]
- Madabushi R, Tewari S, Gautam SK, Agarwal A, Agarwal A. Serratus anterior plane block: a new analgesic technique for post-thoracotomy pain. Pain Physician. 2015;18(3):E421-4. [PubMed] [Free Full Text]
- Daga V, Narayanan M, Dedhia J, Gaur P, Crick H, Gaur A. Cadaveric feasibility study on the use of ultrasound contrast to assess spread of injectate in the serratus anterior muscle plane. Saudi J Anaesth. 2016;10(2):198-201. DOI: 10.4103/1658-354X.168825 [PubMed]
- Finnerty O, Carney J, McDonnell JG. Trunk blocks for abdominal surgery. Anaesthesia. 2010;65 Suppl 1:76-83. DOI: 10.1111/j.1365-2044.2009.06203.x [PubMed]
- Ma J, Jiang Y, Tang S, Wang B, Lian Q, Xie Z, et al. Analgesic efficacy of ultrasound-guided subcostal transversus abdominis plane block. Medicine (Baltimore). 2017;96(10):e6309. DOI: 10.1097/MD.0000000000006309 [PubMed]
- Tsai H-C, Yoshida T, Chuang TY, Yang SF, Chang CC, Yao HY, et al. Transversus abdominis plane block: an updated review of anatomy and techniques. Biomed Res Int. 2017;2017:8284363. DOI: 10.1155/2017/8284363 [PubMed]
- Baeriswyl M, Kirkham KR, Kern C, Albrecht E. The Analgesic efficacy of ultrasound-guided transversus abdominis plane block in adult patients: a meta-analysis. Anesth Analg. 2015;121(6):1640-54. DOI: 10.1213/ANE.0000000000000967 [PubMed]
- Ma N, Duncan JK, Scarfe AJ, Schuhmann S, Cameron AL. Clinical safety and effectiveness of transversus abdominis plane (TAP) block in post-operative analgesia: a systematic review and meta-analysis. J Anesth. 2017;31(3):432-52. DOI: 10.1007/s00540-017-2323-5 [PubMed]
- Bhoi S, Sinha TP, Rodha M, Bhasin A, Ramchandani R, Galwankar S. Feasibility and safety of ultrasound-guided nerve block for management of limb injuries by emergency care physicians. J Emerg Trauma Shock. 2012;5(1):28-32. DOI: 10.4103/0974-2700.93107 [PubMed]
- Desmet M, Vermeylen K, Van Herreweghe I, Carlier L, Soetens F, Lambrecht S, et al. a longitudinal supra-inguinal fascia iliaca compartment block reduces morphine consumption after total hip arthroplasty. Reg Anesth Pain Med. 2017; 42(3):327-33. DOI: 10.1097/AAP.0000000000000543 [PubMed]
- Spence BC, Beach ML, Gallagher JD, Sites BD. Ultrasound-guided interscalene blocks: understanding where to inject the local anaesthetic. Anaesthesia.2011;66(6):509-14. DOI: 10.1111/j.1365-2044.2011.06712.x [PubMed]
- Chen HP, Shen SJ, Tsai HI, Kao SC, Yu HP. Effects of interscalene nerve block for postoperative pain management in patients after shoulder surgery. Biomed Res Intl. 2015;2015:902745. DOI: 10.1155/2015/902745 [PubMed]
- Hanson NA, Auyong DB. Systematic ultrasound identification of the dorsal scapular and long thoracic nerves during interscalene block. Reg Anesth Pain Med.2013;38(1):54-7. DOI: 10.1097/AAP.0b013e31826f0a63 [PubMed]
- Vermeylen K, Engelen S, Sermeus L, Soetens F, Van de Velde M. Supraclavicular brachial plexus blocks: review and current practice. Acta Anaesthesiol Belg. 2012;63(1):15-21. [PubMed]
- Satapathy AR, Coventry DM. Axillary brachial plexus block. Anesthesiol Res Pract. 2011;2011:173796. DOI: 10.1155/2011/173796 [PubMed]
Figure legends:
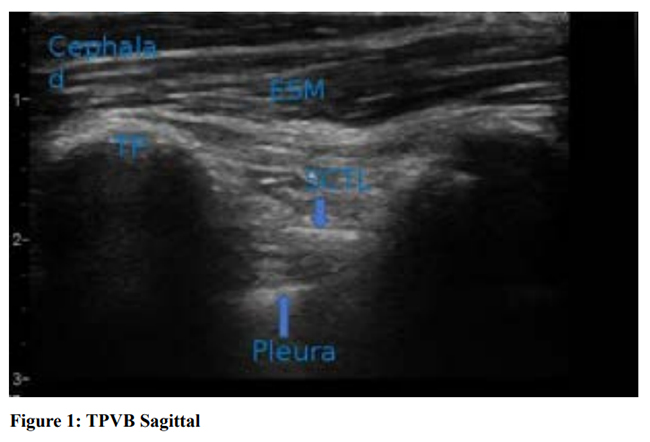
Figure 1: Sagittal approach to Thoracic paravertebral block (TPVB).
Sonoanatomy of TPV region showing the hyperechoic transverse process, muscle and ligament.
Needle entry- craniocaudal or caudocranial. Drug is injected after piercing the SCTL which pushes the pleura down.
TP – transverse process, ESM- erector spinae muscle, SCTL- superior costo-transverse ligament.
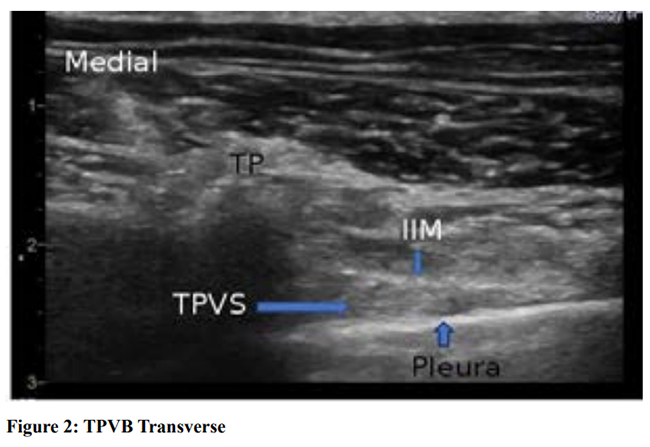
Figure 2: Transverse approach to thoracic paravertebral block.
Sonoanatomy of TPV region in transverse scanning showing the hyperechoic pleura, and apex of TPV space (TPVS).
Needle entry- lateral to medial. Drug is deposited after piercing the IIM (internal intercostal membrane)

Figure 3: Erector spinae plane (ESP) block.
Sonoanatomy for ESP block showing the hyperechoic transverse process, and muscle (ESM) on top.
Needle entry- craniocaudal in-plane. ESM- erector spinae muscle.
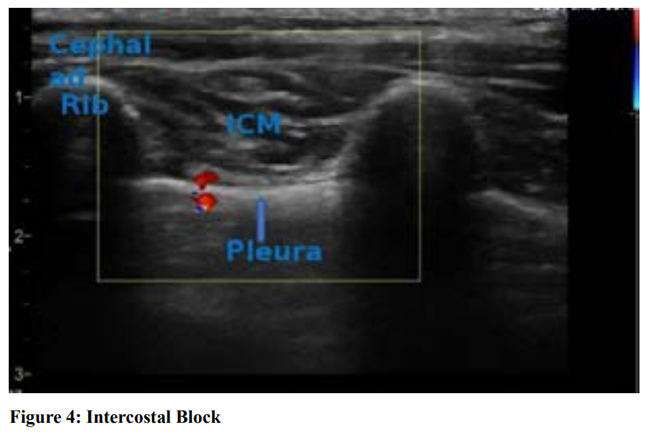
Figure 4: Intercostal block (ICB)
Sonoanatomy of IC region showing the hyperechoic ribs, muscles, blood vessel and pleura. Note the difference in appearance of rib from TP as shown in Figure 3 for ESP block.
ICM- intercostal muscles, red dots- intercostal vessels.
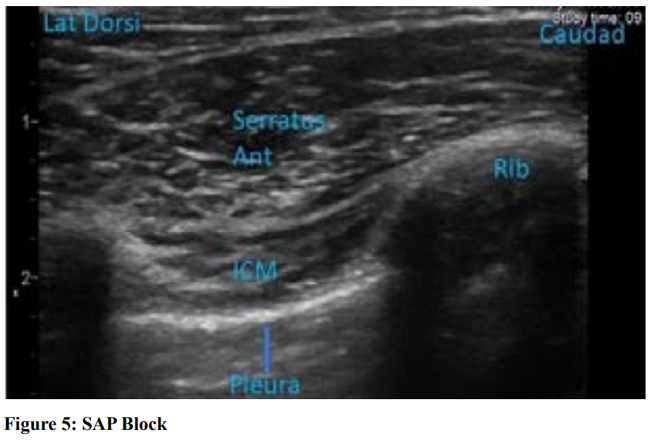
Figure 5: Serratus Anterior Plane (SAP) block.
Sonoanatomy shows hyperechoic ribs with typical acoustic shadow, pleura further deep to the intercostal muscles (ICM). Block needle is inserted in-plane from caudad to cephalad targeting the plane between serratus anterior muscle (SAM) and latissimus dorsi muscle (LDM) or below SAM.
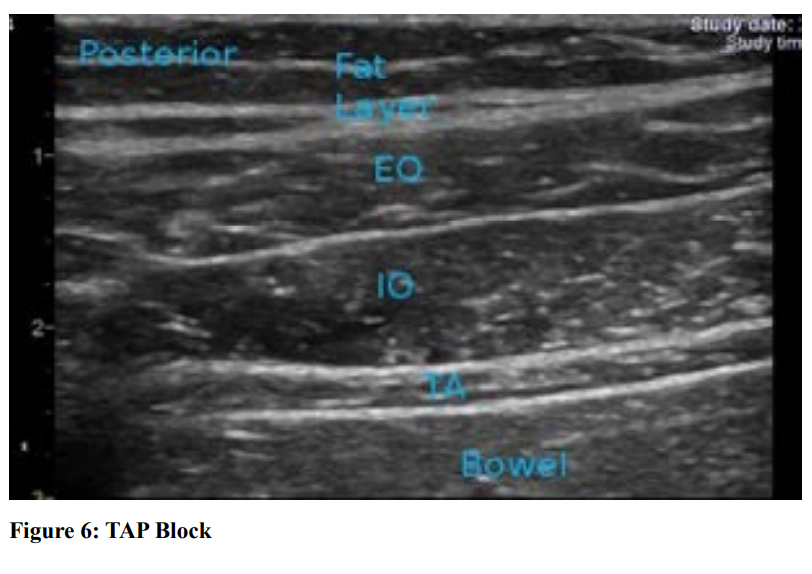
Figure 6: Transversus Abdominis Plane (TAP) block
Sonoanatomy of TAP region showing three muscle layers of abdominal wall and bowel further deep. It is always recommended to count the muscle layers from deep, and IO muscle is thickest of all three.
EO-external oblique muscle, IO-internal oblique muscle, TA-transversus abdominis muscle
Needle entry-medial to lateral, in-plane with probe placed between midpoint of subcostal margin and ASIS. LA is injected in the fascial plane between IO and TA.
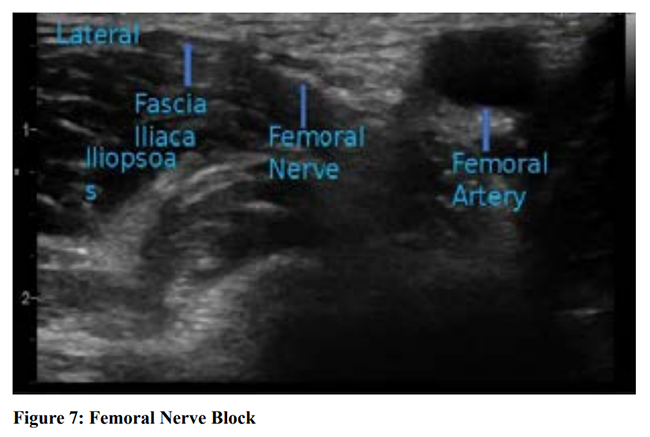
Figure 7: Femoral nerve block.
Sonoanatomy of groin region below the inguinal ligament showing the hyperechoic femoral nerve just below fascia iliaca and on top of the iliacus muscle.
Probe placement- transversely in inguinal region and identify femoral vessels.
Needle entry- lateral to medial, in-plane.

Figure 8: Probe placement for supra-inguinal longitudinal FICB (Fascia Iliaca Compartment Block)
Probe is placed just medial to ASIS (anterior superior iliac spine) to capture a typical bow-tie appearance in Ultrasound.
Needle entry- Caudad to cephalad
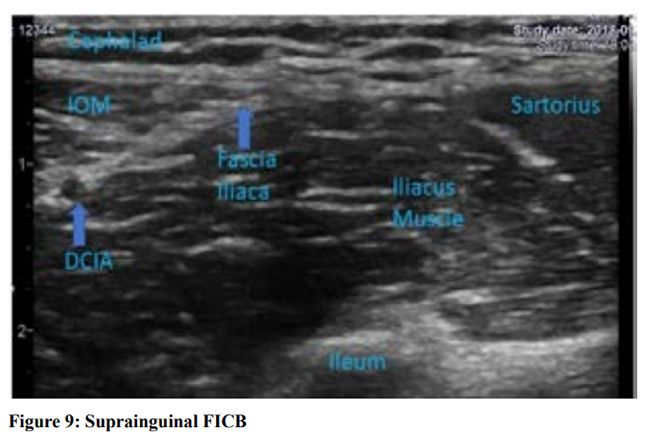
Figure 9: Sonoanatomy of supra-inguinal longitudinal FICB
Typical bow-tie appearance by internal oblique muscle cephalad (IOM) and sartorius muscle caudad. The fascia iliaca (FI) is clearly seen as a hyperechoic continuous line just above the iliacus muscle. Cephalad the deep circumflex iliac artery (DCIA) is usually seen just above the FI.
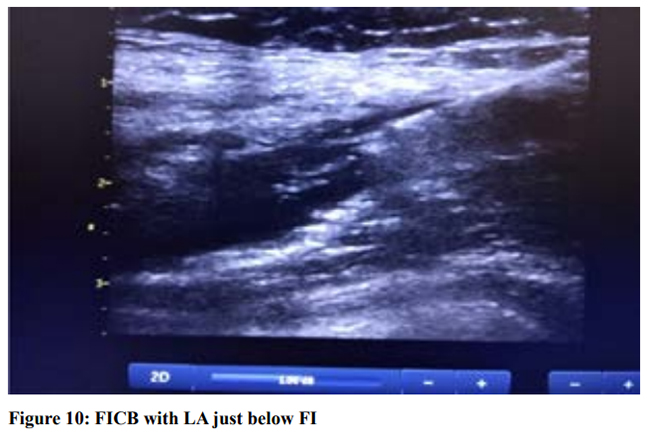
Figure 10: Suprainguinal longitudinal FICB block. Local anaesthetic can be seen deposited below fascia iliaca (FI) and iliacus muscle getting pushed down. The block needle is clearly visible here.
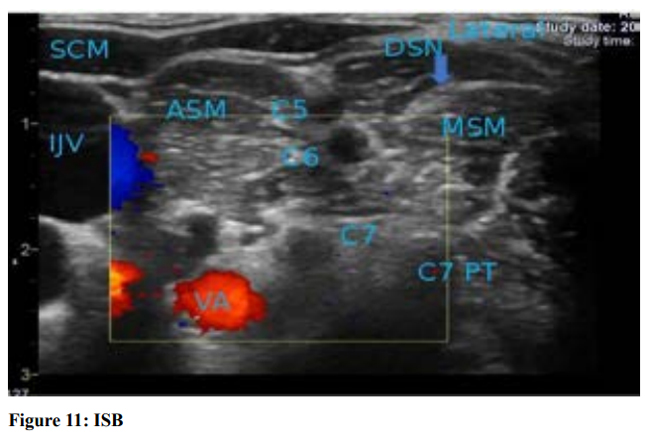
Figure 11: Interscalene block (ISB)
Sonoanatomy of IS region showing the so-called traffic light sign of the nerve roots sand witched between two scalene muscles. Also seen are vertebral vessels, and IJV and carotid artery.
SCM- sternocleidomastoid muscle, IJV-internal jugular vein,
ASM- anterior scalene muscle, MSM-middle scalene muscle, DSN-dorsal scapular nerve, PT- posterior tubercle.
C5, C6, C7- roots of brachial plexus. Needle entry-lateral to medial, in-plane.
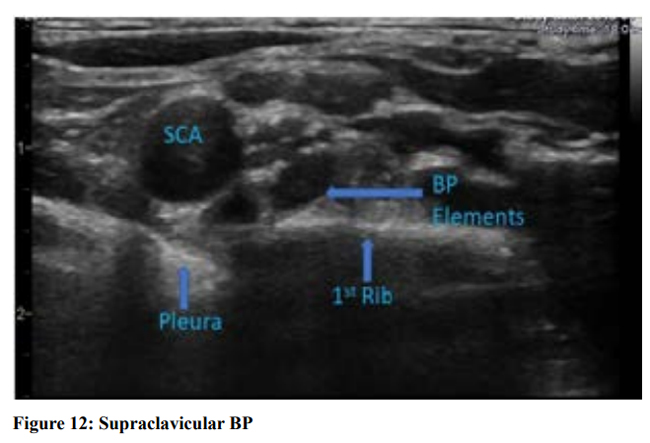
Figure 12: Supraclavicular block (SCB)
Sonoanatomy of SC region showing the so-called bunch of grapes appearance of brachial plexus (BP) elements postero-lateral to subclavian artery (SCA).
SCA- subclavian artery, BP- brachial plexus elements
Needle entry- lateral to medial, in-plane,
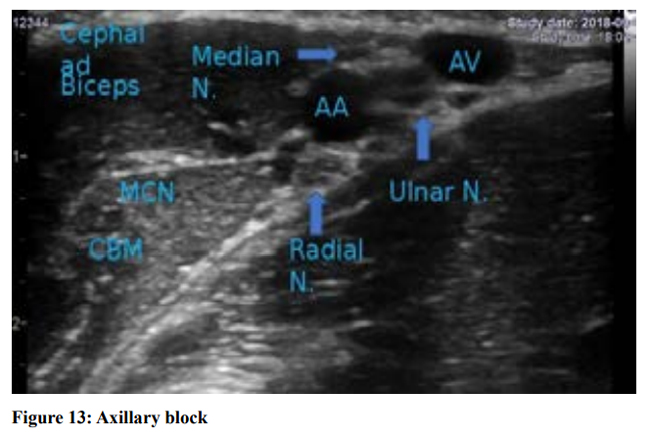
Figure 13: Axillary block.
Sonoanatomy of the axillary region showing the blood vessels and typical arrangement of peripheral nerves of the brachial plexus.
MCN- musculocutaneous nerve, CBN- coracobrachialis muscle, AA- axillary artery, AV- axillary vein.

