Sayed M. Abed 1, Ahmed M. Soliman 2, Mai M. Elrawas 3, Somia A. Elsheikh 4, Ahmed A. Abdallah 5, Reda H. Tabashy 6, Mahmoud A. Kamel 7
Author affiliations:
ABSTRACT
Background & objective: For managing acute postoperative pain is multimodal analgesia, including regional blocks. None of the regional techniques can block the whole breast innervation. Combining different blocks may address the inadequacy of existing methods. This study compared the perioperative analgesic efficacy of US-guided transversus thoracis muscle plane block (TTPB) combined with pectoralis nerve (PECS II) block versus PECS II block alone in patients subjected to modified radical mastectomy (MRM).
Methodology: This prospective randomized clinical trial involved 34 female patients scheduled for MRM under general anesthesia (GA). Patients were randomized into two equal groups: Combined Group (n=17) received TTPB and PECS II block, and PECS Group (n=17) received PECS II block 30 minutes before inducing GA. The primary outcome measure was the total postoperative opioid requirements. Secondary outcomes were postoperative pain, duration of analgesia, hemodynamic stability, and sedation.
Results: The total postoperative morphine consumption was significantly lower (P < 0.001), the duration of analgesia was significantly longer (P < 0.001), and the sedation score was significantly higher (P = 0.034) in the combined group than in the PECS Group . The pain scores were significantly lower in the combined group between 2 and 12 h. Both techniques showed hemodynamic stability, with lower heart rate and blood pressure in the combined group.
Conclusion: Adding TTPB to the PECS II block was superior to the PECS II block alone for patients undergoing MRM. The combined block reduced postoperative pain and morphine consumption. The patients were more well-sedated with improved hemodynamics.
Abbreviations: GA: general anesthesia, MRM: modified radical mastectomy, PECS II block: pectoralis nerve block, TTPB: transversus thoracis muscle plane block.
Keywords: Ultrasound; Transversus Thoracic; Pectoral Nerve Block; Modified Radical Mastectomy; Analgesia
Citation: Abed SM, Soliman AM, Elrawas MM, Elsheikh SAE, Abdallah AA, Tabashy RH, Kamel MA. Ultrasound guided pectoral nerve block with or without ultrasound guided transversus thoracic plane block in modified radical mastectomy; a randomized controlled trial. Anaesth. pain intensive care 2025;29(2):170-176. DOI: 10.35975/apic.v29i2.2700
Received: May 09, 2024; Reviewed: October 26, 2024; Accepted: January 01, 2025
Breast cancer ranked the first of all diagnosed malignancies in 2020 making up 11.7%.1 Surgical intervention is the primary therapy for patients with cancers localized to breast tissue.2 Postoperative pain hampers the patient's mental, physical, and social functioning and diminishes the quality of life.3 Sufficient postoperative pain management shortens the time needed for recovery and minimizes the duration of hospitalization.4 Moreover, prompt therapies effectively hinder the progression of chronic pain, which remains beyond the typical timeframe for relief.5
Regional analgesic methods are now considered an important part of the multimodal strategy for managing postoperative pain after breast surgery.6 Anesthetists consider paravertebral block (PVB) to be the established benchmark in this context.7
The PECS II block can be berformed by 2 injections: one is made between the pectoralis major and minor muscles, and the other is made between serratus anterior and pectoralis minor muscles. The target nerves are expanded to include the lateral cutaneous branches of the intercostal nerves (T2–T6). the intercostobrachial,medial cutaneous nerve of the arm and forearm, the long thoracic nerve and the thoracodorsal nerve.However, Anterior branches of the intercostal nerves from (T2–T6) remain unaffected.8
Anterior branches of the intercostal nerves from (T2–T6) can be blocked when LA is injected between the internal intercostal and transversus thoracis muscles by the transversus thoracis muscle plane (TTP) block.9
The intricate nature of breast innervation imposes anatomical constraints on using individual interfascial techniques. As a result, a combination of blocks is required to achieve comprehensive pain relief for numerous surgical procedures.10 Therefore, this research aimed to compare the perioperative analgesic efficacy of US-guided TTPB combined with PECS II block versus PECS block alone in patients subjected to modified radical mastectomy (MRM).
This prospective randomized clinical trial involved 34 female patients in the period from february 2022 to February 2024 after approval by the Ethical Committee of the National Cancer Institute, Cairo University, Egypt (AP 2202-30104). The study was registered in clinicaltrials.gov (NCT 06371625).Informed written consent was obtained from the participants.
Inclusion criteria were female aged 20-40 y and the ASA physical status II-III, scheduled for unilateral MRM for the treatment of the breast cancer.One of the criteria for exclusion was unwillingness to participate. Other criteria included previous transversus thoracic plane surgeries, body mass index (BMI) > 35 kg/m2, coagulation defect,unstable cardiovascular disease, history of psychiatric disorders, drug abuse, allergy to medication used,injection site infection and chronic pain syndrome.
A computer-generated sequence algorithm was used to randomly split the patients into two equal groups: the PECS Group (n=17) received US-guided PECS II block and the Combined Group (n=17) received US-guided TTPB.
Every patient underwent a thorough physical examination and history taking before the surgery.CBC, liver, renal functions, and coagulation tests are standard preoperative laboratory tests.
Patients received a preoperative dose of 2 mg of midazolam, 500 ml of lactated Ringer's solution was infused. The patients were closely observed using ECG, blood pressure, and pulse oximetry. Thirty minutes before to the surgical incision, the block was performed as needed utilizing a high frequency linear probe (6–13 MHz) of SonoSite M-Turbo (FUGIFILM, USA). Following the completion of the nerve blocks, the sensory block was assessed using cold perception in thoracic segments from T1 to T12, and the onset of the block was recorded. Then, US scanning was done to exclude pneumothorax after the block procedure in both groups. The patient and the data collector were blinded to the type of block.
2.1. Transversus thoracic plane block (TTPB)
The ultrasonic probe counted from the T2-T5 intercostal space and was positioned at a sagittal plane to the sternum. After being turned 90 degrees, the probe was positioned between the fourth and fifth costal cartilages, which join at the sternum close to the nipple.The transversus thoracic muscle and the internal intercostal muscle were identified. A 20G 100 mm echogenic needle was inserted from lateral to medial direction (in-plane approach) and placed between the intercostal muscles and transversus thoracic muscle. A bolus dose of 0.25% bupivacaine 20 ml was administered, hydrodissection and/or downward displacement of pleura was observed.

2.2. Modified pectoral nerve (PECS II) block
The right arm rotated outward and abducted ninety-five degrees.The probe was positioned beneath the clavicle's lateral third. Once the axillary artery and vein and the subclavian artery have been located, the probe was moved distally and laterally until space between the 2nd and 3rd rib was reached. until the pectoralis major muscle was identified. A 20G 100 mm echogenic needle was inserted between pectrolis muscles, To prevent intravascular injection, 20 ml of LA was administered in 5 cc increments, with aspiration following each 5 cc.The probe was moved distally and laterally until space between the 3rd and 4th ribs was reached. The fascial plane between the pectoralis minor and serratus anterior muscles was opened, and 10 ml of LA was injected in 5 cc increments.
2.3. General anesthesia
Before the patients were put under anesthesia, they had their ECG, NIBP, and SpO2 checked when they arrived in the operating room. the baseline values of oxygen saturation (SpO2), (HR), and (MAP). EtCO2 was tracked when anesthesia was induced. Propofol 1.5–2 mg/kg, fentanyl 1 µg/kg, and atracurium 0.5 mg/kg were used for induction. To keep MAP and HR values within 30% of baseline vital signs, further boluses of fentanyl (0.3 µg/kg) and atracurium (0.1–0.2 mg/kg every 30 minutes) were given. In accordance with fluid chart maintenance, deficit, third space loss, urine output, and blood loss, the lactated ringer's solution was transfused.
2.4. Postoperative care
All patients received the postoperative pain regimen within the first 24 h following surgery, which included intravenous administration of 1 gm paracetamol every 6 h and intravenous administration of 30 mg ketorolac every 8 h. If the patient requested more analgesia or if the VAS score at rest was > 3, 3 mg of morphine was provided as rescue analgesia. Intravenous administration of ondansetron 4 mg was administered in cases of nausea, whether or not vomiting occurred.
Additional medication or technique-related problems, including procedure-induced pneumothorax, LA toxicity, puncture site hematomas, and respiratory depression, were noted.
The total amount of opioids needed in the first twenty-four h following surgery served as the main primary outcome measure. The secondary outcomes were the duration of analgesia, hemodynamic stability, sedation (measured by Ramsay score), nausea and vomiting, and postoperative pain score using a visual analog scale (VAS, 0–10 mm; 0 = no pain and 10 = greatest severe pain). The amount of time between the end of surgery and the initial request for analgesia was called the duration of analgesia.
2.5. Sample size calculation
Assuming a true difference in means between the test and the reference group of 1.5 units, and a pooled standard deviation of 4 units, the study would require a sample size of 17 for each group (i.e. a total sample size of 34) to achieve a power of 80% and a level of significance of 5%, for declaring that the test drug is superior to the active control drug at -2 units margin of superiority (assuming that a smaller mean is desirable).
2.6. Statistical analysis
IBM© SPSS© Statistics version 27 (IBM© Corp., Armonk, NY, USA) was used for statistical analysis. When specified, quantitative data were presented as mean ± standard deviation (SD) or median (range). Frequency and percentage were used to express qualitative data. Dependinng o the data distribution, the independent-sample t-test or the Mann-Whitney U test was employed to compare numericaal dta between two groups. To compare qualitative variables, the Chi-square test was employed. Every test had two tails, and a significant p-value was defined as one less than 0.05.
53 patients had their eligibility evaluated; 11 of them did not fit the requirements, and 8 of them declined to take part in the research. After being divided into the two groups, the remaining 34 patients underwent statistical analysis (Figure 1).
Regarding age, BMI, and ASA class, there was no discernible difference between the two groups (Table 1).
The duration of the block performance was significantly longer (P < 0.001) in the combined group (13.1 ± 1.3) than PECS group (8.3 ± 1.2). The time to onset of the block was comparable between the two groups (P = 0.768).
The total morphine consumption in the first 24 postoperative h was significantly lower (P < 0.001) in the combined group than the PECS group (Table 2). The duration of analgesia was significantly longer (P < 0.001) in the combined group than the PECS Group (Table 2).
The Ramsey sedation score was significantly higher (P = 0.034) in the combined group than the PECS Group (Table 2).
Table 3 shows a statistically significant difference between the two groups in VAS score between 2 and 12 h, while the difference was not significant immediately postoperative and after 24 h.
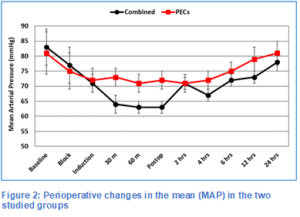
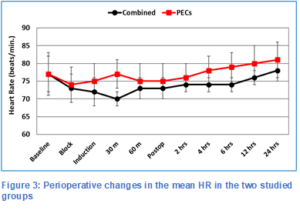
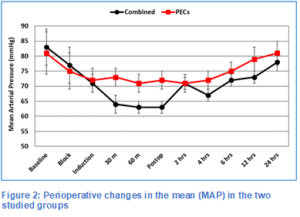
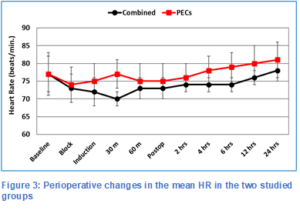
Figures 2 and 3 show the intra- and postoperative MAP and HR. The MAP was comparable at baseline and up to skin incision, then it was lower in the combined group during the remaining intraoperative period. Immediately postoperative, there was no significant difference in MAP between the two groups (P = 0.392). Then, it was lower in the combined group up to 12 h, but it became comparable after 24 h. The HR showed almost the same pattern of change and intergroup differences.
The gold standard for managing acute postoperative pain is multimodal analgesia, which fundamentally includes infiltration procedures utilizing local anesthetics (LA) and regional anesthesia methods.11
This study demonstrated that the combination of two interfascial plane blocks, PECS II and TTP blocks was associated with reduced total postoperative morphine consumption, longer duration of analgesia, reduced pain scores, better sedation, and consequently slower HR and lower MAP when compared to PECS II alone
PECS II blockade is the most widely used postoperative analgesia technique for breast cancer patients.12 It reduces opioid requirement and pain intensity, making it a more effective alternative to general anesthesia (GA) procedures.13,14 The LA is situated between the pectoralis minor and the serratus anterior as an additional fascial plane in PECS II. Alongside a blockade of the pectoral nerves, the intercostal nerves are anesthetized from the T2 to T5 levels, as well as the long thoracic nerve.13 PECS II block is not expected to anesthetize the anterior cutaneous branches (ACBs) of the intercostal nerves, which emerge close to the sternum. As such, it is anticipated that a PECS II block will not eliminate the medial breast's sensory innervation.15
In the TTP block, the local anesthetic is injected Between the internal intercostal muscle and the transversus thoracis muscle.9 The T2-T6 intercostal nerves were specifically covered by the TTP block according to the first cadaveric research guided by ultrasonography. This new method may be able to offer analgesia for anterior chest wall surgery because the ACBs of the intercostal nerves have a major impact on the sensory innervation of the internal mammary region.16
In a recent randomized trial by Zhao Y, et al. in patients undergoing MRM, the PECS-TTP combination showed a superior analgesic profile than TPVB.17 This combined regional block exhibited a prolonged analgesic duration and reduced perioperative opioids and extra-analgesics compared to the TPVB group. Moreover, the inflammatory response and the VAS scores at rest, during activity, were decreased in the TTP-PECS group relative to the TPVB group after 12 h postoperatively.
Arasu T, et al. carried out a prospective, randomized, comparative pilot study in which thirty adult patients undergoing cardiac implanted electronic device (CIED) insertion between the ages of 18 and 85 were recruited for the study.18 It was discovered that, in comparison to PECS1 block alone, combined PECS1 and TTM blocks offer better analgesia and a lower net intake of sedatives, rescue analgesics, and local anesthetics.
TTP-PECS block combination can reduce pain, speed up recovery, regulate hemodynamic level, and lessen stress responses in patients following radical mastectomy, according to a study by Li J, et al.19
According to a research by Alshaimaa, et al. combined PECS II-TTP blocks offered postoperative analgesia that was more efficient and durable than SAP blocks.20 Moreover, they took less morphine after surgery and postponed the first analgesic administration (median 8 h) as opposed to SAP block (median 6 h); however, there were no discernible variations between the groups in terms of intraoperative fentanyl consumption, patient satisfaction, or complications.
Patients who underwent pectoral nerve block experienced much less discomfort throughout their PACU stay than patients who received placebo block, according to a prospective randomized study conducted by Barbara Versyck, et al. involving 140 breast cancer patients.21 In addition, compared to patients in the placebo group, patients in the PECS group needed much less postsurgical opioid delivery interventions and postoperative opioids.
Nonetheless, our study possesses multiple limitations. Despite the randomized double-blinded nature of the study, the small sample size analyzed might hinder the generalization of the results. Besides, the study was a single-center analysis. We conducted only a thorough evaluation of several short-term indicators of pain and analgesic requirements within 24 h.
When used with GA for breast procedures, pectoralis nerve block and the transversus thoracis plane block provide exceptional analgesia. Having easily identifiable landmarks based on basic anatomical and ultrasonography expertise, these procedures are straightforward and quick to learn, offering a great substitute for the traditional thoracic paravertebral and neuraxial blocks used in breast surgery. For patients undergoing MRM operations, pectoralis nerve plus transversus thoracis plane block resulted in reduced morphine intake and better intraoperative and postoperative analgesic control than pectoralis nerve block alone.
7. Data availability
The numerical data generated during this research is available with the authors.
8. Funding
The study utilized the hospital resources only, and no external or industry funding was involved.
9. Conflict of interest
The authors declare no conflicts of interest.
10. Authors’ contribution
SMA, MAK: Conduct of study and manuscript editing
AMS: statistical analysis
MME, SAE: literature search
AAA: statistical analysis and manuscript editing
RHT: conduct of study
Author affiliations:
- Sayed Mahmoud Abed, Assistant Professor, Department of Anesthesia, Intensive Care & Pain Management, National Cancer Institute, Cairo University, Cairo, Egypt; Email: sydabed2020@outlook.com
- Ahmed Mohamed Soliman, Lecturer, Department of Anesthesia, Intensive Care & Pain Management, National Cancer Institute, Cairo University, Cairo, Egypt; Email: ams21787arif@hotmail.com
- Mai Mohamed Elrawas, Lecturer, Department of Anesthesia, Intensive Care & Pain Management, National Cancer Institute, Cairo University, Cairo, Egypt; Email: elrawas@nci.cu.edu.eg
- Somia Abd El Aziz Elsheikh, Professor, Department of Anesthesia, Intensive Care & Pain Management, National Cancer Institute, Cairo University, Cairo, Egypt; Email: Somaya_elshaikh@outlook.com
- Ahmed Abdo Abdallah, Demonstrator, Department of Anesthesia & Pain Management, Faculty of Medicine, Ain Shams University, Cairo, Egypt; Email: pprrooff2@yahoo.com
- Reda Hasan Tabashy, Professor, Department of Diagnostic Radiology, National Cancer Institute, Cairo University, Cairo, Egypt. Email: tabashy@cu.edu.eg
- Mahmoud Ahmed Kamel, Assistant Professor, Department of Anesthesia, Intensive Care & Pain Management, National Cancer Institute, Cairo University, Cairo, Egypt; Email: Mkamel_76@hotmail.com
ABSTRACT
Background & objective: For managing acute postoperative pain is multimodal analgesia, including regional blocks. None of the regional techniques can block the whole breast innervation. Combining different blocks may address the inadequacy of existing methods. This study compared the perioperative analgesic efficacy of US-guided transversus thoracis muscle plane block (TTPB) combined with pectoralis nerve (PECS II) block versus PECS II block alone in patients subjected to modified radical mastectomy (MRM).
Methodology: This prospective randomized clinical trial involved 34 female patients scheduled for MRM under general anesthesia (GA). Patients were randomized into two equal groups: Combined Group (n=17) received TTPB and PECS II block, and PECS Group (n=17) received PECS II block 30 minutes before inducing GA. The primary outcome measure was the total postoperative opioid requirements. Secondary outcomes were postoperative pain, duration of analgesia, hemodynamic stability, and sedation.
Results: The total postoperative morphine consumption was significantly lower (P < 0.001), the duration of analgesia was significantly longer (P < 0.001), and the sedation score was significantly higher (P = 0.034) in the combined group than in the PECS Group . The pain scores were significantly lower in the combined group between 2 and 12 h. Both techniques showed hemodynamic stability, with lower heart rate and blood pressure in the combined group.
Conclusion: Adding TTPB to the PECS II block was superior to the PECS II block alone for patients undergoing MRM. The combined block reduced postoperative pain and morphine consumption. The patients were more well-sedated with improved hemodynamics.
Abbreviations: GA: general anesthesia, MRM: modified radical mastectomy, PECS II block: pectoralis nerve block, TTPB: transversus thoracis muscle plane block.
Keywords: Ultrasound; Transversus Thoracic; Pectoral Nerve Block; Modified Radical Mastectomy; Analgesia
Citation: Abed SM, Soliman AM, Elrawas MM, Elsheikh SAE, Abdallah AA, Tabashy RH, Kamel MA. Ultrasound guided pectoral nerve block with or without ultrasound guided transversus thoracic plane block in modified radical mastectomy; a randomized controlled trial. Anaesth. pain intensive care 2025;29(2):170-176. DOI: 10.35975/apic.v29i2.2700
Received: May 09, 2024; Reviewed: October 26, 2024; Accepted: January 01, 2025
1. INTRODUCTION
Breast cancer ranked the first of all diagnosed malignancies in 2020 making up 11.7%.1 Surgical intervention is the primary therapy for patients with cancers localized to breast tissue.2 Postoperative pain hampers the patient's mental, physical, and social functioning and diminishes the quality of life.3 Sufficient postoperative pain management shortens the time needed for recovery and minimizes the duration of hospitalization.4 Moreover, prompt therapies effectively hinder the progression of chronic pain, which remains beyond the typical timeframe for relief.5
Regional analgesic methods are now considered an important part of the multimodal strategy for managing postoperative pain after breast surgery.6 Anesthetists consider paravertebral block (PVB) to be the established benchmark in this context.7
The PECS II block can be berformed by 2 injections: one is made between the pectoralis major and minor muscles, and the other is made between serratus anterior and pectoralis minor muscles. The target nerves are expanded to include the lateral cutaneous branches of the intercostal nerves (T2–T6). the intercostobrachial,medial cutaneous nerve of the arm and forearm, the long thoracic nerve and the thoracodorsal nerve.However, Anterior branches of the intercostal nerves from (T2–T6) remain unaffected.8
Anterior branches of the intercostal nerves from (T2–T6) can be blocked when LA is injected between the internal intercostal and transversus thoracis muscles by the transversus thoracis muscle plane (TTP) block.9
The intricate nature of breast innervation imposes anatomical constraints on using individual interfascial techniques. As a result, a combination of blocks is required to achieve comprehensive pain relief for numerous surgical procedures.10 Therefore, this research aimed to compare the perioperative analgesic efficacy of US-guided TTPB combined with PECS II block versus PECS block alone in patients subjected to modified radical mastectomy (MRM).
2. METHODOLOGY
This prospective randomized clinical trial involved 34 female patients in the period from february 2022 to February 2024 after approval by the Ethical Committee of the National Cancer Institute, Cairo University, Egypt (AP 2202-30104). The study was registered in clinicaltrials.gov (NCT 06371625).Informed written consent was obtained from the participants.
Inclusion criteria were female aged 20-40 y and the ASA physical status II-III, scheduled for unilateral MRM for the treatment of the breast cancer.One of the criteria for exclusion was unwillingness to participate. Other criteria included previous transversus thoracic plane surgeries, body mass index (BMI) > 35 kg/m2, coagulation defect,unstable cardiovascular disease, history of psychiatric disorders, drug abuse, allergy to medication used,injection site infection and chronic pain syndrome.
A computer-generated sequence algorithm was used to randomly split the patients into two equal groups: the PECS Group (n=17) received US-guided PECS II block and the Combined Group (n=17) received US-guided TTPB.
Every patient underwent a thorough physical examination and history taking before the surgery.CBC, liver, renal functions, and coagulation tests are standard preoperative laboratory tests.
Patients received a preoperative dose of 2 mg of midazolam, 500 ml of lactated Ringer's solution was infused. The patients were closely observed using ECG, blood pressure, and pulse oximetry. Thirty minutes before to the surgical incision, the block was performed as needed utilizing a high frequency linear probe (6–13 MHz) of SonoSite M-Turbo (FUGIFILM, USA). Following the completion of the nerve blocks, the sensory block was assessed using cold perception in thoracic segments from T1 to T12, and the onset of the block was recorded. Then, US scanning was done to exclude pneumothorax after the block procedure in both groups. The patient and the data collector were blinded to the type of block.
2.1. Transversus thoracic plane block (TTPB)
The ultrasonic probe counted from the T2-T5 intercostal space and was positioned at a sagittal plane to the sternum. After being turned 90 degrees, the probe was positioned between the fourth and fifth costal cartilages, which join at the sternum close to the nipple.The transversus thoracic muscle and the internal intercostal muscle were identified. A 20G 100 mm echogenic needle was inserted from lateral to medial direction (in-plane approach) and placed between the intercostal muscles and transversus thoracic muscle. A bolus dose of 0.25% bupivacaine 20 ml was administered, hydrodissection and/or downward displacement of pleura was observed.

2.2. Modified pectoral nerve (PECS II) block
The right arm rotated outward and abducted ninety-five degrees.The probe was positioned beneath the clavicle's lateral third. Once the axillary artery and vein and the subclavian artery have been located, the probe was moved distally and laterally until space between the 2nd and 3rd rib was reached. until the pectoralis major muscle was identified. A 20G 100 mm echogenic needle was inserted between pectrolis muscles, To prevent intravascular injection, 20 ml of LA was administered in 5 cc increments, with aspiration following each 5 cc.The probe was moved distally and laterally until space between the 3rd and 4th ribs was reached. The fascial plane between the pectoralis minor and serratus anterior muscles was opened, and 10 ml of LA was injected in 5 cc increments.
2.3. General anesthesia
Before the patients were put under anesthesia, they had their ECG, NIBP, and SpO2 checked when they arrived in the operating room. the baseline values of oxygen saturation (SpO2), (HR), and (MAP). EtCO2 was tracked when anesthesia was induced. Propofol 1.5–2 mg/kg, fentanyl 1 µg/kg, and atracurium 0.5 mg/kg were used for induction. To keep MAP and HR values within 30% of baseline vital signs, further boluses of fentanyl (0.3 µg/kg) and atracurium (0.1–0.2 mg/kg every 30 minutes) were given. In accordance with fluid chart maintenance, deficit, third space loss, urine output, and blood loss, the lactated ringer's solution was transfused.
2.4. Postoperative care
All patients received the postoperative pain regimen within the first 24 h following surgery, which included intravenous administration of 1 gm paracetamol every 6 h and intravenous administration of 30 mg ketorolac every 8 h. If the patient requested more analgesia or if the VAS score at rest was > 3, 3 mg of morphine was provided as rescue analgesia. Intravenous administration of ondansetron 4 mg was administered in cases of nausea, whether or not vomiting occurred.
Additional medication or technique-related problems, including procedure-induced pneumothorax, LA toxicity, puncture site hematomas, and respiratory depression, were noted.
The total amount of opioids needed in the first twenty-four h following surgery served as the main primary outcome measure. The secondary outcomes were the duration of analgesia, hemodynamic stability, sedation (measured by Ramsay score), nausea and vomiting, and postoperative pain score using a visual analog scale (VAS, 0–10 mm; 0 = no pain and 10 = greatest severe pain). The amount of time between the end of surgery and the initial request for analgesia was called the duration of analgesia.
2.5. Sample size calculation
Assuming a true difference in means between the test and the reference group of 1.5 units, and a pooled standard deviation of 4 units, the study would require a sample size of 17 for each group (i.e. a total sample size of 34) to achieve a power of 80% and a level of significance of 5%, for declaring that the test drug is superior to the active control drug at -2 units margin of superiority (assuming that a smaller mean is desirable).
2.6. Statistical analysis
IBM© SPSS© Statistics version 27 (IBM© Corp., Armonk, NY, USA) was used for statistical analysis. When specified, quantitative data were presented as mean ± standard deviation (SD) or median (range). Frequency and percentage were used to express qualitative data. Dependinng o the data distribution, the independent-sample t-test or the Mann-Whitney U test was employed to compare numericaal dta between two groups. To compare qualitative variables, the Chi-square test was employed. Every test had two tails, and a significant p-value was defined as one less than 0.05.
| Table 1: Baseline characteristics and block data of the two studied groups | |||
| Parameter | Combined Group
(n=17) |
PECS Group
(n=17) |
P-value |
| Age (years) | 46.1 ± 6.9 | 45.8 ± 7.8 | 0.926 |
| Body mass index (kg/m2) | 29.5 ± 2.2 | 28.7 ± 1.4 | 0.237 |
| ASA Class (II/III) | 13/4 | 14/3 | 0.761 |
| Procedure duration (min) | 13.1 ± 1.3 | 8.3 ± 1.2 | < 0.001 |
| Time to onset of block (min) | 6.4 ± 0.9 | 6.5 ± 1.3 | 0.768 |
| Data are presented as mean ± SD; P < 0.05 considered as significant
ASA: American Society of Anesthesiologists |
|||
| Table 2: Comparison between groups regarding the time of 1st rescue analgesia, total opioid consumption, and sedation scores | |||
| Parameter | Combined Group
(n=17) |
PECS Group
(n=17) |
P-value |
| Time of 1st rescue analgesia (h) | 11.0 ± 0.6 | 8.3 ± 0.7 | < 0.001 |
| Total rescue morphine used (mg) | 8.6 ± 0.8 | 12.9 ± 1.1 | < 0.001 |
| Ramsay Sedation Score | 3 (2-4) | 2 (2-3) | 0.034 |
| Data are presented as mean ± SD or median (Range); P < 0.05 considered as significant | |||
| Table 3: The pain VAS score at rest in the two studied groups | |||
| Time | Combined Group
(n=17) |
PECS Group
(n=17) |
P-value |
| Immediate | 3 (2-4) | 4 (3-4) | 0.160 |
| 2 h | 3 (1-4) | 4 (2-6) | 0.026 |
| 4 h | 3 (1-4) | 4 (3-4) | 0.016 |
| 6 h | 4 (2-6) | 4 (3-7) | 0.018 |
| 12 h | 4 (2-5) | 5 (4-6) | 0.034 |
| 24 h | 5 (5-7) | 5 (3-7) | 0.708 |
| Data are presented as median (Range); P < 0.05 considered as significant | |||
3. RESULTS
53 patients had their eligibility evaluated; 11 of them did not fit the requirements, and 8 of them declined to take part in the research. After being divided into the two groups, the remaining 34 patients underwent statistical analysis (Figure 1).
Regarding age, BMI, and ASA class, there was no discernible difference between the two groups (Table 1).
The duration of the block performance was significantly longer (P < 0.001) in the combined group (13.1 ± 1.3) than PECS group (8.3 ± 1.2). The time to onset of the block was comparable between the two groups (P = 0.768).
The total morphine consumption in the first 24 postoperative h was significantly lower (P < 0.001) in the combined group than the PECS group (Table 2). The duration of analgesia was significantly longer (P < 0.001) in the combined group than the PECS Group (Table 2).
The Ramsey sedation score was significantly higher (P = 0.034) in the combined group than the PECS Group (Table 2).
Table 3 shows a statistically significant difference between the two groups in VAS score between 2 and 12 h, while the difference was not significant immediately postoperative and after 24 h.
Figures 2 and 3 show the intra- and postoperative MAP and HR. The MAP was comparable at baseline and up to skin incision, then it was lower in the combined group during the remaining intraoperative period. Immediately postoperative, there was no significant difference in MAP between the two groups (P = 0.392). Then, it was lower in the combined group up to 12 h, but it became comparable after 24 h. The HR showed almost the same pattern of change and intergroup differences.
4. DISCUSSION
The gold standard for managing acute postoperative pain is multimodal analgesia, which fundamentally includes infiltration procedures utilizing local anesthetics (LA) and regional anesthesia methods.11
This study demonstrated that the combination of two interfascial plane blocks, PECS II and TTP blocks was associated with reduced total postoperative morphine consumption, longer duration of analgesia, reduced pain scores, better sedation, and consequently slower HR and lower MAP when compared to PECS II alone
PECS II blockade is the most widely used postoperative analgesia technique for breast cancer patients.12 It reduces opioid requirement and pain intensity, making it a more effective alternative to general anesthesia (GA) procedures.13,14 The LA is situated between the pectoralis minor and the serratus anterior as an additional fascial plane in PECS II. Alongside a blockade of the pectoral nerves, the intercostal nerves are anesthetized from the T2 to T5 levels, as well as the long thoracic nerve.13 PECS II block is not expected to anesthetize the anterior cutaneous branches (ACBs) of the intercostal nerves, which emerge close to the sternum. As such, it is anticipated that a PECS II block will not eliminate the medial breast's sensory innervation.15
In the TTP block, the local anesthetic is injected Between the internal intercostal muscle and the transversus thoracis muscle.9 The T2-T6 intercostal nerves were specifically covered by the TTP block according to the first cadaveric research guided by ultrasonography. This new method may be able to offer analgesia for anterior chest wall surgery because the ACBs of the intercostal nerves have a major impact on the sensory innervation of the internal mammary region.16
In a recent randomized trial by Zhao Y, et al. in patients undergoing MRM, the PECS-TTP combination showed a superior analgesic profile than TPVB.17 This combined regional block exhibited a prolonged analgesic duration and reduced perioperative opioids and extra-analgesics compared to the TPVB group. Moreover, the inflammatory response and the VAS scores at rest, during activity, were decreased in the TTP-PECS group relative to the TPVB group after 12 h postoperatively.
Arasu T, et al. carried out a prospective, randomized, comparative pilot study in which thirty adult patients undergoing cardiac implanted electronic device (CIED) insertion between the ages of 18 and 85 were recruited for the study.18 It was discovered that, in comparison to PECS1 block alone, combined PECS1 and TTM blocks offer better analgesia and a lower net intake of sedatives, rescue analgesics, and local anesthetics.
TTP-PECS block combination can reduce pain, speed up recovery, regulate hemodynamic level, and lessen stress responses in patients following radical mastectomy, according to a study by Li J, et al.19
According to a research by Alshaimaa, et al. combined PECS II-TTP blocks offered postoperative analgesia that was more efficient and durable than SAP blocks.20 Moreover, they took less morphine after surgery and postponed the first analgesic administration (median 8 h) as opposed to SAP block (median 6 h); however, there were no discernible variations between the groups in terms of intraoperative fentanyl consumption, patient satisfaction, or complications.
Patients who underwent pectoral nerve block experienced much less discomfort throughout their PACU stay than patients who received placebo block, according to a prospective randomized study conducted by Barbara Versyck, et al. involving 140 breast cancer patients.21 In addition, compared to patients in the placebo group, patients in the PECS group needed much less postsurgical opioid delivery interventions and postoperative opioids.
5. LIMITATIONS
Nonetheless, our study possesses multiple limitations. Despite the randomized double-blinded nature of the study, the small sample size analyzed might hinder the generalization of the results. Besides, the study was a single-center analysis. We conducted only a thorough evaluation of several short-term indicators of pain and analgesic requirements within 24 h.
6. CONCLUSION
When used with GA for breast procedures, pectoralis nerve block and the transversus thoracis plane block provide exceptional analgesia. Having easily identifiable landmarks based on basic anatomical and ultrasonography expertise, these procedures are straightforward and quick to learn, offering a great substitute for the traditional thoracic paravertebral and neuraxial blocks used in breast surgery. For patients undergoing MRM operations, pectoralis nerve plus transversus thoracis plane block resulted in reduced morphine intake and better intraoperative and postoperative analgesic control than pectoralis nerve block alone.
7. Data availability
The numerical data generated during this research is available with the authors.
8. Funding
The study utilized the hospital resources only, and no external or industry funding was involved.
9. Conflict of interest
The authors declare no conflicts of interest.
10. Authors’ contribution
SMA, MAK: Conduct of study and manuscript editing
AMS: statistical analysis
MME, SAE: literature search
AAA: statistical analysis and manuscript editing
RHT: conduct of study
11. REFERENCES
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. [PubMed] DOI: 3322/caac.21660
- Sinnadurai S, Kwong A, Hartman M, Tan EY, Bhoo-Pathy NT, Dahlui M, et al. Breast-conserving surgery versus mastectomy in young women with breast cancer in Asian settings. BJS Open. 2019;3:48–55. [PubMed] DOI: 1002/bjs5.50111
- Quadt L, Esposito G, Critchley HD, Garfinkel SN. Brain-body interactions underlying the association of loneliness with mental and physical health. Neurosci Biobehav Rev. 2020;116:283–300. [PubMed] DOI: 1016/j.neubiorev.2020.06.015
- Yousuf MS, Sohail I, Bhatti S, Cox J. Improving postoperative analgesia in after mastectomy: Is now the time for an international randomized controlled trial? Breast J. 2020;26:1464–5. [PubMed] DOI: 1111/tbj.13732
- Raffaeli W, Arnaudo E. Pain as a disease: an overview. J Pain Res. 2017;10:2003–8. [PubMed] DOI: 2147/JPR.S138864
- Wong HY, Pilling R, Young BWM, Owolabi AA, Onwochei DN, Desai N. Comparison of local and regional anesthesia modalities in breast surgery: A systematic review and network meta-analysis. J Clin Anesth. 2021;72:110274. [PubMed] DOI: 1016/j.jclinane.2021.110274
- Terkawi AS, Tsang S, Sessler DI, Terkawi RS, Nunemaker MS, Durieux ME, et al. Improving analgesic efficacy and safety of thoracic paravertebral block for breast surgery: A mixed-effects meta-analysis. Pain Physician. 2015;18:E757–80. [PubMed]
- Blanco R, Fajardo M, Parras Maldonado T. Ultrasound description of Pecs II (modified Pecs I): a novel approach to breast surgery. Rev Esp Anestesiol Reanim. 2012;59:470–5. [PubMed] DOI: 1016/j.redar.2012.07.003
- Nakanishi T, Yoshimura M, Toriumi T. Pectoral nerve II block, transversus thoracic muscle plane block, and dexmedetomidine for breast surgery in a patient with achondroplasia: a case report. JA Clin Rep. 2019;5:47. [PubMed] DOI: 1186/s40981-019-0267-5
- de la Torre PA, García PD, Alvarez SL, Miguel FJG, Pérez MF. A novel ultrasound-guided block: a promising alternative for breast analgesia. Aesthet Surg J. 2014;34:198–200. [PubMed] DOI: 1177/1090820X13515902
- Misiołek H, Zajączkowska R, Daszkiewicz A, Woroń J, Dobrogowski J, Wordliczek J, et al. Postoperative pain management 2018 – consensus statement. Anaesthesiol Intensive Ther. 2018;50:173–99. [PubMed] DOI: 5603/AIT.2018.0026
- Gola W, Białka S, Andrzejewska A, Palaczynski P, Misiołek H. Fascial plane blocks for breast surgery – current state of knowledge. Anaesthesiol Intensive Ther. 2022;54:262. [PubMed] DOI: 5114/ait.2022.119220
- Cassai AD, Bonanno C, Sandei L, Finozzi F, Carron M, Marchet A. PECS II block is associated with lower incidence of chronic pain after breast surgery. Korean J Pain. 2019;32:286–91. [PubMed] DOI: 3344/kjp.2019.32.4.286
- Ameta N, Ramkiran S, Vivekanand D, Honwad M, Jaiswal A, Gupta MK. Comparison of the efficacy of ultrasound-guided pectoralis-II block and intercostal approach to paravertebral block among patients undergoing conservative breast surgery: A randomized control study. J Anaesthesiol Clin Pharmacol. 2023;39:488–96. [PubMed] DOI: 4103/joacp.joacp_411_21
- Woodworth GE, Ivie RMJ, Nelson SM, Walker CM, Maniker RB. Perioperative breast analgesia: A qualitative review of anatomy and regional techniques. Reg Anesth Pain Med. 2017;42:609–31. [PubMed] DOI: 1097/AAP.0000000000000641
- Fujii S, Bairagi R, Roche M, Zhou JR. Transversus thoracis muscle plane block. Biomed Res Int. 2019;2019:1716365. [PubMed] DOI: 1155/2019/1716365
- Zhao Y, Jin W, Pan P, Feng S, Fu D, Yao J. Ultrasound-guided transversus thoracic muscle plane-pectoral nerve block for postoperative analgesia after modified radical mastectomy: A comparison with the thoracic paravertebral nerve block. Perioper Med (Lond). 2022;11:39. [PubMed] DOI: 1186/s13741-022-00270-3
- Arasu T, Ragavendran S, Nagaraja PS, Singh NG, Vikram MN, Basappanavar VS. Comparison of pectoral nerve (PECS1) block with combined PECS1 and transversus thoracis muscle (TTM) block in patients undergoing cardiac implantable electronic device insertion – A pilot study. Ann Card Anaesth. 2020;23:165–9. [PubMed] DOI: 4103/aca.ACA_255_18
- Li J, Lyu Q, Su W, Li M, Du Y, Hu Y. A randomized trial: Effects of different anesthesia methods on early perioperative pain sensitivity and cellular immune function in patients undergoing radical mastectomy. Gland Surg. 2021;10:2246–54. [PubMed] DOI: 21037/gs-21-343
- Alasrag AS, Elkeblawy AM, Abo Elyazid MME, Ezz HAA. Analgesic efficacy of ultrasound-guided PECS II and transversus thoracic plane blocks compared to serratus anterior plane block for modified radical mastectomy: A randomized prospective study. Egypt J Anaesth. 2023;39:218–25. DOI: 1080/11101849.2023.2182991
- Versyck B, van Geffen GJ, Van Houwe P. Prospective double-blind randomized placebo-controlled clinical trial of the pectoral nerves (PECS) block type II. J Clin Anesth. 2017;40:46–50. [PubMed] DOI: 1016/j.jclinane.2017.03.054