Yasuhiro Morimoto, MD1
1Department of Anesthesia, Ube Industries Central Hospital, Ube Yamaguchi, (Japan)
Correspondence: Yasuhiro Morimoto, MD, 750-Nishikiwa Ube Yamaguchi 755-0151(Japan); E-mail: yasumorimo@gmail.com
ABSTRACT
Regional anesthesiahas an important role in the anesthetic management of thoracic surgeries.Regional anesthesia provides better pain control than systemic opioid analgesia, controls stress response, and prevents respiratory complications.These factors should improve patient outcomes.The first choice of regional anesthesia for thoracic surgery is epidural analgesia or thoracic paravertebral block (TPVB).In general, analgesic efficiency of epidural analgesia and TPVB is equivalent.However, TPVB has some advantage over epidural analgesia including fewer complications.When these two blocks are contraindicated, application of intercostal nerve block or inter-pleural block can be considered.
Key words:Epidural Analgesia; Nerve Block; Thoracic Surgery; Thoracic Surgical Procedures; Anesthesia, Conduction;Anesthesia, Local;Anesthesia, Spinal; Anesthesia, Epidural; Ultrasonography
Citation: Morimoto Y. Regional anesthesia for thoracic surgery. Anaesth Pain & Intensive Care 2015;19(3):352-356
INTRODUCTION
Regional anesthesia plays an important role in thoracic surgeries.1Severe pain is common after thoracic surgeries. Compared to systemic opioid analgesia, regional anesthesia results in better pain control, better control of stress response and lesser respiratory complications.These will improve overall patient outcomes.
In addition, chronic pain after thoracic surgery is common and may persist for several years, use of regional analgesia techniques may decrease this complication.
Recently, non-intubated surgery with regional anesthesia for high-risk patients has beenreported.2There are several regional anesthesia techniques for thoracic surgeriesIn this review, I would like to summarize these techniques and their indications for use during thoracic surgeries, in particularly lung surgeries.
ANATOMY CRUCIAL TO THORACIC SURGERY
Several nerves are involved in thoracic surgery. The intercostal nerve is the most important component in the skin and muscles at the incision site and the ribs. Damage to the intercostal nerve may lead to chronic pain, and hence nociceptive transmission via the intercostal nerve should be blocked by regional anesthesia.
The vagus and phrenic nerves are associated with pain stimuli originating in the mediastinal and diaphragmatic pleura, and the brachial plexus is associated with shoulder pain after surgery.
These nerves cannot be blocked by regional anesthesia in the thoracic region; therefore, multimodal analgesia with opioids and non-steroidal anti-inflammatory drugs (NSAIDs) should be considered along with use of regional analgesia techniques.
The intercostal nerve runs between the internal intercostal muscle and pleura. The intercostal nerve block (INB) involves a distal approach to the intercostal nerve, while the thoracic paravertebral block (TPVB) involves a more proximal approach. TPVB provides multi-segmental intercostal nerve blockade as well as sympathetic block; therefore, it is a good alternative for epidural analgesia for thoracic surgeries.
CHOICE OF REGIONAL ANESTHESIA FOR THORACIC SURGERY
The first choice of regional anesthesia for thoracic surgeries is epidural analgesia.Recently ultrasound guided TPVB is a good alternative when epidural analgesia is contraindicated for patients receiving anti-coagulant therapy or those with bleeding tendencies. Although TPVB is safer than epidural analgesia for these patients, it should be carefully selected. When these two blocks are contraindicated, the intercostal nerve block or interpleural block can be considered.
EPIDURAL ANALGESIA AND TPVB
Thoracic epidural analgesia remains the gold standard analgesia technique for thoracic surgeries. It provides excellent pain control after the procedure. However, it is not indicated for patients receiving anti-coagulant therapy or those with bleeding tendencies. It causes rare but serious complications, including epidural abscess and hematoma formation, after the procedure. It also causes hypotension.
The level of puncture for epidural analgesia depends on the surgical incision site, although it is usually between T3 and T7. The required level of analgesia is between T2 and T12.
Thoracic paravertebral block(TPVB) is an alternative to thoracic epidural analgesia. It is safe and successful under ultrasound guidance. We can perform TPVB under deep sedation or general anesthesia; therefore, it can also be used for pediatric patients. TPVB offers the advantages of a unilateral block and a low incidence of hypotension, urinary retention and pulmonary complications. It can result in pneumothorax, but the incidence is low at 0.5%. When thoracic surgery with chest tube placement is planned, this does not pose a serious problem.
Several studies have compared epidural analgesia and TPVB for thoracic surgery.3,4 In general, the analgesic efficacy of both these techniques is equivalent. However, complications are more common with epidural analgesia and include urinary retention, nausea and hypotension. Furthermore, pulmonary function is better preserved with TPVB. Pintaricet al5 compared continuous thoracic epidural analgesia with TPVB in patients who underwent open lung surgery. TPVB resulted in similar analgesia but greater hemodynamic stability compared with epidural analgesia. In addition, TPVB required a smaller volume of colloids and vasopressors.
An unresolved issue with TPVB is its safety in patients receiving anti-coagulant therapy or those with bleeding tendencies. Therefore, the application of TPVB for the patients is similar to epidural analgesia.
Figure 1 shows the anatomy of the thoracic paravertebral space. The paravertebral space lies adjacent to the vertebral body and between the pleura and internal intercostal muscle. Note that on the proximal side, the internal intercostal muscle transitions to the internal intercostal membrane and the costotransverse ligament.
Figure 2 shows an ultrasound view for PVB. In the longitudinal view, we can recognize the paravertebral space between the transverse process and between the

Figure 1: Anatomy of thoracic paravertebral space
PV space = para vertebral space
costo transverse ligament and pleura. In the transverse view, the paravertebral space is recognized between the internal intercostal muscle and pleura. I use the transverse view for ultrasound-guided TPVB. The needle is inserted using an in-line approach.

Figure 2: Ultrasound views for thoracic paravertebral block
TP = transverse process
The patient is placed in the lateral position. TPVB can be administered before or after the induction of general anesthesia. I administer a single injection of 20 mL of 0.2% ropivacaine at needle insertion, followed by catheter insertion. I then administer another single injection of 10 mL of 0.2% ropivacaine at the end of surgery, followed by continuous infusion of 0.2% ropivacaine at 4 mL/h in the post-operative period.
INTERCOSTAL NERVE BLOCK AND OTHER TECHNIQUES
The intercostal nerve block involves a more distal approach to the intercostal nerve compared with TPVB. The indications for this block are similar to those for TPVB. Video-assisted thoracic surgery is a good indication for this block. The local anesthetic remains confined to the intercostal space and should be injected at several intercostal levels depending on the procedure.
There are two techniques for intercostal nerve block. The percutaneous approach is normally employed before the procedure. The other approach involves the intra-operative injection of local anesthetic solution under direct vision by the surgeon.6
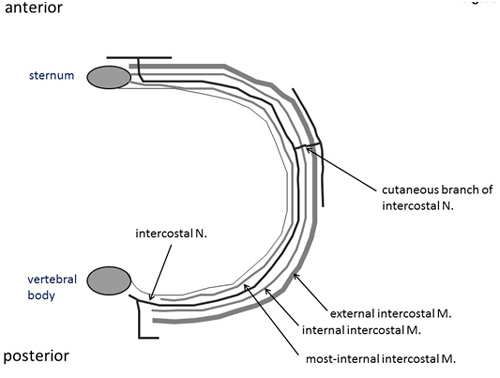
Figure 3: Anatomy of intercostal nerve(N)
Figure 3 shows the anatomy of the intercostal nerve, which runs between the internal intercostal muscle and the innermost internal intercostal muscle. The intercostal nerve gives out a cutaneous branch at the mid-axillary line; therefore, the intercostal nerve block should be administered at the posterior thoracic wall for thoracic surgery.
I perform this block after the induction of general anesthesia under ultrasound guidance (Figure 4). The patient is placed in lateral position. After locating the ultrasound probe in the intercostal space, the pleura and the intercostal muscles
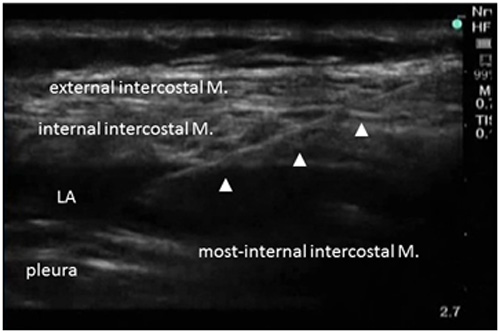
Figure 4: Ultrasound view during intercostal nerve block
LA = local anesthetic; ▲: block needle
LA is injected between internal intercostal muscle(M) and most-internal intercostal M.
should be identified. I insert the block needle by using an in-line approach. Then, a local anesthetic is injected between the internal intercostal muscle and the innermost internal intercostal muscle. If the innermost internal intercostal muscle is not identified, the anesthetic can be injected above the pleura. I use 5 mL of 0.375% ropivacaine for each intercostal space.
A recent study used liposomal bupivacaine for intercostal nerve blocks.7This technique offered post-operative pain scores comparable to those after thoracic epidural analgesia. Therefore, intercostal nerve block with liposomal bupivacaine may be considered a suitable alternative to epidural analgesia.
Another approach is interpleural administration of local anesthetics. A catheter is introduced percutaneously into the pleural space with the chest tube before the end of the procedure. Then, a large amount of anesthetic is infused intermittently or continuously, and the chest tubes are clamped for 5 to 30 min. This technique is easy and reliably places the catheter into the pleural space. However, the effects of this approach are limited. Chest tube management is essential.
NON-INTUBATED THORACIC SURGERY
Non-intubated thoracic surgery, which is also called awake thoracic surgery, is aimed at minimizing the risks of general anesthesia with one-lung ventilation.2 This technique is less invasive and does not require endotracheal intubation. Non-intubated thoracic surgery facilitates faster recovery and a shorter hospital stay. On the other hand, coughing, poor maneuverability due to diaphragmatic and lung movements, and patient movements are the limitations of this procedure. Therefore, the indications for this technique should be well considered with the surgeon and the patient.
Non-intubated thoracic surgery is technically more challenging than thoracic surgery under general anesthesia. Regional anesthesia plays a major role in this procedure. Awake video-assisted thoracic surgery has been performed with intercostal nerve blocks and local anesthetic infiltration at the incision site, while TPVB and epidural anesthesia are used for more invasive procedures.8Piccioni et al9 reported two cases of non-intubated thoracic surgeries with TPVB and concluded that the use of TPVB for video-assisted thoracoscopy resulted in adequate anesthesia with high levels of patient satisfaction.
In the near future, non-intubated thoracic surgery by regional anesthesia will play an increased role in the anesthetic management for thoracic surgery.
CONCLUSIONS
Regional anesthesia plays an important role in thoracic surgery, particularly with regard to post-operative pain control. The first choice of regional anesthesia for thoracic surgery is epidural analgesia or TPVB.In general, the analgesic efficiencies of epidural analgesia and TPVB are equivalent. However, TPVB has some advantages over epidural analgesia, including fewer complications. When these two blocks are contraindicated, intercostal nerve block or interpleural block should be considered.
Non-intubated thoracic surgery presents a challenge, and excellent regional anesthesia techniques facilitate the successful performance of this procedure.
REFERENCES
1Department of Anesthesia, Ube Industries Central Hospital, Ube Yamaguchi, (Japan)
Correspondence: Yasuhiro Morimoto, MD, 750-Nishikiwa Ube Yamaguchi 755-0151(Japan); E-mail: yasumorimo@gmail.com
ABSTRACT
Regional anesthesiahas an important role in the anesthetic management of thoracic surgeries.Regional anesthesia provides better pain control than systemic opioid analgesia, controls stress response, and prevents respiratory complications.These factors should improve patient outcomes.The first choice of regional anesthesia for thoracic surgery is epidural analgesia or thoracic paravertebral block (TPVB).In general, analgesic efficiency of epidural analgesia and TPVB is equivalent.However, TPVB has some advantage over epidural analgesia including fewer complications.When these two blocks are contraindicated, application of intercostal nerve block or inter-pleural block can be considered.
Key words:Epidural Analgesia; Nerve Block; Thoracic Surgery; Thoracic Surgical Procedures; Anesthesia, Conduction;Anesthesia, Local;Anesthesia, Spinal; Anesthesia, Epidural; Ultrasonography
Citation: Morimoto Y. Regional anesthesia for thoracic surgery. Anaesth Pain & Intensive Care 2015;19(3):352-356
INTRODUCTION
Regional anesthesia plays an important role in thoracic surgeries.1Severe pain is common after thoracic surgeries. Compared to systemic opioid analgesia, regional anesthesia results in better pain control, better control of stress response and lesser respiratory complications.These will improve overall patient outcomes.
In addition, chronic pain after thoracic surgery is common and may persist for several years, use of regional analgesia techniques may decrease this complication.
Recently, non-intubated surgery with regional anesthesia for high-risk patients has beenreported.2There are several regional anesthesia techniques for thoracic surgeriesIn this review, I would like to summarize these techniques and their indications for use during thoracic surgeries, in particularly lung surgeries.
ANATOMY CRUCIAL TO THORACIC SURGERY
Several nerves are involved in thoracic surgery. The intercostal nerve is the most important component in the skin and muscles at the incision site and the ribs. Damage to the intercostal nerve may lead to chronic pain, and hence nociceptive transmission via the intercostal nerve should be blocked by regional anesthesia.
The vagus and phrenic nerves are associated with pain stimuli originating in the mediastinal and diaphragmatic pleura, and the brachial plexus is associated with shoulder pain after surgery.
These nerves cannot be blocked by regional anesthesia in the thoracic region; therefore, multimodal analgesia with opioids and non-steroidal anti-inflammatory drugs (NSAIDs) should be considered along with use of regional analgesia techniques.
The intercostal nerve runs between the internal intercostal muscle and pleura. The intercostal nerve block (INB) involves a distal approach to the intercostal nerve, while the thoracic paravertebral block (TPVB) involves a more proximal approach. TPVB provides multi-segmental intercostal nerve blockade as well as sympathetic block; therefore, it is a good alternative for epidural analgesia for thoracic surgeries.
CHOICE OF REGIONAL ANESTHESIA FOR THORACIC SURGERY
The first choice of regional anesthesia for thoracic surgeries is epidural analgesia.Recently ultrasound guided TPVB is a good alternative when epidural analgesia is contraindicated for patients receiving anti-coagulant therapy or those with bleeding tendencies. Although TPVB is safer than epidural analgesia for these patients, it should be carefully selected. When these two blocks are contraindicated, the intercostal nerve block or interpleural block can be considered.
EPIDURAL ANALGESIA AND TPVB
Thoracic epidural analgesia remains the gold standard analgesia technique for thoracic surgeries. It provides excellent pain control after the procedure. However, it is not indicated for patients receiving anti-coagulant therapy or those with bleeding tendencies. It causes rare but serious complications, including epidural abscess and hematoma formation, after the procedure. It also causes hypotension.
The level of puncture for epidural analgesia depends on the surgical incision site, although it is usually between T3 and T7. The required level of analgesia is between T2 and T12.
Thoracic paravertebral block(TPVB) is an alternative to thoracic epidural analgesia. It is safe and successful under ultrasound guidance. We can perform TPVB under deep sedation or general anesthesia; therefore, it can also be used for pediatric patients. TPVB offers the advantages of a unilateral block and a low incidence of hypotension, urinary retention and pulmonary complications. It can result in pneumothorax, but the incidence is low at 0.5%. When thoracic surgery with chest tube placement is planned, this does not pose a serious problem.
Several studies have compared epidural analgesia and TPVB for thoracic surgery.3,4 In general, the analgesic efficacy of both these techniques is equivalent. However, complications are more common with epidural analgesia and include urinary retention, nausea and hypotension. Furthermore, pulmonary function is better preserved with TPVB. Pintaricet al5 compared continuous thoracic epidural analgesia with TPVB in patients who underwent open lung surgery. TPVB resulted in similar analgesia but greater hemodynamic stability compared with epidural analgesia. In addition, TPVB required a smaller volume of colloids and vasopressors.
An unresolved issue with TPVB is its safety in patients receiving anti-coagulant therapy or those with bleeding tendencies. Therefore, the application of TPVB for the patients is similar to epidural analgesia.
Figure 1 shows the anatomy of the thoracic paravertebral space. The paravertebral space lies adjacent to the vertebral body and between the pleura and internal intercostal muscle. Note that on the proximal side, the internal intercostal muscle transitions to the internal intercostal membrane and the costotransverse ligament.
Figure 2 shows an ultrasound view for PVB. In the longitudinal view, we can recognize the paravertebral space between the transverse process and between the

Figure 1: Anatomy of thoracic paravertebral space
PV space = para vertebral space
costo transverse ligament and pleura. In the transverse view, the paravertebral space is recognized between the internal intercostal muscle and pleura. I use the transverse view for ultrasound-guided TPVB. The needle is inserted using an in-line approach.

Figure 2: Ultrasound views for thoracic paravertebral block
TP = transverse process
The patient is placed in the lateral position. TPVB can be administered before or after the induction of general anesthesia. I administer a single injection of 20 mL of 0.2% ropivacaine at needle insertion, followed by catheter insertion. I then administer another single injection of 10 mL of 0.2% ropivacaine at the end of surgery, followed by continuous infusion of 0.2% ropivacaine at 4 mL/h in the post-operative period.
INTERCOSTAL NERVE BLOCK AND OTHER TECHNIQUES
The intercostal nerve block involves a more distal approach to the intercostal nerve compared with TPVB. The indications for this block are similar to those for TPVB. Video-assisted thoracic surgery is a good indication for this block. The local anesthetic remains confined to the intercostal space and should be injected at several intercostal levels depending on the procedure.
There are two techniques for intercostal nerve block. The percutaneous approach is normally employed before the procedure. The other approach involves the intra-operative injection of local anesthetic solution under direct vision by the surgeon.6
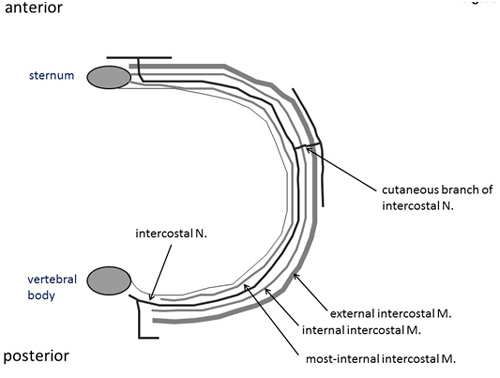
Figure 3: Anatomy of intercostal nerve(N)
Figure 3 shows the anatomy of the intercostal nerve, which runs between the internal intercostal muscle and the innermost internal intercostal muscle. The intercostal nerve gives out a cutaneous branch at the mid-axillary line; therefore, the intercostal nerve block should be administered at the posterior thoracic wall for thoracic surgery.
I perform this block after the induction of general anesthesia under ultrasound guidance (Figure 4). The patient is placed in lateral position. After locating the ultrasound probe in the intercostal space, the pleura and the intercostal muscles
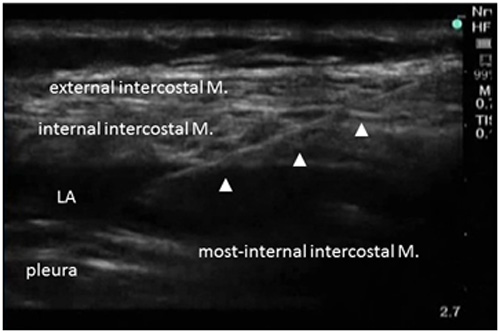
Figure 4: Ultrasound view during intercostal nerve block
LA = local anesthetic; ▲: block needle
LA is injected between internal intercostal muscle(M) and most-internal intercostal M.
should be identified. I insert the block needle by using an in-line approach. Then, a local anesthetic is injected between the internal intercostal muscle and the innermost internal intercostal muscle. If the innermost internal intercostal muscle is not identified, the anesthetic can be injected above the pleura. I use 5 mL of 0.375% ropivacaine for each intercostal space.
A recent study used liposomal bupivacaine for intercostal nerve blocks.7This technique offered post-operative pain scores comparable to those after thoracic epidural analgesia. Therefore, intercostal nerve block with liposomal bupivacaine may be considered a suitable alternative to epidural analgesia.
Another approach is interpleural administration of local anesthetics. A catheter is introduced percutaneously into the pleural space with the chest tube before the end of the procedure. Then, a large amount of anesthetic is infused intermittently or continuously, and the chest tubes are clamped for 5 to 30 min. This technique is easy and reliably places the catheter into the pleural space. However, the effects of this approach are limited. Chest tube management is essential.
NON-INTUBATED THORACIC SURGERY
Non-intubated thoracic surgery, which is also called awake thoracic surgery, is aimed at minimizing the risks of general anesthesia with one-lung ventilation.2 This technique is less invasive and does not require endotracheal intubation. Non-intubated thoracic surgery facilitates faster recovery and a shorter hospital stay. On the other hand, coughing, poor maneuverability due to diaphragmatic and lung movements, and patient movements are the limitations of this procedure. Therefore, the indications for this technique should be well considered with the surgeon and the patient.
Non-intubated thoracic surgery is technically more challenging than thoracic surgery under general anesthesia. Regional anesthesia plays a major role in this procedure. Awake video-assisted thoracic surgery has been performed with intercostal nerve blocks and local anesthetic infiltration at the incision site, while TPVB and epidural anesthesia are used for more invasive procedures.8Piccioni et al9 reported two cases of non-intubated thoracic surgeries with TPVB and concluded that the use of TPVB for video-assisted thoracoscopy resulted in adequate anesthesia with high levels of patient satisfaction.
In the near future, non-intubated thoracic surgery by regional anesthesia will play an increased role in the anesthetic management for thoracic surgery.
CONCLUSIONS
Regional anesthesia plays an important role in thoracic surgery, particularly with regard to post-operative pain control. The first choice of regional anesthesia for thoracic surgery is epidural analgesia or TPVB.In general, the analgesic efficiencies of epidural analgesia and TPVB are equivalent. However, TPVB has some advantages over epidural analgesia, including fewer complications. When these two blocks are contraindicated, intercostal nerve block or interpleural block should be considered.
Non-intubated thoracic surgery presents a challenge, and excellent regional anesthesia techniques facilitate the successful performance of this procedure.
REFERENCES
- Joshi GP, Bonnet F, Shah R, Wilkinson RC, Camu F, Fischer B, Neugebauer EAM, Rawal N, Schug SA, Simanski C, Kehlet H.A systematic review of randomized trials evaluating regional techniques for post-thoracotomy analgesia.AnesthAnalg 2008;107(3):1026-40. [PubMed]doi: 10.1213/01.ane.0000333274.63501.ff.
- Chen K-C, Cheng Y-J, Hung M-H, Tseng Y-D, Chen J-S.Nonintubatedthoracoscopic surgery using regional anesthesia and vagal block and targeted sedation.J Thorac Dis 2014;6(1):31-36. [PubMed][Free full text]doi: 10.3978/j.issn.2072-1439.2014.01.01.
- Baidya DK, Khanna P, Maitra S.Analgesic efficiency and safety of thoracic paravertebral and epidural analgesia for thoracic surgery: a systematic review and meta-analysis.Interactive Cardiovascular and Thoracic Surgery 2014;18:626-36. [PubMed][Free full text]doi: 10.1093/icvts/ivt551.
- Ding X, Jin S, Niu X, Ren H, Fu S, Li Q.A comparison of the analgesic efficacy and side effects of paravertebral compared with epidural blockade for thoracotomy: An updated meta-analysis.Plos One 2014;9:e96233
- Pintaric TS, Potocnik I, Hadzic A, Stupnik t, Pintraric M, Jankovic VN.Comparison of continuous thoracic epidural with paravertebral block on perioperative analgesia and hemodynamic stability in patients having open lung surgery.RegAnesth Pain Med 2011;36(3):256-60. [PubMed]doi: 10.1097/AAP.0b013e3182176f42.
- BolotinG, Lazarovici H, Uretzky G, Zlotnick AY, Tamir A, Saute M.The efficacy of intraoperative internal intercostal nerve block during video-assisted thoracic surgery on postoperative pain.Ann thoracSurg 2000;70(6):1872-5. [PubMed]
- Rice DC, Cata JP, Mena GE, Rodriguez-Restrepo A, Correa AM, Mehran RJ.Posterior intercostal nerve block with liposomal bupivacaine: An alternative to thoracic epidural analgesia.Ann ThoracSurg2015;99(6):1953-6. [PubMed]doi: 10.1016/j.athoracsur.2015.02.074.
- Kiss G, Castillo M.Non-intubated anesthesia in thoracic surgery – technical issues.Ann Transl Med 2015;3(8):109. [PubMed][Free full text]doi: 10.3978/j.issn.2305-5839.2015.05.01.
- Piccioni F, Langer M, Fumagalli L, Haeisler E, Conti B, Previtali P.Thoracic paravertebral anesthesia for awake video-assisted thoracoscopic surgery daily.Anesthesia 2010;65(12):1221-4. [PubMed]doi: 10.1111/j.1365-2044.2010.06420.x.