Yashpal Singh 1 , Adarsh Kumar Yadav 1 , Vijeta Bajpai 2 , Priyanka Diwedi 2 ,
Shekhar Verma 1 , Ravi Kumar Verma 1
Author affiliations:
Abstract
Background & Objective: Hyperbaric bupivacaine is the most commonly used local anesthetic for spinal anesthesia, alone or in combination with various adjuvants. Opioids are frequently used for their rapid onset and intense block characteristics. Fentanyl is the preferred intrathecal opioids with rapid onset of action but has a shorter duration of action. Buprenorphine is a mixed agonist-antagonist with high affinity at both mu and kappa opioid receptors. We compared administration of buprenorphine with fentanyl as adjuvants with intrathecal hyperbaric bupivacaine in gynecological surgeries.
Methodology: After Institutional Ethical Committee approval and written informed consent, 60 patients aged 18–65 y, scheduled for lower abdominal gynecological surgery, were divided into two equal groups; Group F to receive 0.5% hyperbaric bupivacaine 2.5 ml with fentanyl 25 µg intrathecal and Group B to receive 0.5% hyperbaric bupivacaine 2.5 ml with buprenorphine 75 µg intrathecal. Block characteristics and associated side effects were compared between two groups. The data was analyzed using Chi square test and Fisher’s exact test. For comparing two group of mean, independent student’s t test was used. P-value < 0.05 was considered as statistically significant.
Results: The mean onset of sensory and motor block was significantly earlier in Group F than Group B (p < 0.001). Mean duration of sensory block was significantly prolonged in Group B compared to Group F (p < 0.05). Whereas, the duration of motor was comparable in both of the groups (p > 0.05). Duration of analgesia was significantly prolonged in Group B than Group F (p < 0.001).
Conclusion: We conclude that when a longer duration of postoperative pain relief is needed, buprenorphine can be a suitable drug to be used with intrathecal hyperbaric bupivacaine for gynecological surgeries because of prolonged duration of action.
Key words: Spinal anesthesia; Fentanyl; Buprenorphine; Bupivacaine
Citation: Singh Y, Yadav AK, Vijeta Bajpai, Diwedi P, Verma S, Verma RK. Comparison of intrathecal fentanyl and buprenorphine as adjuvants to bupivacaine in gynecological surgery. Anaesth. pain intensive care 2021;26(1):39-43. DOI: 10.35975/apic.v26i1.1764
Introduction
Spinal anesthesia is the most commonly used anesthetic technique in lower abdominal and lower limb surgeries.1 Various local anesthetic drugs are used at different doses and in different baricities with or without addition of an adjuvant.2,3 Hyperbaric bupivacaine is the most commonly used local anesthetic drug since long time with rapid onset and reliable block characteristics.4,5
Different adjuvants are added to local anesthetics for improving the quality of block and to increase the duration of analgesia, without causing significant adverse effects.6,7 The collective use of local anesthetic adjuvants has evolved over the period from classical opioids to a wide array of drugs spanning several groups and varying mechanisms of action.8
Intrathecal opioids act synergistically with local anesthetic drugs, these drugs intensify the sensory block without increasing the sympathetic block while achieving a satisfactory quality of spinal anesthesia at a much lower dose of local anesthetics drugs. Fentanyl is a potent, commonly used centrally acting opioid that is usually combined with the local anesthetic agent for perioperative anesthesia and analgesia.9,10 Fentanyl binds to opioid receptors, mainly the mu opioid receptor. Buprenorphine is an adjuvant used in spinal anesthesia, it is a mixed agonist-antagonist with high affinity at both mu and kappa opioid receptors.11 It is a weak kappa-opioid receptor antagonist and weak partial mu-opioid receptor agonist. Buprenorphine is readily available as compared to fentanyl, especially in peripheral cities.
We compared the effects of intrathecal administration of fentanyl and buprenorphine with hyperbaric bupivacaine, on block characteristics in elective gynecological surgeries.
Methodology
After Institutional Ethical Committee approval and written informed consent, 63 patients aged 18–65 y, American Society of Anesthesiologist (ASA) grade I or II, scheduled for lower abdominal gynecological surgery were included in this prospective, randomized trial. Patients with a history of hypertension, diabetes mellitus, morbid obesity, hypersensitivity to studied drugs and emergency surgery were excluded from study.
All patients were randomly assigned to one of the two equal groups; Group F to receive 0.5% hyperbaric bupivacaine 2.5 ml with fentanyl 25 µg; and Group B to receive 0.5% hyperbaric bupivacaine 2.5 ml with buprenorphine 75 µg. Total volume of the drugs administered intrathecally was 3 ml in both of the groups. Randomization was performed by an anesthesiologist involved in studied drug preparation, who did not participate in drug administration. Further procedure and monitoring were performed by another investigator unaware of the group allocation; patients were also blinded to the drug regimen utilized for spinal anesthesia in them.
All the patient were premedicated with tablet alprazolam (0.25 mg) and tablet ranitidine (150 mg) orally evening before surgery, and 2 h before the scheduled procedure. In operating room, standard monitors were placed and baseline parameters recorded. An 18-gauge intravenous (IV) catheter was placed at the dorsum of the hand and lactated ringer solution started. Patients were explained about the procedure and methodology of monitoring. A midline lumbar puncture was performed at L3‑L4 intervertebral space by 25-gauge Quincke spinal needle (BD, Gurgaon, Haryana, India) in the lateral decubitus position, under aseptic precautions. After confirmation of the free flow of cerebrospinal fluid through the spinal needle, the studied drug solution was injected over a period of 10–15 sec and the patients were turned supine.
Duration of sensory-motor block was measured from the point of commencement of spinal anesthesia. The upper level of sensory block was assessed bilaterally by pinprick method. Modified Bromage scale was used to assess motor block; 0 = Patient able to move hip, knee, ankle, 1 = Unable to move hip, able to move knee and
ankle, 2 = Unable to move hip and knee, able to move ankle, 3 = Unable to move hip, knee and ankle. Assessment of block was performed every 2 min after the spinal anesthesia till the T6 dermatomal level and Bromage score of 3 was achieved. After that it was performed at every 20 min, until the recovery of S2 dermatome (duration of the sensory block) and Bromage score of “0” (duration of the motor block) was achieved. Hemodynamic variables were monitored continuously and any incidence of associated side-effects was documented till sensory-motor levels regressed to above-mentioned threshold during the postoperative period.
Statistical analysis: Sample size was calculated by the following formula;
For two mean n = 2S2(Z1-α/2+Z1-β)2 /2. Where, S = pooled standard deviation, n = required number of samples for each group, 1-β = power, 1-α = level of confidence, d = mean difference, S = combined standard deviation, α = 5% level of significance at two tailed test, 80% is the power of the study with one-to-one ratio. Sample size required for each group was calculated to be 30 (n = 30).
Statistical analysis was performed using statistical package for the social sciences (SPSS), Version 23.0. IBM Corp., NY). Simple descriptive statistics were used, e.g., mean ± SD for quantitative variables, and frequency with percentage for categorized variables. The data was analyzed using Chi square test and Fisher’s exact test. For comparing two groups of means independent student’s t test was used. P-value < 0.05 was considered as statistically significant.
Results
Out of 63 patients, 60 patient completed study and 3 were excluded (Figure 1). The study groups were comparable in terms of demographic profile, baseline hemodynamic variables and ASA status (Table 1).
The mean onset of sensory block (onset time of T10 level sensory block) was significantly earlier in Group F (2.96 ± 0.35 min) than Group B (3.47 ± 60.35 min) (p < 0.001) (Table 2). Whereas, the mean duration of sensory block was significantly prolonged in Group B (270.10 ± 42.22 min) compared to Group F (234.13 ± 34.58 min) (p value < 0.05) (Table 2).
The mean time for onset of motor block was significantly earlier in Group F (3.85 ± 00.38 min) when compared with Group B (4.12 ± 0.36 min) (p < 0.001) (Table 2). Whereas, the duration of motor block (Modified Bromage score to become 0) was comparable in both the groups (P > 0.05) (Table 2).
Duration of analgesia (time to first analgesia requirement after the study drugs were injected intra-thecally) was significantly prolonged in Group B (516.50 ± 47.25 min) than Group F (371.20 ± 60.03 min) (P < 0.001).
Regarding side effects of study medications, nausea was found in both the groups, but the incidence was higher in Group B (50%) as compared to Group F (20%). Similarly, the incidence of vomiting and shivering was higher in Group B (53.3% and 40% respectively) than in Group F (13.3% and 6.7% respectively) (Table 3).
Discussion
For this study, we selected two opioids belonging to two different groups. Both are lipophilic drugs, but while fentanyl is a pure agonist, buprenorphine is a partial agonist. In our study, the onset of sensory and motor block was earlier in fentanyl group than buprenorphine group. This finding was supported by the study of Khan et al.12 in which sensory and motor blockade was achieved faster in fentanyl group than buprenorphine. The mean duration of sensory block was significantly longer in Group B (p = 0.001) than Group F in our study. The longer duration of buprenorphine is because of its higher affinity towards opioid receptor and high lipid solubility.10 Mean duration of motor block was comparable between two groups (p = 0.265). The finding was consistent with the study by Khan et al.12
Buprenorphine has a prolonged duration of action due to its complex receptor kinetics. It has a very high affinity to opiate receptors. It forms an avid complex with the receptor, tends to persist for long duration of period. The opiate receptor affinity for buprenorphine is 50 times more than that of morphine.13,14 The high lipid solubility and high affinity for opiate receptors of buprenorphine explains buprenorphine’s prolonged duration of action when compared to other lipid soluble drugs like fentanyl which produces short lived analgesia due to its rapid clearance from spinal cord sites.15
Nausea and vomiting are due to rostral spread of opioid in CSF to intrathecal structures including vomiting center and chemoreceptor trigger zone in the vascularized area postrema in the floor of fourth ventricle. In our study, the incidence of nausea, vomiting and shivering was higher in the buprenorphine group than the fentanyl group.
None of the patients in our study exhibited any untoward serious cardiovascular, respiratory or CNS effects, which further proved that buprenorphine is a safe and suitable agent for postoperative pain relief by intrathecal route. When a longer duration of postoperative pain relief is needed, buprenorphine can be a suitable drug for gynecological patients because of prolonged duration of action.
Conclusion
Although buprenorphine had a relatively higher incidence of side effects, especially nausea and vomiting, most of the patients tolerated these side effects well. Therefore, it can be a good alternative option as an adjuvant to spinal anesthesia in patients undergoing abdominal gynecological surgeries, especially to prolong the duration of the postoperative analgesia.
Limitations
The present study had certain limitations. It was conducted with a small sample size. Therefore, we feel that a few randomized double-blind control trials with a larger sample size of patients may be conducted to further confirm its usefulness.
Conflict of interest
None declared by the authors.
Authors’ contribution
YS, AKY: Concept and design, Literature search, conduct of study, manuscript preparation, data analysis, manuscript editing, and manuscript review.
VB, PD, RKV: Concept and design, Literature search, data analysis, critical manuscript editing, manuscript review.
SV: Concept and design, Literature search, conduct of study, data analysis, manuscript editing,
References
Shekhar Verma 1 , Ravi Kumar Verma 1
Author affiliations:
- Department of Anesthesiology, Institute of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh 221005, India.
- Dept. of Anesthesiology, All India Institute of Medical Sciences, Kunraghat, Gorakhpur, Uttar Pradesh 273008, India.
Abstract
Background & Objective: Hyperbaric bupivacaine is the most commonly used local anesthetic for spinal anesthesia, alone or in combination with various adjuvants. Opioids are frequently used for their rapid onset and intense block characteristics. Fentanyl is the preferred intrathecal opioids with rapid onset of action but has a shorter duration of action. Buprenorphine is a mixed agonist-antagonist with high affinity at both mu and kappa opioid receptors. We compared administration of buprenorphine with fentanyl as adjuvants with intrathecal hyperbaric bupivacaine in gynecological surgeries.
Methodology: After Institutional Ethical Committee approval and written informed consent, 60 patients aged 18–65 y, scheduled for lower abdominal gynecological surgery, were divided into two equal groups; Group F to receive 0.5% hyperbaric bupivacaine 2.5 ml with fentanyl 25 µg intrathecal and Group B to receive 0.5% hyperbaric bupivacaine 2.5 ml with buprenorphine 75 µg intrathecal. Block characteristics and associated side effects were compared between two groups. The data was analyzed using Chi square test and Fisher’s exact test. For comparing two group of mean, independent student’s t test was used. P-value < 0.05 was considered as statistically significant.
Results: The mean onset of sensory and motor block was significantly earlier in Group F than Group B (p < 0.001). Mean duration of sensory block was significantly prolonged in Group B compared to Group F (p < 0.05). Whereas, the duration of motor was comparable in both of the groups (p > 0.05). Duration of analgesia was significantly prolonged in Group B than Group F (p < 0.001).
Conclusion: We conclude that when a longer duration of postoperative pain relief is needed, buprenorphine can be a suitable drug to be used with intrathecal hyperbaric bupivacaine for gynecological surgeries because of prolonged duration of action.
Key words: Spinal anesthesia; Fentanyl; Buprenorphine; Bupivacaine
Citation: Singh Y, Yadav AK, Vijeta Bajpai, Diwedi P, Verma S, Verma RK. Comparison of intrathecal fentanyl and buprenorphine as adjuvants to bupivacaine in gynecological surgery. Anaesth. pain intensive care 2021;26(1):39-43. DOI: 10.35975/apic.v26i1.1764
Introduction
Spinal anesthesia is the most commonly used anesthetic technique in lower abdominal and lower limb surgeries.1 Various local anesthetic drugs are used at different doses and in different baricities with or without addition of an adjuvant.2,3 Hyperbaric bupivacaine is the most commonly used local anesthetic drug since long time with rapid onset and reliable block characteristics.4,5
Different adjuvants are added to local anesthetics for improving the quality of block and to increase the duration of analgesia, without causing significant adverse effects.6,7 The collective use of local anesthetic adjuvants has evolved over the period from classical opioids to a wide array of drugs spanning several groups and varying mechanisms of action.8
Intrathecal opioids act synergistically with local anesthetic drugs, these drugs intensify the sensory block without increasing the sympathetic block while achieving a satisfactory quality of spinal anesthesia at a much lower dose of local anesthetics drugs. Fentanyl is a potent, commonly used centrally acting opioid that is usually combined with the local anesthetic agent for perioperative anesthesia and analgesia.9,10 Fentanyl binds to opioid receptors, mainly the mu opioid receptor. Buprenorphine is an adjuvant used in spinal anesthesia, it is a mixed agonist-antagonist with high affinity at both mu and kappa opioid receptors.11 It is a weak kappa-opioid receptor antagonist and weak partial mu-opioid receptor agonist. Buprenorphine is readily available as compared to fentanyl, especially in peripheral cities.
We compared the effects of intrathecal administration of fentanyl and buprenorphine with hyperbaric bupivacaine, on block characteristics in elective gynecological surgeries.
Methodology
After Institutional Ethical Committee approval and written informed consent, 63 patients aged 18–65 y, American Society of Anesthesiologist (ASA) grade I or II, scheduled for lower abdominal gynecological surgery were included in this prospective, randomized trial. Patients with a history of hypertension, diabetes mellitus, morbid obesity, hypersensitivity to studied drugs and emergency surgery were excluded from study.
All patients were randomly assigned to one of the two equal groups; Group F to receive 0.5% hyperbaric bupivacaine 2.5 ml with fentanyl 25 µg; and Group B to receive 0.5% hyperbaric bupivacaine 2.5 ml with buprenorphine 75 µg. Total volume of the drugs administered intrathecally was 3 ml in both of the groups. Randomization was performed by an anesthesiologist involved in studied drug preparation, who did not participate in drug administration. Further procedure and monitoring were performed by another investigator unaware of the group allocation; patients were also blinded to the drug regimen utilized for spinal anesthesia in them.
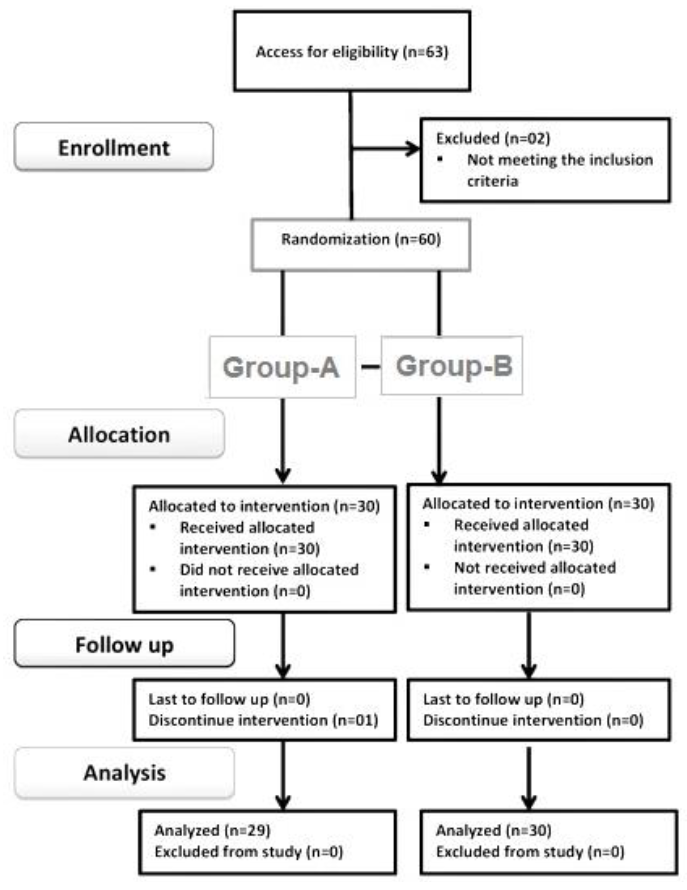 Figure 1: CONSORT flow diagram |
Duration of sensory-motor block was measured from the point of commencement of spinal anesthesia. The upper level of sensory block was assessed bilaterally by pinprick method. Modified Bromage scale was used to assess motor block; 0 = Patient able to move hip, knee, ankle, 1 = Unable to move hip, able to move knee and
| Table 1: Demographic and baseline parameters of patient studied (n = 30). | ||||
| Parameters | Group F | Group B | t-value | p-value |
| Age (y) | 40.33 ± 10.90 | 40.73 ± 10.17 | 0.147 | 0.884 |
| Weight (Kg) | 63.23 ± 13.30 | 60.90 ± 11.01 | 0.740 | 0.462 |
| Height (m) | 1.62 ± 0.096 | 1.63 ± 0.08 | 0.450 | 0.655 |
| BMI Kg/m2 | 24.08 ± 3.56 | 22.87 ± 3.47 | 1.344 | 0.184 |
| Baseline HR (min) | 86.77 ± 8.53 | 86.07 ± 7.71 | 0.333 | 0.740 |
| Baseline SBP (mmHg) | 124.03 ± 16.46 | 128.30 ± 16.52 | 1.002 | 0.321 |
| ASA Status ǀ/ǀǀ | 20/10 | 21/09 | 0.077 | 0.781 |
| Data presented as mean ± SD or numbers. p < 0.05 considered as significant. BMI = Body Mass Index, HR = Heart rate, SBP = Systolic blood pressure | ||||
| Table 2: Comparison of onsets and duration of sensory and motor block between two groups (n = 30) | ||||
| Parameters | Group F | Group B | t-value | p-value |
| Onset of Sensory Block (Min) | 2.96 ± 0.35 | 3.48 ± 0.35 | 5.670 | < 0.001 |
| Onset Of Motor Block (Min) | 3.85 ± 0.38 | 4.12 ± 0.36 | 2.803 | 0.007 |
| Duration Of Sensory Block (Min) | 234.13 ± 34.59 | 270.10 ± 42.22 | 3.609 | 0.001 |
| Duration Of Motor Block (Min) | 192.97 ± 17.67 | 188.03 ± 16.29 | 1.125 | 0.265 |
| Data presented as mean ± SD or numbers. p < 0.05 considered as significant, SD = Standard deviation | ||||
| Table 3: Comparison of side–effects and complications amongst the study groups (n = 3) | ||||
| Parameters | Group F | Group B | t-value | p-value |
| Nausea | 6 (20) | 12 (50) | 5.934 | 0.015 |
| Vomiting | 4 (13.3) | 16 (53.33) | 10.800 | 0.001 |
| shivering | 2 (6.7) | 12 (40) | 9.317 | 0.002 |
| Data is presented as number (percentage). p < 0.05 considered as significant | ||||
ankle, 2 = Unable to move hip and knee, able to move ankle, 3 = Unable to move hip, knee and ankle. Assessment of block was performed every 2 min after the spinal anesthesia till the T6 dermatomal level and Bromage score of 3 was achieved. After that it was performed at every 20 min, until the recovery of S2 dermatome (duration of the sensory block) and Bromage score of “0” (duration of the motor block) was achieved. Hemodynamic variables were monitored continuously and any incidence of associated side-effects was documented till sensory-motor levels regressed to above-mentioned threshold during the postoperative period.
Statistical analysis: Sample size was calculated by the following formula;
For two mean n = 2S2(Z1-α/2+Z1-β)2 /2. Where, S = pooled standard deviation, n = required number of samples for each group, 1-β = power, 1-α = level of confidence, d = mean difference, S = combined standard deviation, α = 5% level of significance at two tailed test, 80% is the power of the study with one-to-one ratio. Sample size required for each group was calculated to be 30 (n = 30).
Statistical analysis was performed using statistical package for the social sciences (SPSS), Version 23.0. IBM Corp., NY). Simple descriptive statistics were used, e.g., mean ± SD for quantitative variables, and frequency with percentage for categorized variables. The data was analyzed using Chi square test and Fisher’s exact test. For comparing two groups of means independent student’s t test was used. P-value < 0.05 was considered as statistically significant.
Results
Out of 63 patients, 60 patient completed study and 3 were excluded (Figure 1). The study groups were comparable in terms of demographic profile, baseline hemodynamic variables and ASA status (Table 1).
The mean onset of sensory block (onset time of T10 level sensory block) was significantly earlier in Group F (2.96 ± 0.35 min) than Group B (3.47 ± 60.35 min) (p < 0.001) (Table 2). Whereas, the mean duration of sensory block was significantly prolonged in Group B (270.10 ± 42.22 min) compared to Group F (234.13 ± 34.58 min) (p value < 0.05) (Table 2).
The mean time for onset of motor block was significantly earlier in Group F (3.85 ± 00.38 min) when compared with Group B (4.12 ± 0.36 min) (p < 0.001) (Table 2). Whereas, the duration of motor block (Modified Bromage score to become 0) was comparable in both the groups (P > 0.05) (Table 2).
Duration of analgesia (time to first analgesia requirement after the study drugs were injected intra-thecally) was significantly prolonged in Group B (516.50 ± 47.25 min) than Group F (371.20 ± 60.03 min) (P < 0.001).
Regarding side effects of study medications, nausea was found in both the groups, but the incidence was higher in Group B (50%) as compared to Group F (20%). Similarly, the incidence of vomiting and shivering was higher in Group B (53.3% and 40% respectively) than in Group F (13.3% and 6.7% respectively) (Table 3).
Discussion
For this study, we selected two opioids belonging to two different groups. Both are lipophilic drugs, but while fentanyl is a pure agonist, buprenorphine is a partial agonist. In our study, the onset of sensory and motor block was earlier in fentanyl group than buprenorphine group. This finding was supported by the study of Khan et al.12 in which sensory and motor blockade was achieved faster in fentanyl group than buprenorphine. The mean duration of sensory block was significantly longer in Group B (p = 0.001) than Group F in our study. The longer duration of buprenorphine is because of its higher affinity towards opioid receptor and high lipid solubility.10 Mean duration of motor block was comparable between two groups (p = 0.265). The finding was consistent with the study by Khan et al.12
Buprenorphine has a prolonged duration of action due to its complex receptor kinetics. It has a very high affinity to opiate receptors. It forms an avid complex with the receptor, tends to persist for long duration of period. The opiate receptor affinity for buprenorphine is 50 times more than that of morphine.13,14 The high lipid solubility and high affinity for opiate receptors of buprenorphine explains buprenorphine’s prolonged duration of action when compared to other lipid soluble drugs like fentanyl which produces short lived analgesia due to its rapid clearance from spinal cord sites.15
Nausea and vomiting are due to rostral spread of opioid in CSF to intrathecal structures including vomiting center and chemoreceptor trigger zone in the vascularized area postrema in the floor of fourth ventricle. In our study, the incidence of nausea, vomiting and shivering was higher in the buprenorphine group than the fentanyl group.
None of the patients in our study exhibited any untoward serious cardiovascular, respiratory or CNS effects, which further proved that buprenorphine is a safe and suitable agent for postoperative pain relief by intrathecal route. When a longer duration of postoperative pain relief is needed, buprenorphine can be a suitable drug for gynecological patients because of prolonged duration of action.
Conclusion
Although buprenorphine had a relatively higher incidence of side effects, especially nausea and vomiting, most of the patients tolerated these side effects well. Therefore, it can be a good alternative option as an adjuvant to spinal anesthesia in patients undergoing abdominal gynecological surgeries, especially to prolong the duration of the postoperative analgesia.
Limitations
The present study had certain limitations. It was conducted with a small sample size. Therefore, we feel that a few randomized double-blind control trials with a larger sample size of patients may be conducted to further confirm its usefulness.
Conflict of interest
None declared by the authors.
Authors’ contribution
YS, AKY: Concept and design, Literature search, conduct of study, manuscript preparation, data analysis, manuscript editing, and manuscript review.
VB, PD, RKV: Concept and design, Literature search, data analysis, critical manuscript editing, manuscript review.
SV: Concept and design, Literature search, conduct of study, data analysis, manuscript editing,
References
- Di Cianni S, Rossi M, Casati A, Cocco C, Fanelli G. Spinal anesthesia: an evergreen technique. Acta Biomed. 2008;79:9–17. [PubMed]
- Kuthiala G, Chaudhary G. Ropivacaine: A review of its pharmacology and clinical use. Indian J Anaesth. 2011;55:104-10. [PubMed] DOI: 4103/0019-5049.79875
- Luck JF, Fettes PD, Wildsmith JA. Spinal anaesthesia for elective surgery: A comparison of hyperbaric solutions of racemic bupivacaine, levobupivacaine, and ropivacaine. Br J Anaesth. 2008;101:705-10. [PubMed] DOI: 1093/bja/aen250
- Uppal V, Retter S, Shanthanna H, Prabhakar C, McKeen DM. Hyperbaric versus isobaric bupivacaine for spinal anesthesia: systematic review and meta-analysis for adult patients undergoing noncesarean delivery surgery. Anesth Analg. 2017;125:1627–37. [PubMed] DOI: 1213/ANE.0000000000002254
- Pargger H, Hampl KF, Aeschbach A, Paganoni R, Schneider MC. Combined effect of patient variables on sensory level after spinal 0.5% plain bupivacaine. Acta Anaesthesiol Scand. 1998;42:430–34. [PubMed] DOI: 1111/j.1399-6576.1998.tb05137.x
- Kanazi GE, Aouad MT, Jabbour-Khoury SI, Al Jazzar MD, Alameddine MM, Al-Yaman R et al. Effect of low-dose dexmedetomidine or clonidine on the characteristics of bupivacaine spinal block. Acta Anesthesiol Scand. 2006;50:222–7. [PubMed] DOI: 1111/j.1399-6576.2006.00919.x
- Boussofara M, Carlès M, Raucoules-Aimé M, Sellam MR, Horn JL. Effects of intrathecal midazolam on postoperative analgesia when added to a bupivacaine-clonidine mixture. Reg Anesth Pain Med. 2006;31:501–5. [PubMed] DOI: 1016/j.rapm.2006.05.013
- Swain A, Nag DS, Sahu S, Samaddar DP. Adjuvants to local anesthetics: Current understanding and future trends. World J Clin Cases. 2017;5:307–323. [PubMed] DOI: 10.12998/wjcc.v5.i8.307
- Singh I, Gupta M, Mahawar B, Gupta A. Comparison of effect of intrathecal sufentanil-bupivacaine and fentanyl-bupivacaine combination on postoperative analgesia. Indian J Anaesth. 2008;52:301-4. [Free Full Text] DOI: 4103/0019-5049.138985
- Cowan CM, Kendall JB, Barclay PM, Wilkes RG. Comparison of intrathecal fentanyl and diamorphine in addition to bupivacaine for caesarean section under spinal anaesthesia. Br J Anaesth. 2002;89:452-8. [PubMed]
- Sheikh S, Kiran M. Intrathecal buprenorphine for postoperative analgesia: A prospective double blind randomized study. J Anaesth Clin Pharmacol. 2010;26(1):35-8. [Free Full Text]
- Khan FA, Hamdani GA. Comparison of intrathecal fentanyl and buprenorphine in urological surgery. J Pak Med Assoc. 2006;56:277–81. [PubMed]
- Lutfy K, Eitan S, Bryant CD, Yang YC, Saliminejad N, Walwyn W, et al. Buprenorphine-induced antinociception is mediated by mu-opioid receptors and compromised by concomitant activation of opioid receptor-like receptors. J Neurosci. 2003:12;23:10331-7. [PubMed] DOI: 1523/JNEUROSCI.23-32-10331.2003
- Lutfy K, Cowan A. Buprenorphine: a unique drug with complex pharmacology. Curr Neuropharmacol. 2004;2(4):395-402. [PubMed] DOI: 2174/1570159043359477
- Boas RA, Villiger JW. Clinical actions of fentanyl and buprenorphine. The significance of receptor binding. Br J Anaesth. 1985;57:192-6. [PubMed] DOI: 1093/bja/57.2.192