TRAN Van Dang1, Nguyen Do Hung2, Nguyen Xuan Quang3, Tu Huu Nguyen4, Duc Viet Tran5, VU Hoang Phuong6
Author affiliations:
Background: Postoperative pain often remains troublesome for the patients, if not adequately managed. Various modalities have been tried to keep the patient pain free. Regional nerve blocks under ultrasound guidance have recently gained much popularity. We aimed to compare the pain relief outcomes after hip replacement surgery by continuous Pericapsular Nerve Group Block (PENG Block) in combination with lateral femoral cutaneous nerve (LFCN) block under the guidance of ultrasound versus patient-controlled intravenous analgesia (PCA).
Methodology: Sixty patients, who underwent hip surgery at E University Hospital, Hanoi, Vietnam, from August 2021 to August 2022, were randomly allocated to one of the two groups: group of patients with pain relief with PENG block in combination with LFCN block (PENG group) and the group of patients with patient-controlled intravenous analgesia (PCA group). Outcomes regarding clinical parameters and pain scores on Visual Analogue Scale (VAS), from the initiation of the blocks or the PCA (H0) to 72 h (H72) were recorded and compared.
Results: Sixty patients were included in this study. The average VAS scores at rest in both groups was at low pain level (VAS < 4). The average VAS score in both of the groups at most of the time of the study did not have a statistically significant difference. The VAS on movement at the time points H18, H21, H24, H30, H36, H48, H72 of the PENG group was lower than that of the PCA group and the difference was statistically significant between the two groups (P < 0.05). The rate of vomiting/nausea of patients in the PCA group was significantly higher than in the PENG group (P = 0.006).
Conclusion: Pericapsular nerve block combined with lateral femoral cutaneous nerve block offers prolonged pain relief when compared with traditional patient-controlled intravenous analgesia in postoperative pain relief after hip replacement, and is associated with lower frequency of vomiting/nausea.
Abbreviations: ASA - American Society of Anesthesiologists; AIIS - Anterior Inferior Iliac Spine; IPE - Iliopubic Eminence; LFCN - Lateral Femoral Cutaneous Nerve; PCA - Patient-Controlled Analgesia; PENG - Pericapsular Nerve Group; VAS - Visual Analogue Scale.
Keywords: Pericapsular nerve group block; Lateral femoral cutaneous nerve; Hip replacement; Multimodal analgesia; Ultrasound-guided analgesia; Patient-controlled analgesia; Side effects.
Citation: Dang TV, Hung ND, Quangm NX, Nguyen TH, Tran DV, VU Hoang Phuong VH. A randomized controlled study of pericapsular nerve group block (PENG block) plus lateral femoral cutaneous nerve block vs patient-controlled intravenous analgesia for postoperative analgesia after hip replacement surgery. Anaesth. pain intensive care 2024;28(2):324−328; DOI: 10.35975/apic.v28i2.2441
Received: December 22, 2023; Revised: January 26, 2024; Accepted: January 31, 2024
Hip joint degeneration tends to increase in all age groups.1 Early diagnosis and intervention play an important role in the prevention of complications and severe progression, after which hip replacement is the surgical procedure of choice. Postoperative pain after hip replacement surgery is moderate to severe, especially during the first 24 hours of the surgery, and has many sources of origin.2, 3 Postoperative patient recovery requires effective analgesia to ensure comfort and satisfaction, thereby supporting early mobilization and rehabilitation. Appropriate relief of post-operative pain accelerates recovery, shortens hospital stay, reduces surgical complications and minimizes post-operative mortality.4, 5
Various methods have been used to relieve pain after hip replacement such as systemic intravenous analgesia, continuous epidural analgesia, and peripheral nerve blocks. In particular, peripheral nerve block (PENG block) is known to be an effective pain reliever for hip surgery due to less motor and sympathetic inhibition, fewer opioid-related side effects, and reduced incidence of hypotension than other pain relief methods such as patient-controlled intravenous analgesia (PCA) and continuous epidural analgesia.5,6 However, the incision and the subcutaneous dissection of hip replacement surgery on the lateral surfaces of the upper thigh is innervated by the lateral femoral cutaneous nerve (LFCN). Evidence for the effectiveness of PENG Block in combination with LFCN block under ultrasound is still limited.
We conducted this study to compare the postoperative pain relief after hip replacement surgery by continuous PENG block in combination plus lateral femoral cutaneous nerve block under the guidance of ultrasound with patient-controlled intravenous analgesia.
2.1. Study settings and participants
We performed a randomized, controlled study on patients from 18 to 80 years old with American Society of Anesthesiologists (ASA) physical status I–III, who underwent hip replacement surgery at E University Hospital, Hanoi, Vietnam, from August 2021 to August 2022. Patients were excluded from the study if: patients had any contraindication to regional anesthesia, infection of the anesthetized area, coagulation disorders, organs dysfunction, allergy to anesthetics, did not cooperate with the physicians, history of opioid dependence, or inability to participate in the study.
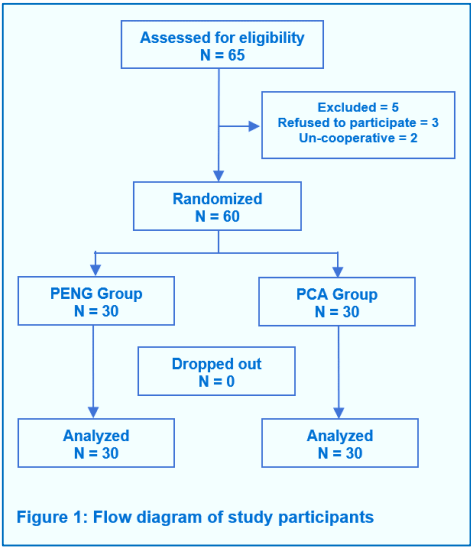
A total of 65 patients were assessed for eligibility. Five patients were excluded (2 patients refused to participate; 3 patients did not cooperate with the physicians). Therefore, a total of 60 patients were randomly divided into one of the two groups; PENG group receiving pain relief through PENG and LFCN block, and the PCA group receiving intravenous morphine as patient controlled analgesia (Figure 1).
2.2. Study procedure
First, patients were explained about the study and asked to sign written informed consent if they agreed to participate in the study. Next, the patient was instructed to use the visual analogue scale (VAS) for pain scoring, as well as how to press the button of the bell to request pain relief. Then the clinical parameters, e.g., electrocardiogram, blood pressure, SpO2, arterial blood pressure, and temperature, were monitored. The patient was oxygenated with 3-5 L/min O2 and a peripheral intravenous line established with an 18G catheter to infuse with 0.9% NaCl solution. Spinal anesthesia was administered with ropivacaine 0.5% and fentanyl.
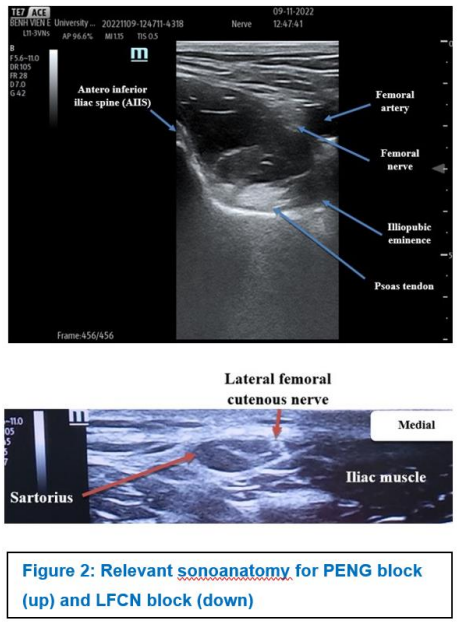
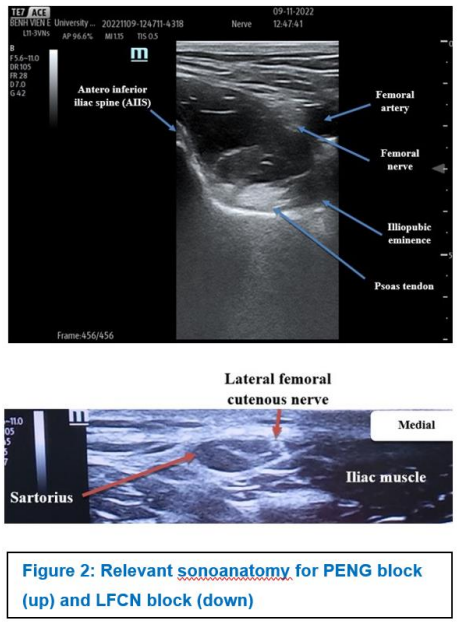
During and after the surgery, PCA group of patients received intravenous morphine (concentration 1 mg/ml, bolus dose of 1 mg, lock time 10 min, maximum dose 10 mg/4 h) via a PCA pump. The PENG group of patients received pain relief by PENG block and LFCN block. In this group, the ultrasound probe was placed horizontally from the anterior superior iliac spine, and was moved along the femoral arc defining the pubic spine. Then, the transducer was rotated 45 degrees, moved parallel to the femoral arch identifying the anterior inferior iliac spine (AIIS), iliopubic eminence (IPE) and inferior lumbosacral head. The ultrasound probe was moved lightly until the upper end of the femoral head was identified. Next, a 120 mm Tuohy 18G anesthetic needle was used under ultrasound guidance, which was moved lateral to medial in the plane between the ultrasound transducer and the superior tip of the femoral head. Then, 10 mL of ropivacaine 0.25% were injected through the needle tip (Figure 2).
2.3. Data collection
Data were collected; before surgery, before anesthesia, during surgery and after surgery. The information was recorded in the medical record.
2.3.1. Preoperative data: The collected information included the general characteristics of the study patients including age, gender, weight, height, history of smoking/motion sickness, diagnosis, physical status according to American Society of Anesthesiologists (ASA) classification, and liver and kidney function tests. With pre-anesthesia clinical data was collected including pulse, blood pressure, respiratory rate, and SpO2.
2.3.2. Intraoperative data: the information collected included information about anesthesia and surgical procedure.
2.3.3. Post-operative data: the collected information included blood test results (urea, creatinine, liver enzymes), pain scores (VAS - scale from 0 to 10, the higher the score, the higher the pain level), analgesic drugs consumption, respiratory and circulatory changes, adverse events, and patient satisfaction. Time was recorded from initiation of catheterization or PCA insertion (H0) to after 72 h (H72).
2.4. Statistical analysis
Data were entered and analyzed using SPSS 22.0 software. Descriptive statistics were applied. Statistical tests including t-test and chi-squared test were applied to compare the characteristics between PCA and PENG groups. Statistical significance was determined with the p < 0.05.
Table 1 shows that, there was no difference in age, gender, ASA PS classification, type of surgery, height, weight, time of surgery and dose of intrathecal ropivacaine in the two study groups.
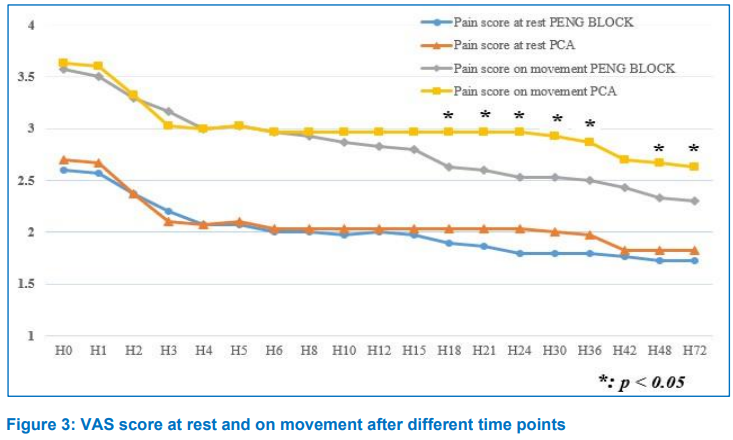
Figure 3 shows that, in the study times, the average VAS score at rest of both groups was at low pain level (VAS < 4). The average VAS score of the two groups at most of the time of the study did not have a statistically significant difference with P > 0.05. The VAS scores at rest at the time points H18, H21, H24, H30 in the PCA group were higher than in the PENG group. This difference was not statistically significant between the 2 study groups with P < 0.05. The VAS scores on movement at the time of H0, H1, H2, H3, H4, H5, H6, H8, H10, H12, H15, H42 of both study groups were not statistically significant between the 2 study groups with P > 0.05. The VAS score on movement at the time points H18, H21, H24, H30, H36, H48, H72 of the PCA group was higher than that of the PENG group. This difference was statistically significant between the 2 study groups with P < 0.05.
There were 22 patients (73.3%) in the PENG group, who did not need additional morphine after surgery.
Comparison of the average amount of morphine used in the 72 h after surgery was lower in the PENG group; 6.4 vs. 28.1mg with P < 0.001.
Table 2 shows that the frequency of vomiting/nausea of patients in the PCA group was significantly higher than in the PENG group (P = 0.006). No patient had had respiratory failure or urinary retention. There was statistically insignificant difference in the rate of itching in the two groups (P = 1).
The study results provide evidence of the effectiveness of PENG block method when compared with traditional PCA method in pain relief after hip replacement surgery.
When comparing the VAS pain score at rest and when flexing the thigh between the PENG group and the PCA group at the time of follow-up for 3 days after surgery, the study results showed that before local anesthetic injection in both groups, patients felt moderate pain at rest: VAS at rest at H0 (2.60 ± 0.563) in PENG group and (2.70 ± 0.466) in PCA group and this difference was not statistically significant (P > 0.05). After 3 hours (H3), the average resting VAS score in both groups decreased: in the PENG group it was 2.20 ± 0.484 and 2.10 ± 0.305 in PCA group. Our study also showed that the PENG group had lower VAS pain score at rest than the PCA group at all time-points after H0, but this difference was not statistically significant. This was similar to the study done by D-Yin Lin et al.,7 whose study showed that the PENG group experienced less pain than the femoral nerve block group. In that study, in the PENG group, 63% of the patients had no pain, 27% had mild pain, and 10% had moderate to severe pain. Meanwhile, 30% of the femoral nerve block group reported no pain, 27% mild pain and 36% moderate to severe pain; P = 0.04).7 Compared with other groups, the analgesic effect in the PENG group was better.
Assessing the pain scores on movement, the average VAS score was higher than the VAS score at rest at the same time. The VAS score on movement at H0 in PENG group (3.57 ± 0.728) and in PCA group (3.63 ± 0.556) was not different (P > 0.05). After 3 h of follow-up, the VAS score on movement in the PENG group was lower than that in the PCA group, but the difference was not significant. From H18 onwards, the VAS score on movement in the PENG group was lower than that of the PCA group and the difference between the two groups was statistically significant (P < 0.05). The results of our study showed that PENG block method combined with LFCN in patients after hip replacement surgery had good analgesic effect, reduces VAS pain score for patients after hip replacement surgery with comparable pain relief most of the time at rest. Regarding the difference in VAS scores between the two groups, especially when on movement, we believed that in the PENG group, the nerve block is incomplete and we do not know for sure the spread of the drug in the muscle fascia.
In our study, the PCA group had 8 patients (26.7%) with nausea/vomiting, 1 patient (3.3%) had itching, no patient had respiratory failure and urinary retention. Meanwhile, in the PENG group, there were no patients with any side effects such as nausea/vomiting, respiratory depression, urinary retention and itching. Adverse effects such as nausea or vomiting in the PCA group had a significantly higher rate than in the PENG group (P < 0.05). This result is similar to the result of Singelyn FJ et al.6 The rate of patients with nausea might vary from 22-30% due to undesirable effects of morphine drugs that stimulate receptors in the vomiting center of the brain. Most patients had mild nausea and itching that did not require treatment. This was also a major disadvantage of intravenous PCA analgesia compared with regional anesthesia when choosing to relieve pain after hip surgery, because the selective nerve block method allows the correct position of the surgical site to be blocked, reducing these undesirable effects.8
In our study, the number of patients with complications during anesthesia and pain relief was three. In the PENG group, there were 3 patients with mild pain at the local insertion site. In these cases, we proceeded to adjust the anesthetic needle, or re-inject the needle, checked the aspiration and conducted catheterization and pain relief after surgery normally. Currently, with the application of ultrasound techniques to regional anesthesia and analgesia, anesthesiologists can clearly see the images of nerves, arteries, and veins, which helps to minimize complications related to nerve and vascular puncture. Regional block even under ultrasound guidance could still have potential risks such as vascular puncture, nerve damage, infection, and local injection allergy.9, 10
Our study did not record any complications such as swelling in the needle puncture area, infection or local anesthetic drug poisoning. The complications encountered were all mild, did not require any further intervention and did not affect the results of postoperative pain relief.
This study has some limitations with its small sample size and was conducted in only one hospital. Further studies with largeer sample sizes and multicenter implementation are needed. In addition, studies to understand the factors related to the analgesic effect of PENG block method also need to be done in the future.
In conclusion, study results show that pericapsular nerve group block in combination with lateral femoral cutaneous nerve block offers good postoperative pain relief results when compared with traditional PCA method after hip replacement.
7. Data availability
The datasets supporting the finding of this study are available from the corresponding author upon reasonable request.
8. Acknowledgements
The authors would like to express their sincere thanks to the medical staff working at the Department of Anesthesiology and Resuscitation, E Hospital, Hanoi in conducting this study.
9. Conflict of interest
No potential conflict of interest relevant to this article is reported. No funding to declare.
10. Ethical approval
The protocol of this study was approved by the Hanoi Medical University Institutional Ethical Review Board number CKII34/IRB-VN01.001/IRB00003121/FWA00004148 and registered in the Clinical Trial (registration number: NCT06040879). Patients were informed and asked to give written informed consent before participating in the study.
11. Authors’ contribution
TVD, VHP: conduct study, literature search, statistical analysis and manuscript write
NDH, NXQ: literature search, statistical analysis and manuscript write
THN, DVT: statistical analysis and manuscript write
Author affiliations:
- TRAN Van Dang, Can Tho University of Medicine and Pharmacy, Can Tho, Vietnam; E-mail: tvdang@ctump.edu.vn
- NGUYEN Do Hung, E University Hospital, Hanoi, Vietnam; E-mail: dohung@trungtamtimmach.vn
- NGUYEN Xuan Quang, E University Hospital, Hanoi, Vietnam; E-mail: drquangvx@gmail.com
- Tu Huu Nguyen, Hanoi Medical University, Hanoi Medical University Hospital, Hanoi, Vietnam; E-mail: nguyenhuutu@hmu.edu.vn
- Duc Viet Tran, Hanoi Medical University Hospital, Hanoi, Vietnam; E-mail: ductran.hmu@gmail.com
- VU Hoang Phuong, Hanoi Medical University, Hanoi Medical University Hospital, Hanoi, Vietnam; E-mail: vuhoangphuong@hmu.edu.vn
ABSTRACT
Background: Postoperative pain often remains troublesome for the patients, if not adequately managed. Various modalities have been tried to keep the patient pain free. Regional nerve blocks under ultrasound guidance have recently gained much popularity. We aimed to compare the pain relief outcomes after hip replacement surgery by continuous Pericapsular Nerve Group Block (PENG Block) in combination with lateral femoral cutaneous nerve (LFCN) block under the guidance of ultrasound versus patient-controlled intravenous analgesia (PCA).
Methodology: Sixty patients, who underwent hip surgery at E University Hospital, Hanoi, Vietnam, from August 2021 to August 2022, were randomly allocated to one of the two groups: group of patients with pain relief with PENG block in combination with LFCN block (PENG group) and the group of patients with patient-controlled intravenous analgesia (PCA group). Outcomes regarding clinical parameters and pain scores on Visual Analogue Scale (VAS), from the initiation of the blocks or the PCA (H0) to 72 h (H72) were recorded and compared.
Results: Sixty patients were included in this study. The average VAS scores at rest in both groups was at low pain level (VAS < 4). The average VAS score in both of the groups at most of the time of the study did not have a statistically significant difference. The VAS on movement at the time points H18, H21, H24, H30, H36, H48, H72 of the PENG group was lower than that of the PCA group and the difference was statistically significant between the two groups (P < 0.05). The rate of vomiting/nausea of patients in the PCA group was significantly higher than in the PENG group (P = 0.006).
Conclusion: Pericapsular nerve block combined with lateral femoral cutaneous nerve block offers prolonged pain relief when compared with traditional patient-controlled intravenous analgesia in postoperative pain relief after hip replacement, and is associated with lower frequency of vomiting/nausea.
Abbreviations: ASA - American Society of Anesthesiologists; AIIS - Anterior Inferior Iliac Spine; IPE - Iliopubic Eminence; LFCN - Lateral Femoral Cutaneous Nerve; PCA - Patient-Controlled Analgesia; PENG - Pericapsular Nerve Group; VAS - Visual Analogue Scale.
Keywords: Pericapsular nerve group block; Lateral femoral cutaneous nerve; Hip replacement; Multimodal analgesia; Ultrasound-guided analgesia; Patient-controlled analgesia; Side effects.
Citation: Dang TV, Hung ND, Quangm NX, Nguyen TH, Tran DV, VU Hoang Phuong VH. A randomized controlled study of pericapsular nerve group block (PENG block) plus lateral femoral cutaneous nerve block vs patient-controlled intravenous analgesia for postoperative analgesia after hip replacement surgery. Anaesth. pain intensive care 2024;28(2):324−328; DOI: 10.35975/apic.v28i2.2441
Received: December 22, 2023; Revised: January 26, 2024; Accepted: January 31, 2024
1. INTRODUCTION
Hip joint degeneration tends to increase in all age groups.1 Early diagnosis and intervention play an important role in the prevention of complications and severe progression, after which hip replacement is the surgical procedure of choice. Postoperative pain after hip replacement surgery is moderate to severe, especially during the first 24 hours of the surgery, and has many sources of origin.2, 3 Postoperative patient recovery requires effective analgesia to ensure comfort and satisfaction, thereby supporting early mobilization and rehabilitation. Appropriate relief of post-operative pain accelerates recovery, shortens hospital stay, reduces surgical complications and minimizes post-operative mortality.4, 5
Various methods have been used to relieve pain after hip replacement such as systemic intravenous analgesia, continuous epidural analgesia, and peripheral nerve blocks. In particular, peripheral nerve block (PENG block) is known to be an effective pain reliever for hip surgery due to less motor and sympathetic inhibition, fewer opioid-related side effects, and reduced incidence of hypotension than other pain relief methods such as patient-controlled intravenous analgesia (PCA) and continuous epidural analgesia.5,6 However, the incision and the subcutaneous dissection of hip replacement surgery on the lateral surfaces of the upper thigh is innervated by the lateral femoral cutaneous nerve (LFCN). Evidence for the effectiveness of PENG Block in combination with LFCN block under ultrasound is still limited.
We conducted this study to compare the postoperative pain relief after hip replacement surgery by continuous PENG block in combination plus lateral femoral cutaneous nerve block under the guidance of ultrasound with patient-controlled intravenous analgesia.
2. METHODOLOGY
2.1. Study settings and participants
We performed a randomized, controlled study on patients from 18 to 80 years old with American Society of Anesthesiologists (ASA) physical status I–III, who underwent hip replacement surgery at E University Hospital, Hanoi, Vietnam, from August 2021 to August 2022. Patients were excluded from the study if: patients had any contraindication to regional anesthesia, infection of the anesthetized area, coagulation disorders, organs dysfunction, allergy to anesthetics, did not cooperate with the physicians, history of opioid dependence, or inability to participate in the study.
A total of 65 patients were assessed for eligibility. Five patients were excluded (2 patients refused to participate; 3 patients did not cooperate with the physicians). Therefore, a total of 60 patients were randomly divided into one of the two groups; PENG group receiving pain relief through PENG and LFCN block, and the PCA group receiving intravenous morphine as patient controlled analgesia (Figure 1).
2.2. Study procedure
First, patients were explained about the study and asked to sign written informed consent if they agreed to participate in the study. Next, the patient was instructed to use the visual analogue scale (VAS) for pain scoring, as well as how to press the button of the bell to request pain relief. Then the clinical parameters, e.g., electrocardiogram, blood pressure, SpO2, arterial blood pressure, and temperature, were monitored. The patient was oxygenated with 3-5 L/min O2 and a peripheral intravenous line established with an 18G catheter to infuse with 0.9% NaCl solution. Spinal anesthesia was administered with ropivacaine 0.5% and fentanyl.
During and after the surgery, PCA group of patients received intravenous morphine (concentration 1 mg/ml, bolus dose of 1 mg, lock time 10 min, maximum dose 10 mg/4 h) via a PCA pump. The PENG group of patients received pain relief by PENG block and LFCN block. In this group, the ultrasound probe was placed horizontally from the anterior superior iliac spine, and was moved along the femoral arc defining the pubic spine. Then, the transducer was rotated 45 degrees, moved parallel to the femoral arch identifying the anterior inferior iliac spine (AIIS), iliopubic eminence (IPE) and inferior lumbosacral head. The ultrasound probe was moved lightly until the upper end of the femoral head was identified. Next, a 120 mm Tuohy 18G anesthetic needle was used under ultrasound guidance, which was moved lateral to medial in the plane between the ultrasound transducer and the superior tip of the femoral head. Then, 10 mL of ropivacaine 0.25% were injected through the needle tip (Figure 2).
2.3. Data collection
Data were collected; before surgery, before anesthesia, during surgery and after surgery. The information was recorded in the medical record.
2.3.1. Preoperative data: The collected information included the general characteristics of the study patients including age, gender, weight, height, history of smoking/motion sickness, diagnosis, physical status according to American Society of Anesthesiologists (ASA) classification, and liver and kidney function tests. With pre-anesthesia clinical data was collected including pulse, blood pressure, respiratory rate, and SpO2.
2.3.2. Intraoperative data: the information collected included information about anesthesia and surgical procedure.
2.3.3. Post-operative data: the collected information included blood test results (urea, creatinine, liver enzymes), pain scores (VAS - scale from 0 to 10, the higher the score, the higher the pain level), analgesic drugs consumption, respiratory and circulatory changes, adverse events, and patient satisfaction. Time was recorded from initiation of catheterization or PCA insertion (H0) to after 72 h (H72).
2.4. Statistical analysis
Data were entered and analyzed using SPSS 22.0 software. Descriptive statistics were applied. Statistical tests including t-test and chi-squared test were applied to compare the characteristics between PCA and PENG groups. Statistical significance was determined with the p < 0.05.
3. RESULTS
Table 1 shows that, there was no difference in age, gender, ASA PS classification, type of surgery, height, weight, time of surgery and dose of intrathecal ropivacaine in the two study groups.
| Table 1: Demographic and clinical characteristics | |||
| PENG Group
(n=30) |
PCA Group
(n=30) |
p-value | |
| ASA classification | |||
| I | 3 (10.0%) | 4 (13.3%) | 1.000 |
| II | 27 (90.0%) | 26 (86.7%) | |
| Gender | |||
| Male | 17 (56.7%) | 14 (46.7%) | 0.606 |
| Female | 13 (43.3%) | 16 (53.3%) | |
| Type of surgery | |||
| Total hip replacement | 17 (56.7%) | 21 (70.0) | 0.422 |
| Partial hip replacement | 13 (43.3%) | 9 (30.0) | |
| Age (years) | 60.6 ± 12.8 | 66.0 ± 11.7 | 0.090 |
| Height (m) | 1.62 ± 0.0861 | 1.60 ± 0.0924 | 0.494 |
| Weight (kg) | 54.2 ± 8.28 | 53.5 ± 9.79 | 0.772 |
| Surgery time (min) | 57.0 ± 19.9 | 61.8 ± 23.1 | 0.390 |
| Dose of ropivacaine (mg) | 10.6 ± 1.33 | 10.2 ± 1.13 | 0.214 |
| Data presented as n (%) or mean ± SD; P < 0.05 considered as significant. | |||
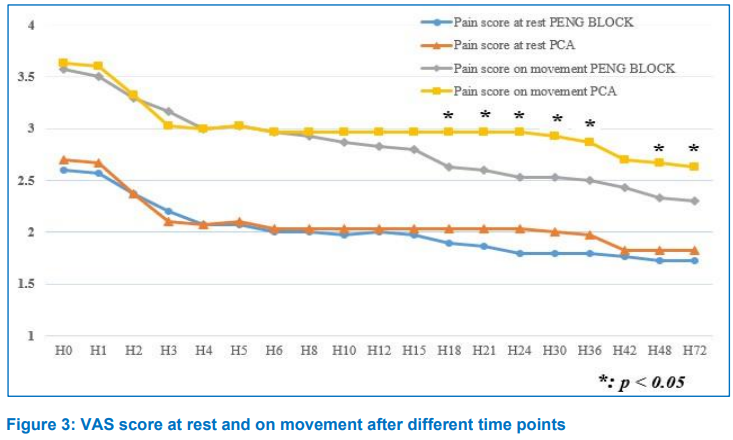
Figure 3 shows that, in the study times, the average VAS score at rest of both groups was at low pain level (VAS < 4). The average VAS score of the two groups at most of the time of the study did not have a statistically significant difference with P > 0.05. The VAS scores at rest at the time points H18, H21, H24, H30 in the PCA group were higher than in the PENG group. This difference was not statistically significant between the 2 study groups with P < 0.05. The VAS scores on movement at the time of H0, H1, H2, H3, H4, H5, H6, H8, H10, H12, H15, H42 of both study groups were not statistically significant between the 2 study groups with P > 0.05. The VAS score on movement at the time points H18, H21, H24, H30, H36, H48, H72 of the PCA group was higher than that of the PENG group. This difference was statistically significant between the 2 study groups with P < 0.05.
There were 22 patients (73.3%) in the PENG group, who did not need additional morphine after surgery.
| Table 2: Side effects comparing between two groups | |||
| PENG Group (n = 30) |
PCA Group (n = 30) |
P-value | |
| Itchy | 0 (0%) | 1 (3.3%) | 1 |
| Vomiting/ Nausea | 0 (0%) | 8 (26.7%) | 0.006 |
| Respiratory failure | 0 (0%) | 0 (0%) | 1 |
| Urinary retention | 0 (0%) | 0 (0%) | 1 |
| P < 0.05 considered as significant. | |||
Comparison of the average amount of morphine used in the 72 h after surgery was lower in the PENG group; 6.4 vs. 28.1mg with P < 0.001.
Table 2 shows that the frequency of vomiting/nausea of patients in the PCA group was significantly higher than in the PENG group (P = 0.006). No patient had had respiratory failure or urinary retention. There was statistically insignificant difference in the rate of itching in the two groups (P = 1).
4. DISCUSSION
The study results provide evidence of the effectiveness of PENG block method when compared with traditional PCA method in pain relief after hip replacement surgery.
When comparing the VAS pain score at rest and when flexing the thigh between the PENG group and the PCA group at the time of follow-up for 3 days after surgery, the study results showed that before local anesthetic injection in both groups, patients felt moderate pain at rest: VAS at rest at H0 (2.60 ± 0.563) in PENG group and (2.70 ± 0.466) in PCA group and this difference was not statistically significant (P > 0.05). After 3 hours (H3), the average resting VAS score in both groups decreased: in the PENG group it was 2.20 ± 0.484 and 2.10 ± 0.305 in PCA group. Our study also showed that the PENG group had lower VAS pain score at rest than the PCA group at all time-points after H0, but this difference was not statistically significant. This was similar to the study done by D-Yin Lin et al.,7 whose study showed that the PENG group experienced less pain than the femoral nerve block group. In that study, in the PENG group, 63% of the patients had no pain, 27% had mild pain, and 10% had moderate to severe pain. Meanwhile, 30% of the femoral nerve block group reported no pain, 27% mild pain and 36% moderate to severe pain; P = 0.04).7 Compared with other groups, the analgesic effect in the PENG group was better.
Assessing the pain scores on movement, the average VAS score was higher than the VAS score at rest at the same time. The VAS score on movement at H0 in PENG group (3.57 ± 0.728) and in PCA group (3.63 ± 0.556) was not different (P > 0.05). After 3 h of follow-up, the VAS score on movement in the PENG group was lower than that in the PCA group, but the difference was not significant. From H18 onwards, the VAS score on movement in the PENG group was lower than that of the PCA group and the difference between the two groups was statistically significant (P < 0.05). The results of our study showed that PENG block method combined with LFCN in patients after hip replacement surgery had good analgesic effect, reduces VAS pain score for patients after hip replacement surgery with comparable pain relief most of the time at rest. Regarding the difference in VAS scores between the two groups, especially when on movement, we believed that in the PENG group, the nerve block is incomplete and we do not know for sure the spread of the drug in the muscle fascia.
In our study, the PCA group had 8 patients (26.7%) with nausea/vomiting, 1 patient (3.3%) had itching, no patient had respiratory failure and urinary retention. Meanwhile, in the PENG group, there were no patients with any side effects such as nausea/vomiting, respiratory depression, urinary retention and itching. Adverse effects such as nausea or vomiting in the PCA group had a significantly higher rate than in the PENG group (P < 0.05). This result is similar to the result of Singelyn FJ et al.6 The rate of patients with nausea might vary from 22-30% due to undesirable effects of morphine drugs that stimulate receptors in the vomiting center of the brain. Most patients had mild nausea and itching that did not require treatment. This was also a major disadvantage of intravenous PCA analgesia compared with regional anesthesia when choosing to relieve pain after hip surgery, because the selective nerve block method allows the correct position of the surgical site to be blocked, reducing these undesirable effects.8
In our study, the number of patients with complications during anesthesia and pain relief was three. In the PENG group, there were 3 patients with mild pain at the local insertion site. In these cases, we proceeded to adjust the anesthetic needle, or re-inject the needle, checked the aspiration and conducted catheterization and pain relief after surgery normally. Currently, with the application of ultrasound techniques to regional anesthesia and analgesia, anesthesiologists can clearly see the images of nerves, arteries, and veins, which helps to minimize complications related to nerve and vascular puncture. Regional block even under ultrasound guidance could still have potential risks such as vascular puncture, nerve damage, infection, and local injection allergy.9, 10
Our study did not record any complications such as swelling in the needle puncture area, infection or local anesthetic drug poisoning. The complications encountered were all mild, did not require any further intervention and did not affect the results of postoperative pain relief.
5. LIMITATIONS
This study has some limitations with its small sample size and was conducted in only one hospital. Further studies with largeer sample sizes and multicenter implementation are needed. In addition, studies to understand the factors related to the analgesic effect of PENG block method also need to be done in the future.
6. CONCLUSION
In conclusion, study results show that pericapsular nerve group block in combination with lateral femoral cutaneous nerve block offers good postoperative pain relief results when compared with traditional PCA method after hip replacement.
7. Data availability
The datasets supporting the finding of this study are available from the corresponding author upon reasonable request.
8. Acknowledgements
The authors would like to express their sincere thanks to the medical staff working at the Department of Anesthesiology and Resuscitation, E Hospital, Hanoi in conducting this study.
9. Conflict of interest
No potential conflict of interest relevant to this article is reported. No funding to declare.
10. Ethical approval
The protocol of this study was approved by the Hanoi Medical University Institutional Ethical Review Board number CKII34/IRB-VN01.001/IRB00003121/FWA00004148 and registered in the Clinical Trial (registration number: NCT06040879). Patients were informed and asked to give written informed consent before participating in the study.
11. Authors’ contribution
TVD, VHP: conduct study, literature search, statistical analysis and manuscript write
NDH, NXQ: literature search, statistical analysis and manuscript write
THN, DVT: statistical analysis and manuscript write
12. REFERENCES
- World Health Organization. Musculoskeletal health 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions.
- Ferguson RJ, Palmer AJ, Taylor A, Porter ML, Malchau H, Glyn-Jones S. Hip replacement. Lancet. 2018;392:1662-71. PMID: 30496081 DOI: 1016/S0140-6736(18)31777-X
- Ferrata P, Carta S, Fortina M, Scipio D, Riva A, Di Giacinto S. Painful hip arthroplasty: definition. Clin Cases Miner Bone Metab. 2011;8(2):19-22. PMID: 22461810
- YaDeau JT, Tedore T, Goytizolo EA, Kim DH, Green DS, Westrick A, et al. Lumbar plexus blockade reduces pain after hip arthroscopy: a prospective randomized controlled trial. Anesth Analg. 2012;115(4):968-72. D PMID: 22822195 OI: 1213/ANE.0b013e318265bacd
- Duarte LT, Beraldo PS, Saraiva RA. Effects of epidural analgesia and continuous lumbar plexus block on functional rehabilitation after total hip arthroplasty. Rev Bras Anestesiol. 2009;59(5):531-44. PMID: 19784509 DOI: 1016/s0034-7094(09)70078-9
- Singelyn FJ, Ferrant T, Malisse MF, Joris D. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous femoral nerve sheath block on rehabilitation after unilateral total-hip arthroplasty. Reg Anesth Pain Med. 2005;30(5):452-7. PMID: 16135349 DOI: 1016/j.rapm.2005.05.008
- Lin DY, Morrison C, Brown B, Saies AA, Pawar R, Vermeulen M, et al. Pericapsular nerve group (PENG) block provides improved short-term analgesia compared with the femoral nerve block in hip fracture surgery: a single-center double-blinded randomized comparative trial. Reg Anesth Pain Med. 2021;46(5):398-403. PMID: 33637625 DOI: 1136/rapm-2020-102315
- Shafiq F, Hamid M, Samad K. Complications and interventions associated with epidural analgesia for postoperative pain relief in a tertiary care hospital. Middle East J Anaesthesiol. 2010;20(6):827-32. PMID: 21526668
- Rasouli MR, Viscusi ER. Adductor Canal Block for Knee Surgeries: An Emerging Analgesic Technique. Arch Bone Jt Surg. 2017;5(3):131-2. PMID: 28656158
- Kamel I, Ahmed MF, Sethi A. Regional anesthesia for orthopedic procedures: What orthopedic surgeons need to know. World J Orthop. 2022;13(1):11-35. PMID: 35096534 DOI: 5312/wjo.v13.i1.11