Azmat Riaz1, Ali Raza Ali Shah2, Syed Asad Ullah Jafri1
1Consultant Anesthesiologist, Department of Anesthesiology, Military Hospital, Rawalpindi (Pakistan)
2Consultant Anesthesiologist, Department of Anesthesiology, Combined Military Hospital, Kohat (Pakistan)
Correspondence: Azmat Riaz, Consultant Anesthesiologist, Department of Anesthesiology, Military Hospital, Rawalpindi (Pakistan); Phone: +92 333 8163966; E-mail: azmatrt@yahoo.com
ABSTRACT
Background: Single-shot caudal block is a common regional technique for below umbilicus surgery in children to provide intraoperative and postoperative analgesia. Traditionally the landmark technique has been used to perform this block but correct needle placement may sometimes be difficult due to anatomical variations. We performed this clinical trial to find out the usefulness of the recently introduced ultrasound guidance in success of performing caudal block.
Methodology: This randomized controlled clinical trial was conducted after approval from hospital ethical committee. 240 children between 2 and 10 years of age, were divided into two equal groups. Patients in first group (Group USG) received caudal block with the help of real-time ultrasonography, while the second group (Group LM) received blocks using traditional landmark technique. The primary end point was a successful block which was defined as injection into the caudal canal without any resistance, no blood or CSF on aspiration and no subcutaneous swelling. The secondary end point was no tachycardia (more than 10% increase in heart rate from base line) on skin incision. We also recorded block performing time and number of needle punctures. Mean and standard deviation values were calculated for age, weight and time taken in procedure. Frequency and percentages were calculated for gender, tachycardia and success on first attempt.
Results: There was no significant difference between the two groups in regards to age, gender or weight. However, the success on 1st attempt was higher in ultrasound group (95%) as compared to landmark technique (p = 0.000). Similarly, frequency of tachycardia on skin incision was significantly lower in ultrasound group (10%) as compared to landmark technique (p = 0.000). But the time taken was significantly higher in ultrasound group (110.88 ± 16.11 sec) as compared to landmark technique (63.62 ± 13.10 sec) {p= 0.000}
Conclusion: Success rate in placement of caudal block significantly is increased by using ultrasound guidance as compared to standard anatomical landmarks technique, but the time taken is significantly higher in ultrasound group as compared to landmark technique.
Key words: Caudal block; Ultrasound guided; Sacral hiatus; Sacral canal; Caudal epidural block
Citation: Riaz A, Shah ARA, Jafri SAU. Comparison of pediatric caudal block with ultrasound guidance or landmark technique. Anaesth. Pain & intensive care 2019;23(1):18-22
Received – 16 October 2018; Reviewed – 20 October 2018, 2 December 2018, ; Corrected – 6 January, 19 February,25 March 2019 ; Accepted – 25 March 2019
INTRODUCTION
Surgery is associated with painful stimulus which leads to stress response.1 Pharmacological measures to relieve pain can have multiple issues in pediatric population due to immature hepatic and renal systems. Regional anesthesia can suppress this stress response effectively.2 Compared to intravenous opioids, its use is associated with reduced frequency of side effects like respiratory depression and ileus etc.3
Caudal block is one of the most preferred regional anesthesia methods in pediatric population.4 If used in combination with general anesthesia, it helps in reducing opioid and inhalational anesthetic requirement.5
Ultrasonography is a safe non-invasive procedure, and has been used even in infants with sacral dimples.6 It has even been used for better understanding the anatomy for teaching purposes.7,8
Keeping in view the anatomic differences in landmarks,9,10 the significance of ultrasound guidance is increased. It has proven its worth as a safe and reliable modality to observe the anatomic differences.11 It improves the safety factor as needle can be redirected to avoid subarachnoid injection in case of unanticipated dural sac puncture.12 Though fluoroscopy is considered gold standard for caudal block, its limited availability and risk of radiation exposure gives an edge to ultrasound guided caudal block.13
However, its efficacy has not been studied much in Pakistan. So, we decided to perform this study to compare success in caudal block using standard anatomical landmark technique with ultrasound guidance.
METHODOLOGY
We included a total of 240 children, ASA I-II, aged between 2 and 10 years, who were scheduled for elective below umbilicus, abdominal, lower limb or perianal surgery after the ethical committee approval. The children were selected preoperatively at the time of preanesthesia assessment, procedure was explained to the guardian and written consent was obtained. The study was conducted at Military Hospital Rawalpindi from Nov 2017 to July 2018. Children who underwent emergency surgery; with spinal deformity, coagulation abnormality, history of allergy to local anesthetics, systemic infection or local infection at the site of block, were excluded from the study.
Eligible patients for this study were divided into two equal groups of 120 each, ultrasound-guided block group (Group USG) and landmark technique group (Group LM) using a computer-generated randomization.
Once the patients reached operating rooms, routine monitors, e.g., electrocardiogram (ECG), peripheral oxygen saturation (SpO2) and non-invasive blood pressure (NIBP), were applied and basal levels were recorded. No sedative agent was administered for pre-medication. Anesthesia was induced via a face mask with 6–8% sevoflurane in oxygen until the patients lost consciousness. Then vascular access was secured and LMA or I-gel of appropriate size was inserted. Patients were placed in the lateral position and caudal block was performed. Concentration of sevoflurane was reduced gradually to 2%. All conventional landmark and USG caudal blocks were performed by an experienced anesthesiologist.
Caudal block was performed in Group LM by conventional method. The sacral cornu and the sacral hiatus was palpated. After applying chlorhexidine solution, a 20–22-gauge needle was inserted into the skin at a 60–75-degree angle until the sacrococcygeal membrane was passed with a “pop”. Then, the angle of the needle was reduced to 25–30 degrees and inserted further for 2–3 mm, entering into the sacral canal. Aspiration was done and after confirming the absence of any blood or CSF 1 ml/kg bupivacaine 0.125% was injected, doing frequent aspirations. In the case of the needle touching the bone tissue, CSF or blood aspiration or subcutaneous tissue swelling, the angle of the needle was changed and the intervention was repeated.
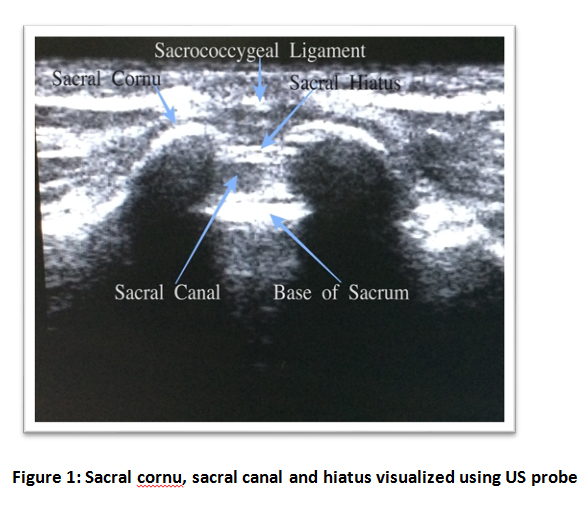
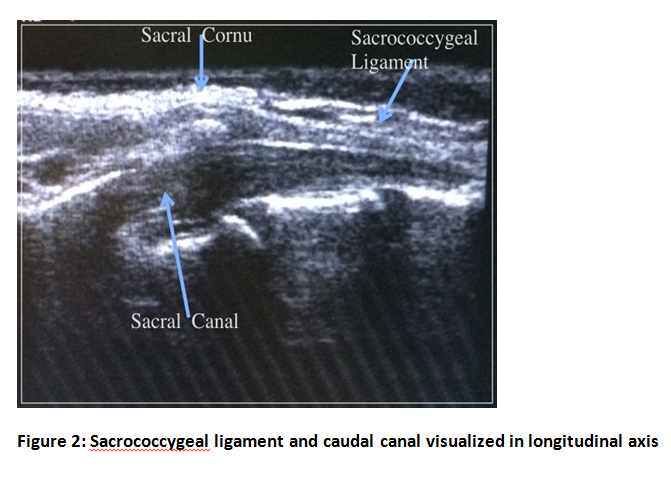
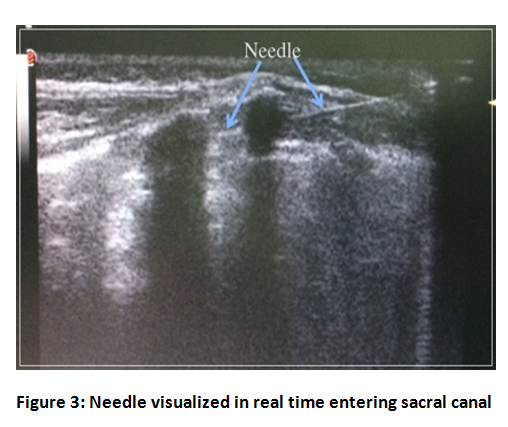
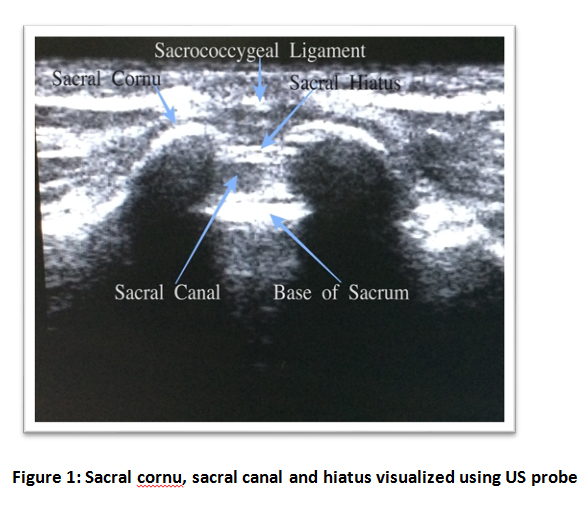
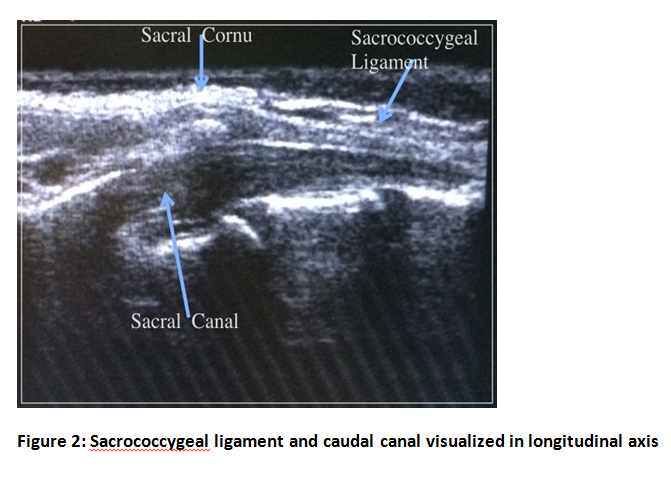
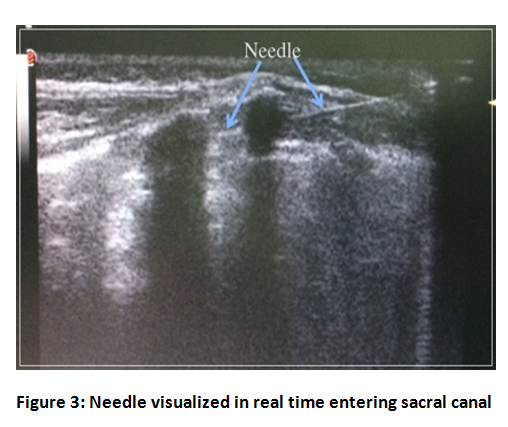
In USG group after sterilization of the region, sacral cornu and hiatus were visualized (Figure 1) using US probe. The probe was then rotated to 90 degrees and sacrococcygeal ligament and caudal canal were visualized (Figure 2). Using in-plane technique a 20-22 gauge needle was inserted through skin overlying sacrococcygeal ligament. The needle tip was continuously visualized in real-time till the tip entered sacral canal (Figure 3). After confirming the absence of any blood or CSF on aspiration, bupivacaine 0.125% 1 ml/kg was injected. Surgery in both groups was started 10 min after the application of caudal block.
Primary outcome of the study was a successful block injection, defined as no blood or cerebrospinal fluid on aspiration, injection into the caudal canal without any resistance and no subcutaneous swelling. If any of the above happened, the block was recorded as unsuccessful. Primary outcome was assessed by the same anesthesiologist performing the blocks.
Secondary outcomes were a heart rate increase on skin incision (defined as more than 10% increase in heart rate from the baseline), number of needle punctures and block performing times. The first puncture success was defined as reaching the sacral canal without any withdrawal from the skin. The block performance time was defined as the period (in sec) between the insertion of the needle and end of local anesthetic injection. Secondary outcomes were assessed by an anesthesia assistant.
Sample size was calculated using WHO calculator, using parameters keeping in view study of Abukawa and his colleagues.14 Level of significance was 5%, Power of test 90%, anticipated population proportion 1 = 10% and anticipated population proportion 2 = 75%.
Sample size in each group was calculated to be 120.
Statistical Analysis: Statistical analysis was done using IBM SPSS version 23. Mean and standard deviation were calculated for age, weight and time taken in procedure. These parameters were compared using Independent Sample’s t-test. Frequency and percentages were calculated for gender, tachycardia and success on first attempt. These parameters were compared using Chi square test. A p-value ≤ 0.05 was taken as significant.
RESULTS
Statistically there was no significant differences between the two groups in regard to age, gender or weight. However, the success on first attempt was higher in ultrasound group (95%) as compared to landmark technique group (70.83%). Similarly the frequency of increase in heart rate on skin incision was significantly lower in ultrasound group as compared to landmark technique, 10% vs. 32.5% respectively (Table 1). But the time taken was significantly higher in ultrasound group (110.88 ± 16.11 sec) as compared to landmark technique (63.62 ± 13.10 sec). Please see Table 1.
Table 1: Comparative age, gender, weight, success on 1st attempt, time taken to perform block and tachycardia on skin incision in two groups
DISCUSSION
Reliability of landmark technique for caudal block in infants and children has been questioned by many.15 Equiangular triangle, used for the identification of sacral hiatus, has been called a myth in children.16 However not many studies have been done on comparison of landmark technique and ultrasound guided caudal injection in children.
Nikooseresht and his colleagues17 worked on caudal block in adult population. They included 240 patients who had low backache or sciatica. Their success on first attempt was 95.8% which is quite similar to our study. They concluded that ultrasound not only helped in the procedure, but also in predicting its success.
Blanchais and his colleagues performed a study similar to Nikooseresht, on 30 patients with backache. And they also concluded that ultrasound improved the success rate of block.18
Caudal block is widely used for analgesia in pediatric population. We observed that success on first attempt was significantly higher in ultrasound group. This can be attributed to the fact that there are anatomical variations in pediatric population. However, duration of procedure was also significantly higher in ultrasound group.
Ahiskalioglu A et al.19 demonstrated that the duration of procedure was similar between the two groups. They performed their study on 134 children. Their timing of 109.9 ± 49.7 sec was similar to our timing of 110.88 ± 16.11 sec in ultrasound group. However, their timing in regards to landmark technique was higher than ours. Their study also showed that success in first puncture was significantly higher in ultrasound group. This is similar to our study; however, their block success rate was similar in both groups. Our study demonstrates better outcome with ultrasound. This may be due to difference in surgical procedure as their study primarily focused on phimosis/circumcision only, where as our study included all surgeries below umbilical region.
Study of Liu JZ, et al.20 also showed results similar to our study. They performed their study on 102 patients, with 52 patients in ultrasound group and 50 in control or traditional technique group. They concluded that success in first attempt and success of block were better in ultrasound group. However, their study showed that duration of procedure was also less in ultrasound group. Timing for ultrasound group was 1.40 ± 0.39 min and that for landmark technique was 3.23 ± 1.23 min. They concluded that using ultrasound is superior to landmark technique for caudal block.
LIMITATIONS
Major limitation of the study is that blinding was not possible as the procedure is totally different.
CONCLUSION
Our study shows that USG markedly improves the success rate of caudal block on first attempt in children aged between 2-10 years. The increased time taken with USG block may be successfully cut short with more practice.
Conflict of interest: None declared by the authors
Authors’ contribution:
AR – Concept, conduct of study, manuscript writing
ARAS - Manuscript writing, statistical analysis
SAUJ – Manuscript editing
REFERENCES
1Consultant Anesthesiologist, Department of Anesthesiology, Military Hospital, Rawalpindi (Pakistan)
2Consultant Anesthesiologist, Department of Anesthesiology, Combined Military Hospital, Kohat (Pakistan)
Correspondence: Azmat Riaz, Consultant Anesthesiologist, Department of Anesthesiology, Military Hospital, Rawalpindi (Pakistan); Phone: +92 333 8163966; E-mail: azmatrt@yahoo.com
ABSTRACT
Background: Single-shot caudal block is a common regional technique for below umbilicus surgery in children to provide intraoperative and postoperative analgesia. Traditionally the landmark technique has been used to perform this block but correct needle placement may sometimes be difficult due to anatomical variations. We performed this clinical trial to find out the usefulness of the recently introduced ultrasound guidance in success of performing caudal block.
Methodology: This randomized controlled clinical trial was conducted after approval from hospital ethical committee. 240 children between 2 and 10 years of age, were divided into two equal groups. Patients in first group (Group USG) received caudal block with the help of real-time ultrasonography, while the second group (Group LM) received blocks using traditional landmark technique. The primary end point was a successful block which was defined as injection into the caudal canal without any resistance, no blood or CSF on aspiration and no subcutaneous swelling. The secondary end point was no tachycardia (more than 10% increase in heart rate from base line) on skin incision. We also recorded block performing time and number of needle punctures. Mean and standard deviation values were calculated for age, weight and time taken in procedure. Frequency and percentages were calculated for gender, tachycardia and success on first attempt.
Results: There was no significant difference between the two groups in regards to age, gender or weight. However, the success on 1st attempt was higher in ultrasound group (95%) as compared to landmark technique (p = 0.000). Similarly, frequency of tachycardia on skin incision was significantly lower in ultrasound group (10%) as compared to landmark technique (p = 0.000). But the time taken was significantly higher in ultrasound group (110.88 ± 16.11 sec) as compared to landmark technique (63.62 ± 13.10 sec) {p= 0.000}
Conclusion: Success rate in placement of caudal block significantly is increased by using ultrasound guidance as compared to standard anatomical landmarks technique, but the time taken is significantly higher in ultrasound group as compared to landmark technique.
Key words: Caudal block; Ultrasound guided; Sacral hiatus; Sacral canal; Caudal epidural block
Citation: Riaz A, Shah ARA, Jafri SAU. Comparison of pediatric caudal block with ultrasound guidance or landmark technique. Anaesth. Pain & intensive care 2019;23(1):18-22
Received – 16 October 2018; Reviewed – 20 October 2018, 2 December 2018, ; Corrected – 6 January, 19 February,25 March 2019 ; Accepted – 25 March 2019
INTRODUCTION
Surgery is associated with painful stimulus which leads to stress response.1 Pharmacological measures to relieve pain can have multiple issues in pediatric population due to immature hepatic and renal systems. Regional anesthesia can suppress this stress response effectively.2 Compared to intravenous opioids, its use is associated with reduced frequency of side effects like respiratory depression and ileus etc.3
Caudal block is one of the most preferred regional anesthesia methods in pediatric population.4 If used in combination with general anesthesia, it helps in reducing opioid and inhalational anesthetic requirement.5
Ultrasonography is a safe non-invasive procedure, and has been used even in infants with sacral dimples.6 It has even been used for better understanding the anatomy for teaching purposes.7,8
Keeping in view the anatomic differences in landmarks,9,10 the significance of ultrasound guidance is increased. It has proven its worth as a safe and reliable modality to observe the anatomic differences.11 It improves the safety factor as needle can be redirected to avoid subarachnoid injection in case of unanticipated dural sac puncture.12 Though fluoroscopy is considered gold standard for caudal block, its limited availability and risk of radiation exposure gives an edge to ultrasound guided caudal block.13
However, its efficacy has not been studied much in Pakistan. So, we decided to perform this study to compare success in caudal block using standard anatomical landmark technique with ultrasound guidance.
METHODOLOGY
We included a total of 240 children, ASA I-II, aged between 2 and 10 years, who were scheduled for elective below umbilicus, abdominal, lower limb or perianal surgery after the ethical committee approval. The children were selected preoperatively at the time of preanesthesia assessment, procedure was explained to the guardian and written consent was obtained. The study was conducted at Military Hospital Rawalpindi from Nov 2017 to July 2018. Children who underwent emergency surgery; with spinal deformity, coagulation abnormality, history of allergy to local anesthetics, systemic infection or local infection at the site of block, were excluded from the study.
Eligible patients for this study were divided into two equal groups of 120 each, ultrasound-guided block group (Group USG) and landmark technique group (Group LM) using a computer-generated randomization.
Once the patients reached operating rooms, routine monitors, e.g., electrocardiogram (ECG), peripheral oxygen saturation (SpO2) and non-invasive blood pressure (NIBP), were applied and basal levels were recorded. No sedative agent was administered for pre-medication. Anesthesia was induced via a face mask with 6–8% sevoflurane in oxygen until the patients lost consciousness. Then vascular access was secured and LMA or I-gel of appropriate size was inserted. Patients were placed in the lateral position and caudal block was performed. Concentration of sevoflurane was reduced gradually to 2%. All conventional landmark and USG caudal blocks were performed by an experienced anesthesiologist.
Caudal block was performed in Group LM by conventional method. The sacral cornu and the sacral hiatus was palpated. After applying chlorhexidine solution, a 20–22-gauge needle was inserted into the skin at a 60–75-degree angle until the sacrococcygeal membrane was passed with a “pop”. Then, the angle of the needle was reduced to 25–30 degrees and inserted further for 2–3 mm, entering into the sacral canal. Aspiration was done and after confirming the absence of any blood or CSF 1 ml/kg bupivacaine 0.125% was injected, doing frequent aspirations. In the case of the needle touching the bone tissue, CSF or blood aspiration or subcutaneous tissue swelling, the angle of the needle was changed and the intervention was repeated.
In USG group after sterilization of the region, sacral cornu and hiatus were visualized (Figure 1) using US probe. The probe was then rotated to 90 degrees and sacrococcygeal ligament and caudal canal were visualized (Figure 2). Using in-plane technique a 20-22 gauge needle was inserted through skin overlying sacrococcygeal ligament. The needle tip was continuously visualized in real-time till the tip entered sacral canal (Figure 3). After confirming the absence of any blood or CSF on aspiration, bupivacaine 0.125% 1 ml/kg was injected. Surgery in both groups was started 10 min after the application of caudal block.
Primary outcome of the study was a successful block injection, defined as no blood or cerebrospinal fluid on aspiration, injection into the caudal canal without any resistance and no subcutaneous swelling. If any of the above happened, the block was recorded as unsuccessful. Primary outcome was assessed by the same anesthesiologist performing the blocks.
Secondary outcomes were a heart rate increase on skin incision (defined as more than 10% increase in heart rate from the baseline), number of needle punctures and block performing times. The first puncture success was defined as reaching the sacral canal without any withdrawal from the skin. The block performance time was defined as the period (in sec) between the insertion of the needle and end of local anesthetic injection. Secondary outcomes were assessed by an anesthesia assistant.
Sample size was calculated using WHO calculator, using parameters keeping in view study of Abukawa and his colleagues.14 Level of significance was 5%, Power of test 90%, anticipated population proportion 1 = 10% and anticipated population proportion 2 = 75%.
Sample size in each group was calculated to be 120.
Statistical Analysis: Statistical analysis was done using IBM SPSS version 23. Mean and standard deviation were calculated for age, weight and time taken in procedure. These parameters were compared using Independent Sample’s t-test. Frequency and percentages were calculated for gender, tachycardia and success on first attempt. These parameters were compared using Chi square test. A p-value ≤ 0.05 was taken as significant.
RESULTS
Statistically there was no significant differences between the two groups in regard to age, gender or weight. However, the success on first attempt was higher in ultrasound group (95%) as compared to landmark technique group (70.83%). Similarly the frequency of increase in heart rate on skin incision was significantly lower in ultrasound group as compared to landmark technique, 10% vs. 32.5% respectively (Table 1). But the time taken was significantly higher in ultrasound group (110.88 ± 16.11 sec) as compared to landmark technique (63.62 ± 13.10 sec). Please see Table 1.
Table 1: Comparative age, gender, weight, success on 1st attempt, time taken to perform block and tachycardia on skin incision in two groups
| Parameters | Group USG
(Ultrasound) |
Group LM
(Land Mark) |
p value |
| Age (years) | 5.04 ± 2.86 | 5.00 ± 2.87 | 0.838 |
| Gender (Male/Female) | 107/13 | 102/18 | 0.336 |
| Weight (kg) | 19.09 ± 5.71 | 19.01 ± 5.73 | 0.838 |
| Success in 1st attempt | 114 (95%) | 85 (70.83%) | 0.000 |
| Time taken (sec) | 110.88 ± 16.11 | 63.62 ± 13.10 | 0.000 |
| Tachycardia on skin incision [n(%)] | 12 (10%) | 39 (32.5%) | 0.000 |
DISCUSSION
Reliability of landmark technique for caudal block in infants and children has been questioned by many.15 Equiangular triangle, used for the identification of sacral hiatus, has been called a myth in children.16 However not many studies have been done on comparison of landmark technique and ultrasound guided caudal injection in children.
Nikooseresht and his colleagues17 worked on caudal block in adult population. They included 240 patients who had low backache or sciatica. Their success on first attempt was 95.8% which is quite similar to our study. They concluded that ultrasound not only helped in the procedure, but also in predicting its success.
Blanchais and his colleagues performed a study similar to Nikooseresht, on 30 patients with backache. And they also concluded that ultrasound improved the success rate of block.18
Caudal block is widely used for analgesia in pediatric population. We observed that success on first attempt was significantly higher in ultrasound group. This can be attributed to the fact that there are anatomical variations in pediatric population. However, duration of procedure was also significantly higher in ultrasound group.
Ahiskalioglu A et al.19 demonstrated that the duration of procedure was similar between the two groups. They performed their study on 134 children. Their timing of 109.9 ± 49.7 sec was similar to our timing of 110.88 ± 16.11 sec in ultrasound group. However, their timing in regards to landmark technique was higher than ours. Their study also showed that success in first puncture was significantly higher in ultrasound group. This is similar to our study; however, their block success rate was similar in both groups. Our study demonstrates better outcome with ultrasound. This may be due to difference in surgical procedure as their study primarily focused on phimosis/circumcision only, where as our study included all surgeries below umbilical region.
Study of Liu JZ, et al.20 also showed results similar to our study. They performed their study on 102 patients, with 52 patients in ultrasound group and 50 in control or traditional technique group. They concluded that success in first attempt and success of block were better in ultrasound group. However, their study showed that duration of procedure was also less in ultrasound group. Timing for ultrasound group was 1.40 ± 0.39 min and that for landmark technique was 3.23 ± 1.23 min. They concluded that using ultrasound is superior to landmark technique for caudal block.
LIMITATIONS
Major limitation of the study is that blinding was not possible as the procedure is totally different.
CONCLUSION
Our study shows that USG markedly improves the success rate of caudal block on first attempt in children aged between 2-10 years. The increased time taken with USG block may be successfully cut short with more practice.
Conflict of interest: None declared by the authors
Authors’ contribution:
AR – Concept, conduct of study, manuscript writing
ARAS - Manuscript writing, statistical analysis
SAUJ – Manuscript editing
REFERENCES
- Yuki K, Matsunami E, Tazawa K, Wang W, DiNardo JA, Koutsogiannaki S. Pediatric Perioperative Stress Responses and Anesthesia. Transl Perioper Pain Med. 2017;2(1):1–12 [Free Full Text]
- Wolf AR. Effects of regional analgesia on stress responses to pediatric surgery. Paediatr Anaesth. 2012;22(1):19-24. [PubMed] [Free Full Text]
- Willschke H, Kettner S. Pediatric regional anesthesia: abdominal wall blocks. Paediatr Anaesth. 2012;22(1):88-92 [PubMed]
- Praveen, R. Remadevi, and N. Pratheeba. Caudal Epidural Analgesia in Pediatric Patients: Comparison of 0.25% Levobupivacaine and 0.25% Ropivacaine in Terms of Motor Blockade and Postoperative Analgesia. Anesth Essays Res. 2017;11(1):223–7. [PubMed] [Free Full Text]
- Marjanovic V, Budic I, Stevic M, Simicc D. A Comparison of Three Different Volumes of Levobupivacaine for Caudal Block in Children Undergoing Orchidopexy and Inguinal Hernia Repair. Med Princ Pract. 2017;26(4):331–336. [PubMed] [Free Full Text]
- Choi JH, Lee T, Kwon HH, You SK, Joon Won Kang. Outcome of ultrasonographic imaging in infants with sacral dimple. Korean J Pediatr. 2018 Jun;61(6):194–9. [Free Full Text]
- Sweetman GM, Crawford G, Hird K, Fear MW. The benefits and limitations of using ultrasonography to supplement anatomical understanding. Anat Sci Educ. 2013 May-Jun;6(3):141-8. [PubMed]
- Dreher SM, DePhilip R, Bahner D. Ultrasound exposure during gross anatomy. J Emerg Med. 2014 Feb;46(2):231-40 [PubMed] [Free Full Text]
- Park GY, Kwon DR, Cho HK. Anatomic Differences in the Sacral Hiatus During Caudal Epidural Injection Using Ultrasound Guidance. J Ultrasound Med. 2015 Dec;34(12):2143-8. [PubMed] [Free Full Text]
- Bagheri H, Govsa F. Anatomy of the sacral hiatus and its clinical relevance in caudal epidural block. Surg Radiol Anat. 2017 Sep;39(9):943-951. [PubMed] [Free Full Text]
- Nikooseresht M, Hashemi M, Mohajerani SA, Shahandeh F, Agah M. Ultrasound as a Screening Tool for Performing Caudal Epidural Injections. Iran J Radiol. 2014 May;11(2):e13262. [Free Full Text]
- Sinskey JL, Vecchione TM, Ekstrom BG, Boretsky K. Benefits of Ultrasound Imaging for Placement of Caudal Epidural Blockade in 3 Pediatric Patients: A Case Report. A A Pract. 2018 Jun 1;10(11):307-309. [PubMed]
- Kao SC, Lin CS. Caudal Epidural Block: An Updated Review of Anatomy and Techniques. Biomed Res Int. 2017;2017:9217145. [Free Full Text]
- Abukawa Y, Hiroki K, Morioka N, Iwakiri H, Fukada T, Higuchi H et al. Ultrasound versus anatomical landmarks for caudal epidural anesthesia in pediatric patients. BMC Anesthesiol. 2015;15:102. [Free Full Text]
- Mirjalili SA, Taghavi K, Frawley G, Craw S. Should we abandon landmark-based technique for caudal anesthesia in neonates and infants? Paediatr Anaesth. 2015;25(5):511-6. [PubMed]
- Kim MS, Han KH, Kim EM, Jeong SH, Lee JR. The myth of the equiangular triangle for identification of sacral hiatus in children disproved by ultrasonography. Reg Anesth Pain Med. 2013;38(3):243-7 [PubMed]
- Nikooseresht M, Hashemi M, Mohajerani SA, Shahandeh F, Agah M. Ultrasound as a Screening Tool for Performing Caudal Epidural Injections. Iran J Radiol. 2014; 11(2): e13262. [Free Full Text]
- Blanchais A, Le Goff B, Guillot P, Berthelot JM, Glemarec J, Maugars Y. Feasibility and safety of ultrasound-guided caudal epidural glucocorticoid injections. Joint Bone Spine. 2010 Oct;77(5):440-4. [PubMed] [Free Full Text]
- Ahiskalioglu A, Yayik AM, Ahiskalioglu EO, Ekinci M, Gölboyu BE, Celik EC. Ultrasound-guided versus conventional injection for caudal block in children: A prospective randomized clinical study. J Clin Anesth. 2018;44:91-96. [PubMed] [Free Full Text]
- Liu JZ, Wu XQ, Li R, Zhang YJ. A comparison of ultrasonography versus traditional approach for caudal block in children. Zhonghua Yi Xue Za Zhi. 2012 3;92(13):882-5. [PubMed]