Yuka Matsuki, Ko Takakura, Kenji Shigemi
Department of Anesthesiology & Reanimatology, Faculty of Medical Sciences, University of Fukui, 23-3 Eiheijicho, Yoshidagun, Fukui 910-1193, (Japan)
Correspondence: Y. Matsuki, Department of Anesthesiology & Reanimatology, Faculty of Medicine Sciences, University of Fukui, 23-3 Eiheijicho, Yoshidagun, Fukui 910-1193, (Japan); Tel: +81-776-61-8391; Fax: +81-776-61-8116; E-mail: ymatsuki@u-fukui.ac.jp
ABSTRACT
We report a 50-year-old woman with severe acute pancreatitis induced shock, who was successfully treated with vasopressin. She took some antipsychotic agents for depression. Although treatment was started with continuous intravenous dopamine and noradrenaline, hypotension was not controlled. After continuous intravenous vasopressin was initiated, arterial blood pressure (BP) was raised and maintained. Vasopressin was effective to catecholamine-resistant shock in severe acute pancreatitis of the melancholic patient.
Key words: Vasopressin; Acute Pancreatitis; Shock, Catecholamine Resistant
Citation: Matsuki Y, Takakura K, Shigemi K. A case of successful treatment with vasopressin for severe acute pancreatitis in a melancholic patient administrated antipsychotic agents. Anaesth Pain & Intensive Care 2016;20(1):71-73.
INTRODUCTION
Severe acute pancreatitis is one of the refractory diseases with a high mortality rate. The prognosis is further exacerbated when it is accompanied with shock and multiorgan failure. Although most of the times shock can be treated by judicial use of catecholamines, these agents are not always effective in all cases. We report successful treatment with vasopressin in severe acute pancreatitis with catecholamine-resistant shock in a melancholic patient.
CASE REPORT
A 50-year-old woman was admitted to our hospital because of disturbance of consciousness. She had experienced stomach ache and fever for the previous three days. She had a history of autoimmune hepatitis and depression, and had suffered from acute pancreatitis four times. She had been on tab quetiapine fumarate 75 mg orally and tab aripiprazole (Abilify™) 6 mg orally for the past 6 years. On physical examination at the time of admission to the hospital, she had a temperature 38.0°C, BP 36/30 mmHg, heart rate 120 per min, SpO2 99% (on 7 L/min oxygen via face mask) and respiratory rate 29 per min. The Glasgow coma scale was 9/15.
Laboratory tests were ordered and the results are shown in Table 1.
Table 1: Blood chemistry and enzymes
| Parameter | Value |
| Leucocytes count | 4.2×109 /L |
| C-reactive protein | 468 mg/L |
| Hemoglobin | 14.7 g/L |
| Hematocrit | 0.45, |
| Platelets | 48×109/L |
| Na | 129 mmol/L |
| K | 5.4 mmol/L |
| Cl | 92 mmol/L |
| Urea nitrogen | 4.9 mmol/L |
| Creatinine | 661 μmol/L |
| Aspartate aminotransferase | 182 U/L |
| Alanine aminotransferase | 93 U/L |
| Lactate dehydrogenase | 1066 U/L |
| Amylase | 711 U/L |
Arterial blood gas analysis (on oxygen 7 L/min via face mask) showed metabolic acidosis (pH 7.158, PaO2 203 Torr, PaCO2 35.5 Torr, HCO3– 12.1 mmol/L, base excess ─15.7 mmol/L). Abdominal contrast-enhanced computed tomography revealed marked liquid retention in the pancreas, its surrounding retroperitoneal space and the mesocolon. The lab results and radiological examination confirmed the diagnosis of severe acute pancreatitis.
The clinical course is shown in Figure 1. When the patient entered the intensive care unit (ICU), her BP was low (40/26 mmHg) even after the continuous infusion of noradrenaline at a rate of 0.3 μg/kg/min. She was intubated and ventilated, and treated with infusion of ringer’s solution and antibiotics. Still her BP continued to be low. After the introduction of vasopressin (2.4 units/h), her BP improved and urine volume gradually increased. The patient fully recovered from shock, was removed from the ventilator and extubated. She was discharged from ICU on the 17th ICU day.
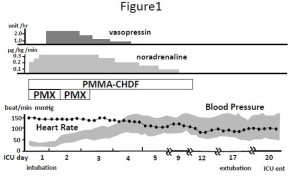
Figure 1: Clinical course of treatment and hemodynamics
[CHDF = Continuous hemodiafiltration; PMX-DHP = Polymyxin B-immobilized column direct hemoperfusion]
DISCUSSION
In our melancholic patient, when even noradrenaline infusion was not effective to treat severe shock with acute pancreatitis, vasopressin infusion successfully increased the BP gradually and the patient recovered from shock.
The possible causes for catecholamine─resistant shock in this patient were sepsis and long-term medication with antipsychotic agents. During sepsis, the mass production of nitric oxide (NO) by NO synthetase induced by bacterial endotoxins and cytokines is thought to cause hypotension, leading to diminished catecholamine response.1 Antipsychotic medications quetiapine and aripiprazole used by the present case have α1 receptor blocking actions and can potentially cause consequent catecholamine-resistant hypotension.
Regarding vasopressin, it inhibits the NO production which stimulated by IL-1 beta and endotoxin in septic shock,2 although plasma levels of vasopressin can be extremely low in septic shock.3 Vasopressin induces vasoconstriction by acting on the V1 receptor and not on the α1 receptor on vascular smooth muscle cells.4 These may be the reasons why vasopressin was effective in septic shock in our patient. Sepsis downregulates V2 receptors and dilates afferent arterioles in the kidney.5 Therefore, although vasopressin has an antidiuretic effect, a diuretic effect is sometimes observed during septic shock.6 In the present case patient’s urine output considerably increased after vasopressin administration.
In conclusion, vasopressin was effective in the melancholic patient of severe acute pancreatitis with catecholamine-resistant shock and should always be considered in refractory patients.
Authors’ contribution: All of the authors took part in the management of the case and preparation of the report.
REFERENCES
- Caroff SN, Mann SC. Neuroleptic malignant syndrome: Diagnostic issues. Psychiatr Ann. 1991;21:130-147.
- Kusano E, Tian S, Umino T, Tetsuka T, Ando Y, Asano Y. Arginine vasopressin inhibits interleukin-1 beta-stimulated nitric oxide and cyclic guanosine monophosphate production via the V1 receptor in cultured rat vascular smooth muscle cells. J Hypertens.1997;15:627-632. [PubMed]
- Landry DW, Levin HR, Gallant EM, Ashton RC Jr, Seo S, D’Alessandro D, et al. Vasopressin deficiency contributes to the vasodilation of septic shock. Circulation.1997;95:1122-1125. [PubMed] [Free full text]
- Patel BM, Chittock DR, Russell JA, Walley KR. Beneficial effects of short-term vasopressin infusion during severe septic shock. Anesthesiology.2002;96:576-582. [PubMed] [Free full text]
- Cross RB, Trace JW, Vattuone JR. The effect of vasopressin upon the vasculature of the isolated perfused rat kidney. J Physiol.1974;239:435-42. [PubMed] [Free full text]
- Robert W, Schrier RW, Wang W. Acute renal failure and sepsis. N Engl J Med. 2004;351:159-169. [PubMed]

