Lakesh K. Anand, MD, FIMSA, FCCP, MAMS, FCCS1, Rashi Sarna, MD2, Sukanya Mitra, MD, MAMS3
1Professor, Department of Anesthesia & Intensive Care, Government Medical College & Hospital, Sector 32, Chandigarh, (India)
2Assistant Professor, Department of Anesthesia, Adesh Medical College & Hospital, Ambala Cant, Haryana (India)
Correspondence: Professor Lakesh K. Anand, Department of Anesthesia & Intensive Care, Government Medical College & Hospital, Sector 32, Chandigarh 160030, (India)
ABSTRACT
Objective: Ropivacaine has been claimed to be superior for epidural labor analgesia, with less motor blockade and toxicity as compared to bupivacaine, and it has largely replaced the later drug for this purpose.
The objective of this study was to compare and evaluate the analgesic efficacy of ropivacaine 0.1% and bupivacaine 0.1% with 2 μg/ml fentanyl for painless labor using patient-controlled epidural analgesia (PCEA).
Methodology: This prospective, randomized and double blind study was undertaken in a tertiary care hospital. Fifty parturients of ASA grade I and II, were randomly allocated into two groups of 25 each, to receive either 10 ml of 0.1% bupivacaine or 0.1% ropivacaine with fentanyl 2μg/ml in Group B and Group R respectively as initial bolus dose. Same dose regimen was used as continuous background infusion and PCEA boluses of 10 ml according to the group allocation. Onset and quality of analgesia, motor weakness, total drug consumption, and fetomaternal outcome in both groups were compared.
Results: Effective labor analgesia (VAS < 30) with onset time of 9.42 ± 1.16 and 9.14 ± 1.46 min in Group B and Group R respectively were comparable in both the groups (p > 0.05). All the patients were pain free within 15 min after initiation of epidural analgesia. Sensory and motor block characteristics in both the groups were comparable. No patient had motor blockade till two hours after initiation of epidural analgesia. Motor block increased as the duration of labor increased. Overall, drug consumption was 85.04 ± 21.02 ml in Group R and 81.56 ± 22.81 ml in Group B with fentanyl during labor (p > 0.05). There were no significant changes in hemodynamic parameters, duration of labor or maternal satisfaction. No adverse effects related to neonatal or maternal outcomes were noted in both groups.
Conclusion: We conclude that 0.1% ropivacaine or 0.1% bupivacaine, with fentanyl 2 μg/ml using PCEA, were equally effective for labor analgesia. There were no statistically significant differences in the quantity of drug used, motor weakness, labor duration, or fetomaternal outcome.
Key words: Labor analgesia; Bupivacaine; Ropivacaine; Fentanyl; Patient-controlled epidural analgesia
Citation: Anand LK, Sarna R, Mitra S. A comparison of 0.1% ropivacaine and 0.1% bupivacaine plus fentanyl with patient-controlled epidural analgesia for labor: a double blind study. Anaesth Pain & Intensive Care 2016;20(3):278-284
Received: 10 March 2016; Reviewed: 11 April & 22 June 2016; Corrected: 28 March & 20 August; Accepted: 31 August 2016
INTRODUCTION
The pain of childbirth is the most painful experience for many women and maternal request is sufficient justification for pain relief during labor.1 Unrelieved labor pain result in maternal stress response, which is neither beneficial for the fetus nor the mother.2 Patient-controlled epidural analgesia (PCEA) is a reliable and effective method for maintaining labor analgesia.3
Bupivacaine is an amide local anesthetic (LA) commonly used for epidural analgesia in obstetric practice.4 Its disadvantages include the potential for motor blockage and cardiovascular toxicity. These concerns have motivated the search for alternative agents. Ropivacaine, an amide LA agent with pharmacological properties similar to bupivacaine has less motor blockade and reduced incidence of toxic effects.5,6
Although studies have suggested that ropivacaine is approximately 40% less potent than bupivacaine,7,8 clinical studies comparing low concentrations of ropivacaine and bupivacaine with or without opioids for labor analgesia suggest the two drugs are equipotent in terms of sensory blockade for labor analgesia.9-11 There are still very limited reports comparing 0.1 % ropivacaine and bupivacaine with fentanyl for labor analgesia by PCEA. Thus, we evaluated and compared the analgesic efficacy of 0.1 % ropivacaine and bupivacaine, with 2 μg /ml fentanyl in epidural labor analgesia using PCEA.
METHODOLOGY
After the approval by the Institutional Ethics Committee (IEC), informed consent was obtained from 50 healthy parturients of American Society of Anesthesiologists (ASA) physical status II to undergo study. We selected ladies with cephalic presentation at ≥ 36 weeks of gestation in early spontaneous labor, with cervical dilation ≤ 5 cm, requesting epidural analgesia for labor to be enrolled for the study.
Participants were excluded if they had any contraindication to epidural analgesia, allergy to study drugs, having twin pregnancy or malpresentation, bleeding disorders, sepsis, or having received parenteral opioids in the last 4 hours.
The study design was prospective, randomized and double blind. Using computer generated random number table patients were randomly allocated to either 0.1% bupivacaine plus 2 μg/ml fentanyl Group B (n=25) or 0.1% ropivacaine plus 2 μg/ml fentanyl Group R (n=25). Allocation concealment was done using sequentially numbered coded sealed envelopes.
For Group B, 50 ml of 0.1% bupivacaine plus 2 μg/ml of fentanyl were prepared by taking 10 ml of 0.5% isobaric bupivacaine and 100 μg fentanyl (2 ml) and diluting with 38 ml of 0.9% normal saline. For Group R, 0.1% ropivacaine was used instead of bupivacaine in similar manner and 50 ml solution was prepared. To ensure double blinding, different anesthesiologists were involved for preparing, administering the study drugs, and recording the data.
Preanesthetic evaluation was done and technique of epidural analgesia was explained to the patients. Before placement of the epidural catheter, visual analog scale (VAS) score was noted with VAS 0 = no pain and 100 = the worst imaginable pain.
For insertion of the epidural catheter the patient was taken to the clean labor room (CLR). Standard monitoring was started and baseline heart rate (HR), non-invasive blood pressure (NIBP) and oxygen saturation (SpO2) were recorded. An infusion of Ringers lactate solution was started through 18G peripheral intravenous (IV) cannula; the parturient was made to sit on the operating table. Following strict aseptic techniques, epidural space was identified at L2-3 or L3-4 interspace, lignocaine 2% was infiltrated; then using a loss of resistance technique to normal saline with an 18G Tuohy needle and a catheter was threaded through to a depth of 4-5 cm into the epidural space. A loading dose of 10 ml of bupivacaine 0.1% with fentanyl 2 μg/ml or ropivacaine 0.1% with fentanyl 2 μg/ml was administered through the catheter. The presence of clinical signs of an IV injection were sought, for the following 2-3 min by asking the patient whether she felt dizzy, had tinnitus, or a metallic taste in her mouth. If there were no signs of an IV injection, the epidural catheter was secured and the parturient was placed in the supine position with left lateral tilt. Five minutes after the initial dose, if there were no clinical signs of subarachnoid injection (as evidenced by the patient’s ability to move her legs and the absence of hypotension), maintenance of PCEA (Master™ PCA pump, Fresenius Kabi) was started with either bupivacaine or ropivacaine solutions as a continuous background infusion according to the group allocation. The patients were given a remote controlled hand-held button with a provision of patient controlled boluses of 10 ml of the same drug with a lockout interval of 15 minutes if needed (VAS > 30) through the second stage of labor.
Analgesia was considered adequate if VAS score was ≤ 30. Onset of analgesia was defined as time of first bolus dose to time of achieving VAS ≤ 30. The patients were observed for 20 min and monitored continuously (HR, NIBP, and SpO2). Pain score (VAS), level of sensory block, and modified Bromage scale12 for motor power in lower extremities before shifting the patient to CLR for monitoring of the mother and fetus during the course of labor.
Hypotension was defined as systolic blood pressure (SBP) of < 90 mmHg and was treated with boluses of 6 mg ephedrine. Bradycardia was defined as heart rate <60 bpm and was treated with bolus doses of 0.4 mg atropine.
Demographic data (age, weight, height, ASA grade), obstetric data (parity, dilatation of the cervix) were noted prior to the initiation of labor analgesia. Pain scores (VAS), sensory and motor block characteristics and hemodynamic parameters (HR, SBP) were recorded at 0 hr (before epidural), every 5 min for the first 20 min and then every 1 h till delivery. Sensory block height was assessed at midline by loss of sensation to pin prick (blunt head of a pin).
Labor was managed according to our obstetric department’s protocols. Complete dilatation of cervix (time from first initial epidural dose until the full dilatation of cervix), mode of delivery (normal/ instrumental /cesarean delivery), injection to delivery time (time from first initial epidural dose until the delivery) and total epidural drug used was noted. Fetal heart rate was monitored throughout the study by using a cardiotocograph, and any changes, e.g. decelerations was recorded. Neonatal assessment was performed by assessing the Apgar score at 1 and 5 min.
Side-effects including nausea, vomiting, hypotension, hypersensitive reaction, shivering, drowsiness, pruritus, respiratory depression and retention of urine were noted. Overall maternal satisfaction scores with labor analgesia (VAS, based on a 0-100 scale, 0 = very dissatisfied, 100 = extremely satisfied) were also assessed and recorded.
We calculate that a sample size of 23 patients in each group would have 82% power at 5% significant level to detect a difference in VAS score of 8 among groups based on a pilot and previous study.9 To allow the potential drop-out, we decided to recruit a total of 25 patients per group.
The statistical analysis was carried out using Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, version 15.0 for Windows). All quantitative variables were estimated using measures of central location (mean, median) and measures of dispersion (standard deviation). Normality of data was checked by measures of Kolmogorov Smirnov tests of normality. For normally distributed data means were compared using student’s t-test for two groups. For skewed data or for scores (for VAS score, motor power) Mann–Whitney test was applied. Proportions were compared using Chi square or Fisher’s exact test whichever was applicable. Onset time was evaluated using Kaplan Meier survival curve and log rank test. For time related variables Two-Way ANOVA was applied. One-Way ANOVA was applied for within group comparison. For scores Friedman test followed by Wilcoxon Signed Rank test was applied. All statistical tests were two-sided and performed at a significance level of α=.05
RESULTS
Sixty patients were enrolled to the study. Ten patients were not randomised, leaving 50 patients (25 per group) included in the data analysis see the consort diagram (Figure 1).
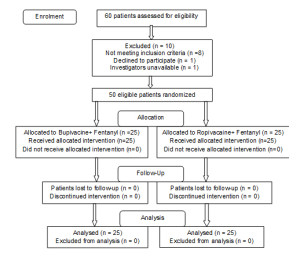
Figure 1: Consort diagram
Demographic data, obstetric data and injection to full cervical dilatation and till delivery time were comparable in both groups, (p > 0.05) (Table 1).
Table 1: Demographic and obstetric parameters mean ± SD
| Variables | Group B
(Bupivacaine + Fentanyl) (n=25) |
Group R
(Ropivacaine + Fentanyl) (n=25) |
p-value |
| Age (years) | 26.04 ± 3.88 | 26.76 ± 3.23 | 0.47 |
| Height (cm) | 160.00 ± 5.63 | 160.40 ± 5.32 | 0.79 |
| Weight (kg) | 61.96 ± 4.11 | 61.80 ± 4.29 | 0.89 |
| ASA I/II (%) | 18(72)/ 7(28) | 18(72)/ 7(28) | |
| Parity
· Primiparous (%) · Multiparous (%) |
20 (84) 4 (16) |
22 (88) 3 (12) |
|
| Dilatation of cervix (cm) | 3.28 ± 0.61 | 3.34 ± 0.54 | 0.73 |
| Injection to complete dilatation of cervix (min) | 78.32 ± 35.78 | 69.43 ± 31.08 | 0.37 |
| ٭Duration of labor (hr) | 5.16 ± 1.67 | 5.32 ± 1.57 | 0.28 |
٭Injection to delivery time
Before initiation of epidural analgesia mean VAS score was 82.80 ± 6.63 in Group B and 84.80 ± 6.99 in Group R (p > 0.05) [Figure 2]. Both the solutions of 0.1% bupivacaine and ropivacaine with fentanyl 2 μg/ml in Group B and Group R respectively produced effective analgesia (defined by VAS < 30) after initial loading dose in parturient of both the groups, stating no failure rate. Onset time of analgesia was 9.42 ± 1.16 and 9.14 ± 1.46 min in Group B and Group R respectively were comparable in both the groups (p > 0.05). All the patients were pain free within 15 minutes after initiation of epidural analgesia (Table 2).
Table 2: Total drug requirement, onset time, sensory level and maternal satisfaction
| Parameters | Group B | Group R | p-value |
| Local Anesthetic (ml) | 81.56 ± 22.81 | 85.04 ± 21.02 | 0.57 |
| Fentanyl | 163.12 ± 43.68 | 170.08 ± 42.04 | 0.37 |
| ٭PCEA demand bolus | 2.40 ± 0.816 | 2.64 ± 0.746 | 0.13 |
| Onset time (min) | 9.420 ± 1.1698 | 9.140 ± 1.4614 | 0.38 |
| Sensory level | T9 (T8-T10) | T9 (T8-T10) | |
| Maternal satisfaction (VAS) | 80.40 ± 7.75 | 82.08 ± 6.55 | 0.39 |
٭PCEA= patient-controlled epidural analgesia
All the parturient in both the groups attained a sensory blocked level up to T9 (T8-T10) and none of the patient in both the groups showed a sensory block higher than T8. Motor block characteristics in both the groups were comparable. No patient had motor blockade till two hours after initiation of epidural analgesia. Three (12%) patients in the Group B and two (8%) patients in the Group R had Bromage score of 2; one patient in Group B had a score of 3. We found that the incidence of motor block increased as the duration of labor increased.
There were no differences between groups in the amounts of LA used for labor analgesia. Overall, LA combination used was 85.04 ± 21.02 ml in Group R and 81.56 ± 22.81 ml in Group B with fentanyl during labor (p > 0.05). Total PCEA demands and delivered doses were also comparable between groups (Table 2).
Hemodynamic (HR, NIBP) status of parturient in both the groups was comparable. None of the patient in any group required either ephedrine or atropine (Figure 3a, b and c).
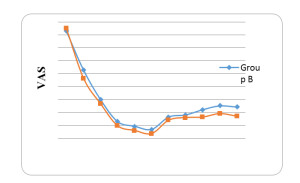
Figure 2: The visual analog score (VAS) for pain
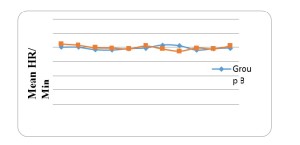
Figure 3: The variation in heart rates of the two groups
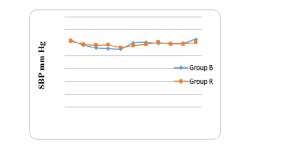
Figure 3b. The hemodynamic parameters: The variation in SBP
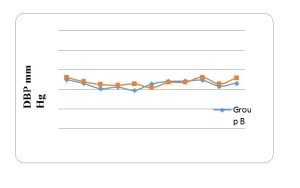
Figure 3c. The hemodynamic parameters: The variation in DBP
| MOD | Group B
N (%) |
Group R
N (%) |
| Vaginal N (%) | 20 (80) | 22 (88) |
| Forceps N (%) | 2 (8) | 1 (4) |
| LSCS N (%) | 3 (12) | 2 (8) |
| Causes of LSCS
· Fetal distress · Nonprogress |
2 (8) 1 (4) |
1 (4) 1 (4) |
Table 3: Comparison of mode of deliveries (MOD)
Spontaneous vaginal delivery occurred in 92% parturient in Group R and 88% in Group B, one parturient in Group R and two parturient in Group B had forceps delivery. Two parturient in Group R and three parturient in Group B had cesarean delivery (Table 3). Neonatal outcome was favorable in both the groups (Apgar scores > 7 at 1 and 5 min) with no side effects.
The overall mean maternal satisfaction VAS score was 80.40 ± 7.75 and 82.08 ± 6.55 in Group B and Group R respectively (p > 0.05). No patient complained of pruritus, shivering, nausea vomiting and urinary retention in either of the two groups.
DISCUSSION
The results of our study demonstrated that 0.1% bupivacaine or ropivacaine combined with fentanyl 2 μg/ml were provide adequate pain relief during labor in all the parturient. All the parturient remain hemodynamically stable; no one had motor weakness till two hours after initial bolus dose; spontaneous vaginal delivery occurred in 92% and 88% in Group R and Group B patients respectively; and neonatal outcome was favorable in both the groups. We did not find any significant differences with respect to drug consumption.
There are controversial data regarding minimum local analgesic concentration (MLAC) of bupivacaine and ropivacaine for epidural labor analgesia. Previous studies estimating relative analgesic potencies of ropivacaine and bupivacaine for epidural analgesia in labor, however, suggest that ropivacaine is 40% less potent than bupivacaine for initiating labor analgesia, and that this difference may account for the decreased toxicity and motor block when equal drug concentrations are compared.9,10 If it is so, then at equally potent doses, ropivacaine may have similar toxicity and motor block to bupivacaine. If ropivacaine is less potent than bupivacaine for the maintenance of labor analgesia, then a larger concentration or a larger volume of ropivacaine should be required to produce a similar degree of labor analgesia assuming parallel dose-response curves for ropivacaine and bupivacaine.
Several clinical studies have compared the bupivacaine and ropivacaine in equal concentration and volume with and without opioid showed similar efficacy,9,13-15 and also supported by a multicenter, randomized, controlled trial.16
Meister et al9 compared 0.125% bupivacaine or ropivacaine with 2 μg/ml fentanyl and same concentration of bupivacaine or ropivacaine without fentanyl by Owenet al13 using the PCEA technique found no significant differences in the consumption of LA required to produce analgesia. The 0.125% concentration of bupivacaine and ropivacaine being at the upper end of the dose-response curve may potentially mask the potency differences between drugs. The present study was designed in an attempt to put off this problem by using a LA concentration (0.1%) nearer the estimated MLAC value.7,8
We found, however, no differences in the volume of solution administered for labor analgesia, VAS score for pain and overall maternal satisfaction between 0.1% bupivacaine and ropivacaine with fentanyl 2 μg/ml. Further, others investigators14,16,17 have administered relatively dilute LA solutions (0.075%, 0.08% and 0.1%) with opioids, using the PCEA method. Although the PCEA settings varied, the results were similar to this study. No differences were found between groups in the volume of LA required to produce labor analgesia. We used the PCEA with background infusion of the same solution, systematic review by Halpern et al3 concluded that a continuous background infusion improved maternal analgesia and reduced unscheduled clinician interventions.
In contrast to PCEA studies, several studies have compared “equianalgesic” concentrations of bupivacaine and ropivacaine based on the relative potency difference reported in the MLAC studies.7,8 Mandell et al18 administered 0.1% ropivacaine and 0.06% bupivacaine with 2 μg/ml fentanyl for maintenance analgesia in laboring women and found lower VAS scores in patients administered ropivacaine. In addition, Atiénzar et al19 found that there were no significant differences in the total dose of LA and the number of rescue boluses when 0.2% ropivacaine or 0.125% bupivacaine and levobupivacaine was used with 1 μg /ml fentanyl.
In the present study, we observed that the onset of analgesia achieved within fifteen minutes in all the parturient and was comparable in both the groups. Chhetty YK et al20 reported that onset of analgesia was achieved in 5-15 minutes after epidural bolus of 0.125% ropivacaine with 2 μg/mL fentanyl.
The PCEA using high volume, dilute LA solutions and opioids with a continuous background infusion appear to be improved maternal analgesia. In the present study, no motor block was observed in both groups until two hours after initial injection. The incidence of motor block increased as the duration of labor increased, more patient develop motor block in bupivacaine group. Clinical studies comparing using equal concentration of ropivacaine or bupivacaine with fentanyl, found more motor blockade with bupivacaine, and the difference was evident within one hour.9,16, Both the study used 1.5% lignocaine (3 ml) with 15 μg epinephrine as test dose, could have been inhibited the motor function. Recently, Guo S et al in a meta-analysis concluded that analgesia with ropivacaine in combination with fentanyl for labor pain is associated with lower incidence of motor blocks in comparison with analgesia with bupivacaine and fentanyl.21 The hemodynamic parameters as in Figures 3a, b and c in both the groups with respect to, heart rate SBP and DBP were comparable, none of the patients had episodes of hypotension or bradycardia requiring treatment.
The injection to complete dilatation of cervix, duration of labor, number of vaginal, instrumental, cesarean deliveries, neonatal outcome and overall maternal satisfaction were comparable in both the groups as observed by the others.21,22,23 Cochrane systematic review (2011) 24 authors believed that epidural analgesia appeared to be effective in reducing pain during labor. However, women who used this form of pain relief were at increased risk of having an instrumental delivery and an increased risk of cesarean section for fetal distress. Epidural analgesia had no statistically significant impact on the risk of cesarean section, maternal satisfaction with pain relief and neonatal outcome as determined by Apgar scores. However, they also stated that further research would be helpful to evaluate rare but potentially severe adverse effects of epidural analgesia on women in labor and long-term neonatal outcomes.
No parturient had pruritus, nausea, urinary retention, vomiting, shivering, though cases of pruritus,14 have been reported with epidural labor analgesia. All the parturient delivered vaginally were satisfied with management of labor similar to Lee et al22 who reported a satisfaction grade of 8 on a scale of 10 for all concentrations.
Our study has some limitations. First, the requirement of a larger sample size which would give a wider perspective on maternal and neonatal side-effects. Similarly, a comparison of intermittent boluses versus a continuous infusion technique would give a better estimation of LA and opioid consumption in both groups.
CONCLUSION
In conclusion, the present study showed that 0.1% ropivacaine or 0.1% bupivacaine, with fentanyl 2 μg/ml, were equally effective for labor analgesia using PCEA. There were statistically no significant differences in the amount of drug used, motor weakness, labor duration, or patient satisfaction.
Conflict of interest: No conflict of interest, actual or potential, declared by the authors in relation to this article
Authors’ contribution: All of the authors tool part in concept, conduction of the study work and manuscript editing
REFERENCES
- Melzack R. The myth of painless childbirth (the John J. Bonica lecture). Pain. 1984 Aug;19(4):321-37. [PubMed]
- Shnider SM, Abboud TK, Artal R, Henriksen EH, Stefani SJ, Levinson G. Maternal catecholamines decrease during labor after lumbar epidural anesthesia. Am J Obstet Gynecol. 1983 Sep;147(1):13-5. [PubMed]
- Halpern SH, Carvalho B. Patient- controlled epidural analgesia for labor. Anesth Analg. 2009 Mar;108(3):921-8. [PubMed]
- Eisenach JC, Grice SC, Dewan DM. Epinephrine enhances analgesia produced by epidural bupivacaine during labor. Anesth Analg. 1987 May;66(5):447-51. [PubMed]
- Kuthiala G, Chaudhary G. Ropivacaine: A review of its pharmacology and clinical use. Indian J Anaesth. 2011 Mar;55(2):104-10. doi: 10.4103/0019-5049.79875. [PubMed] [Free full text]
- Stienstra R, Jonker TA, Bourdrez P, Kuijpers JC, van Kleef JW, Lundberg U. Ropivacaine 0.25% versus bupivacaine 0.25% for continuous epidural analgesia in labor: A double-blind comparison. Anesth Analg. 1995 Feb;80(2):285-9. [PubMed]
- Polley LS, Columb MO, Naughton NN, Wagner DS, van de Ven CJ. Relative analgesic potencies of ropivacaine and bupivacaine for epidural analgesia in labor: implications for therapeutic indexes. Anesthesiology. 1999 Apr;90(4):944-50. [PubMed] [Free full text]
- Palm S, Gertzen W, Ledowski T, Gleim M, Wulf H. Minimum local analgesic dose of plain ropivacaine vs. ropivacaine combined with sufentanil during epidural analgesia for labour. Anaesthesia. 2001 Jun;56(6):526-9. [PubMed]
- Meister GC, D’Angelo R, Owen M, Nelson KE, Gaver R. A comparison of epidural analgesia with 0.125% ropivacaine with fentanyl versus 0.125% bupivacaine with fentanyl during labor. Anesth Analg. 2000 Mar;90(3):632-7. [PubMed]
- Halpern SH, Breen TW, Campbell DC, Muir HA, Kronberg J, Nunn R, et al. A multicenter, randomized, controlled trial comparing bupivacaine with ropivacaine for labor analgesia. Anesthesiology. 2003 Jun;98(6):1431-5. [PubMed] [Free full text]
- Lyons G, Columb M, Hawthorne L, Dresner M. Extradural pain relief in labour: bupivacaine sparing by extradural fentanyl is dose dependent. Br J Anaesth. 1997 May;78(5):493-7. [PubMed] [Free full text]
- Chua SM, Sia AT. Automated intermittent epidural boluses improve analgesia induced by intrathecal fentanyl during labour. Can J Anaesth. 2004;51(6):581-5. [PubMed]
- Owen MD, D’Angelo R, Gerancher JC, Thompson JM, Foss ML, Babb JD, et al. 0.125% ropivacaine is similar to 0.125% bupivacaine for labor analgesia using patient-controlled epidural infusion. Anesth Analg. 1998 Mar;86(3):527-31. [PubMed]
- Owen MD, Thomas JA, Smith T, Harris LC, D’Angelo R. Ropivacaine 0.075% and bupivacaine 0.075% with fentanyl 2 microg/ml are equivalent for labor epidural analgesia. Anesth Analg. 2002 Jan;94(1):179 -83. [PubMed]
- Beilin Y, Halpern S. Focused review: ropivacaine versus bupivacaine for epidural labor analgesia. Anesth Analg. 2010 Aug;111(2):482-7. doi: 10.1213/ANE.0b013e3181e3a08e [PubMed]
- Halpern SH, Breen TW, Campbell DC, Muir HA, Kronberg J, Nunn R, et al. A multicenter, randomized, controlled trial comparing bupivacaine with ropivacaine for labor analgesia. Anesthesiology. 2003 Jun;98(6):1431-5. [PubMed] [Free full text]
- Fischer C, Blanié P, Jaouën E, Vayssière C, Kaloul I, Coltat JC. Ropivacaine, 0.1%, plus sufentanil, 0.5 microg/ml, versus bupivacaine, 0.1%, plus sufentanil, 0.5 microg/ml, using patient-controlled epidural analgesia for labor: a double-blind comparison. Anesthesiology. 2000;92:1588-93. [PubMed] [Free full text]
- Mandell G, Makishima S, Ramanathan S. Is 0.1% Ropivacaine Equipotent to 0.06% Bupivacaine?: A Double-blinded, Randomized Study: A65 (Poster 24). Anesthesiology. 2000;2000NA. doi: 0000542-200004001-00065. [Free full text]
- Atiénzar MC, Palanca JM, Torres F, Borràs R, Gil S, Esteve I. A randomized comparison of levobupivacaine, bupivacaine and ropivacaine with fentanyl, for labor analgesia. Int J Obstet Anesth. 2008 Apr;17(2):106-11. doi: 10.1016/j.ijoa.2007 [PubMed]
- Chhetty YK, Naithani U, Gupta S, Bedi V, Agrawal I, Swain L. Epidural labor analgesia: A comparison of ropivacaine 0.125% versus 0.2% with fentanyl. J Obstet Anaesth Crit Care. 2013;3:16–22.[Free full text].
- Guo S, Li B, Gao C, Tian Y. Epidural analgesia with bupivacaine and fentanyl versus ropivacaine and fentanyl for pain relief in labor. a meta-analysis. Medicine(Baltimore). 2015 Jun;94(23):e880. doi: 10.1097/MD.0000000000000880. [PubMed] [Free full text]
- Lee BB, Ngan Kee WD, Lau WM, Wong AS. Epidural infusions for labor analgesia: a comparison of 0.2% ropivacaine, 0.1% ropivacaine, and 0.1%ropivacaine with fentanyl. Reg Anesth Pain Med. 2002 Jan-Feb;27(1):31-6. [PubMed]
- Bernard JM, Le Roux D, Frouin J. Ropivacaine and fentanyl concentrations in patient-controlled epidural analgesia during labor: A volume-range study. Anesth Analg. 2003 Dec;97(6):1800-7. [PubMed]
- Anim-Somuah M, Smyth RM, Jones L. Epidural versus non-epidural or no analgesia in labour. Cochrane Database Syst Rev. 2011 Dec 7;(12):CD000331. [PubMed]

