Ivana Purnama Dewi1,2,3, Kristin Purnama Dewi1,4, Tiniwati Tanojo2, Eka Prasetya Budi Mulia1,3, Meity Adriana1,3
Author affiliations:
Abstract
Patients undergoing coronary artery bypass grafting (CABG) have a risk of postoperative complications resulting in long hospital stays and even death. In patients undergoing CABG, cardiac rehabilitation is recognized as an essential adjunct therapy for secondary prevention. Encouraging exercise-based cardiac rehabilitation might help speed up the postoperative recovery process, decrease in-hospital stay, prevent complications, and reduce public health costs. Exercise-based cardiac rehabilitation in both pre and post CABG surgery, consist of exercise or physical activity, education and counselling, inspiratory strength muscle conditioning, effective cough exercises, chest physiotherapy, breathing exercises, and gymnastics for respiratory muscle stretching. This literature review aims to analyze the exercise-based cardiac recovery of patients undergoing CABG and its effects in terms of physiological and clinical criteria, such as cardiovascular outcomes, aerobic ability, quality of life, and mortality.
Key words: Cardiac rehabilitation; Coronary artery bypass grafting; Exercise; Physical activity
Citation: Dewi IP, Dewi KP, Tanojo T, Mulia EPB, Adriana M. Pearls of exercise-based cardiac rehabilitation frame in post coronary artery bypass graft. Anaesth. pain intensive care 2021;25(3):367–375. DOI: 10.35975/apic.v25i3.1383
Received: November 2, 2020, Reviewed: February 22, 2021, Accepted: March 26, 2021
Introduction
Coronary artery disease (CAD) is a cardiac abnormality caused by narrowing or obstructing coronary arteries that supply blood to the heart. CAD is one of the cardiovascular diseases (CVD) responsible for 85% death worldwide.1 Since the 1960s, coronary artery bypass grafting (CABG) has been performed as a general surgery to stimulate blood supply in stenotic coronary arteries.2 The risk of future ischaemic events that could extend to atherosclerosis in the grafted veins can also be present in patients who have had CABG.3,4 Other problems that often occur after CABG are pain, sputum builds up, bronchopneumonia, pleural effusion, pericardial effusion, muscle spasm, lower extremity edema (if the graft is taken from the lower extremity), and surgical scar infection. Some patients may have difficulty returning to everyday daily life due to muscle weakness after surgery due to inactivity and the misconception that activity should be limited. This reason can ultimately harm the patient quality of life and psychological status.5–7
Cardiac rehabilitation (CR) has shown significant advantages for post CABG patients. These advantages include >30% mortality reduction,8 acceptance rate of returns to normal dialy life,9–11 decreased major cardiovascular risk factors manifestation, including dyslipidemia, high blood pressure (BP), smoking, hyperglycemia,12 and adverse psychological outcomes.13,14 Therefore CR is crucial to maintain positive results and maintain a healthy life after surgery.
Several strategies are involved in cardiac recoveries, such as routine physical exercise, medical treatment (e.g., drugs), balanced diet, risk factor management education, and stress management.14,15 This literature review aims to describe exercise-based cardiac rehabilitation in patients undergoing CABG surgery.
Physiology of physical exercise
The physiology of physical exercise uses several basic principles and the following terms:
The term VO2 peak should be favored when patients do not exceed their VO2 max.17 In people who are awake at rest, the metabolic equivalent (MET) is defined as the need for oxygen. MET is 3.5 ml/kg body weight/min equivalent.
When patients do not reach their VO2 max, and the term VO2 peak should be preferred. VO2 peak is the highest level achieved by patients if they do not meet the VO2 max criteria.17 A metabolic equivalent (MET) is defined as the oxygen demand in individuals who are awake at rest. MET is equal to 3.5 ml/kg body weight/min.
By multiplying the heart rate (HR) and systolic BP, MO2 can be measured. MO2 is determined not by external work-level preparation but by preparation work speed compared to full training ability. VT is the VO2 curve's divergence and the carbon dioxide (VCO2) production curve, which is due to lactic acid production. Training resistance is shown by VT, which reflects the highest continuous working speed that can be sustained during submaximal exercise.
Cardiac rehabilitation frame post-CABG
Cardiac rehabilitation pays more attention to current clinical status and cardiac pumps, such as left ventricular ejection fraction (LVEF). During hospitalization, treadmill or ergo cycle monitoring is not regularly performed. It is unacceptable to stop exercise based on maximum HR. Moreover, beta-blocker treatment is given to most patients, but their HR response to exercise will decrease. Several clinical criteria, such as BP variations, signs of arrhythmia, dyspnea (Borg scale > 14), rales, syncope or pre-syncope, and angina or claudication, should be considered during exercise. Besides, for surgical knitting, upper body movement should be preserved for four weeks. Three or four months push-ups and other strenuous exercises s needed.
To evaluate baseline perfusion after CABG, some physicians need functional imaging tests such as cardiac scintigraphy. Scintigraphy can be performed with pharmacological stress or treadmill test. This data may be viewed as supplementary information on cardiovascular physiological status, such as chronotropic balance, maximum HR achieved, METs and VO2,16,18 whether the measurement is conducted in combination with a treadmill examination.
Cardiac rehabilitation is a comprehensive long-term service that includes medical evaluation, prescribing exercises, modifying cardiac risk factors, education, counseling, and behavior intervention. The role of CR has started since the pre-CABG procedure and continued after the CABG procedure. The goals of CR include returning patients to optimal physical, mental, social, and vocational conditions, increasing their functional capacity, increasing coronary blood flow/ collateral system, improving the efficiency of the cardiovascular system, improving risk factors, increasing daily life activities, and increasing quality of life.
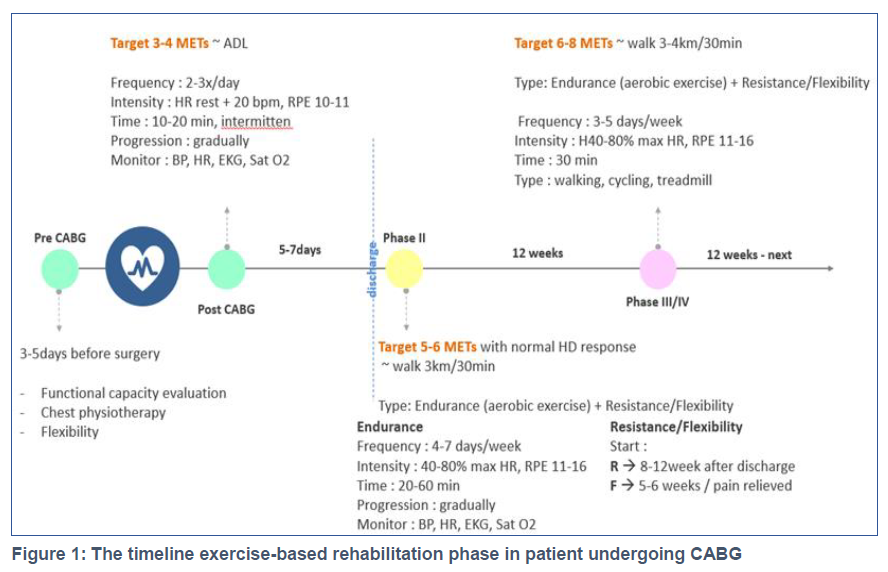
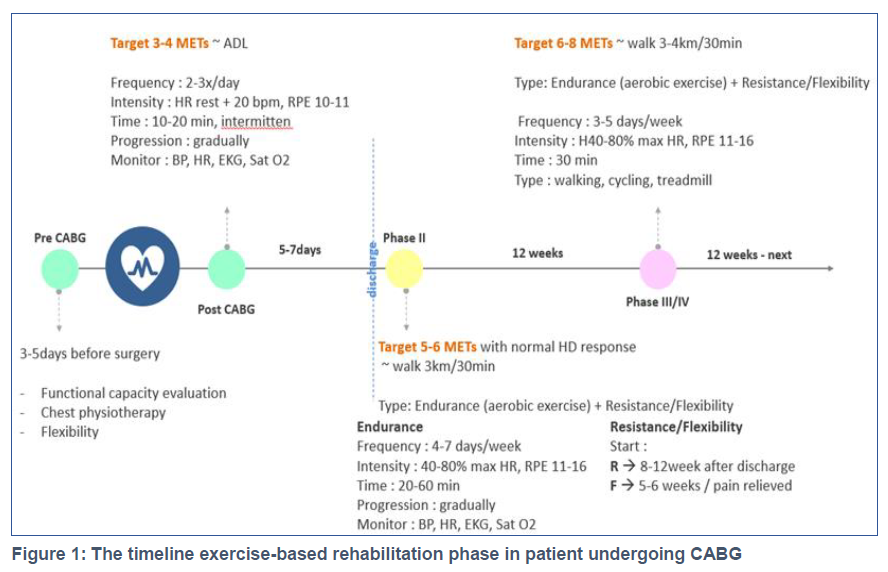
Traditionally, the CR program can be divided into several phases: Phase I performed when the patient was admitted to the hospital before, and after CABG, phase II to phase III / IV was carried out by post-CABG patients who had been discharged from the hospital which could be beneficial for preventing recurrence (Figure 1).
Phase I Rehabilitation (inpatient phase)
 .
.
During the hospitalization, phase I was carried out. This phase's focus is to ensure that the patient is discharged in the best psychological and physical state condition. Rehabilitation in Phase I will bring a healthy and efficient life for the patient. In this step, a mix of physical activity of moderate intensity and stress control strategies and risk factors education is demonstrated. Due to enhancement of clinical treatment and/or utilization of interventional techniques, phase 1 starts after the patient is considered clinically competent. Owing to shorter hospitalizations, the length of this stage has declined in recent years.16,18 It is also possible to split Phase I into two phases: pre- and post-CABG operation.
Pre-CABG procedure
The goal of pre-CABG rehabilitation is to prevent post-CABG complications, especially pulmonary complications. The advantages of pre-rehabilitation in CABG patients are reducing the duration of use of the ventilator, reducing pulmonary complications, and improving lung function.
This rehabilitation program is different for each patient, which is individualized. Prior to rehabilitation, patients can be evaluated first using a 6-minute walking test (6MWT). The objective of 6MWT is to determine the patient's functional ability using METs units. The assessment method is by measuring the distance traveled by the patient walking in a predetermined field within 6 minutes, then converted to the VO2max value and METs unit value. By knowing the patient's functional capacity as expressed by METs, an exercise program can be prescribed.
Cardiovascular rehabilitation programs that can be done pre-CABG include chest physiotherapy, breathing exercises consisting of deep breathing exercises and diaphragmatic breathing exercises, incentive spirometry exercises, cough exercises, and flexibility exercises for the head, neck, shoulder joints, upper and lower extremities.
Post-CABG procedure
The rehabilitation program begins with a patient assessment and educates the patient that the exercise is needed to prevent postoperative complications. Psychosocial management is also needed to manage the patient's psychology, anxiety, or fear of movement after CABG. Early mobilization and physical exercise / reconditioning are essential to restore and improve the condition of functional abilities and prevent complications due to prolonged bed rest. It is important to know that before exercising, we must pay attention to risk factors, namely blood pressure, lipid profile, blood sugar, whether the patient is a smoker or obese. Here also needs nutritional counseling to improve risk factors, occupational therapy to support appropriate physical activity, and provide vocational recommendations according to functional capacity progress.
Mobilization and exercises are carried out when the patient's condition is stable, including no new/recurring chest pain in the previous 8 hours, HR and electrocardiogram (ECG) are normal and stable in the previous 8 hours, no sign of decompensated heart failure (e.g., dyspnea), no elevation of cardiac marker enzymes (CK-MB or troponin). Types of physical exercise for Phase I in post-CABG patients include breathing exercises and chest expansion, coughing exercises to clear the sputum, incentive spirometry exercise, broad motion exercises for the upper and lower extremities, extensive exercises for neck and shoulder joint motion, ankle pumping exercises (especially when grafting taken from the lower leg), mobility training, and training activities of daily life. The target of physical training in Phase I is mainly to achieve the target of daily living activities, which 3-4 METs.
Physical training load using prescription according to FITT (frequency, intensity, time, type). The frequency is given 2-3 times a day. The intensity corresponds to resting HR+20 beats per minute (bpm) and rating of perceived exertion (RPE) 10-11. Time/duration 10-20 minutes, intermittent, and the load is increased gradually. During physical exercise, blood pressure, HR, ECG, O2 saturation, cardiac symptoms such as chest pain, palpitations, tightness, and fatigue should be monitored.
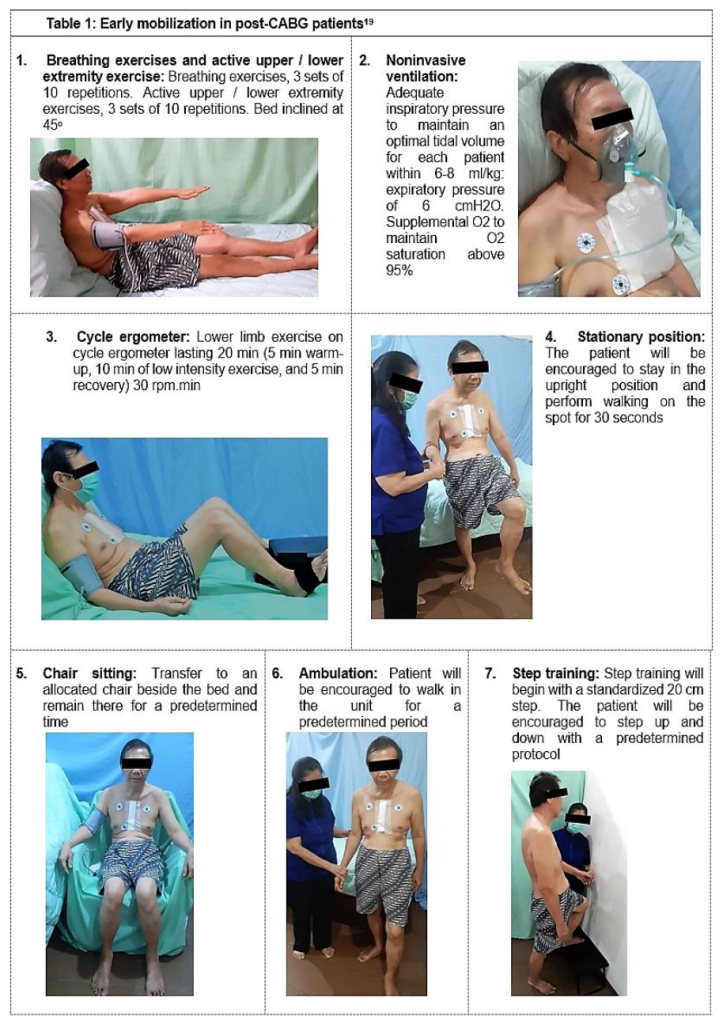
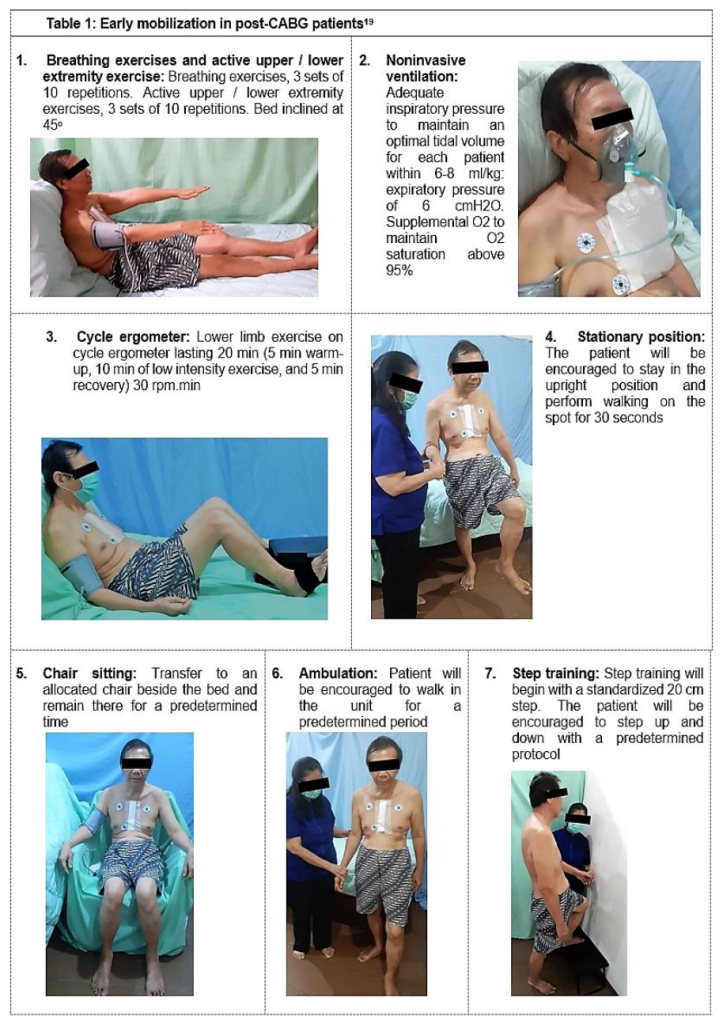
Early mobilization steps in post-CABG patients can be performed, as presented in Table 1.19 Criteria for physical exercise should be stopped if there are any of the following signs: an increase in systolic blood pressure greater than 40 mmHg or a decrease greater than 10 mmHg; HR increased by more than 30 bpm or HR greater than 130 bpm; ventricular/atrial arrhythmias, first or second-degree atrioventricular block; exercise intolerance, angina pectoris, dyspnea, palpitations; ECG changes leading to ischemia.
Before the patient is discharged from the hospital, it is necessary to evaluate functional capacity by performing 6MWT to evaluate activities of daily life that can be carried out safely. Also, education is also given on the modification of life habits before surgery for secondary prevention, including routine aerobic exercise, BP control, blood sugar and cholesterol levels, smoking cessation, and stress management.
Phase II Rehabilitation (outpatient phase)
Phase II is the first out-of-hospital training step. This phase starts shortly after and/or a few days after discharge, usually within 1-3 weeks, with physical activity supervision. Phase II duration is usually 3–6 months, and in some cases, maybe longer. This phase is carried out in a hospital gym or other environment suitable for physical training. Doctors, physiotherapists, physical education practitioners,. Phase II works with a physiotherapist and/or physical clinicians, nutritionists, and psychiatrists should be part of the ideal team education teacher supervising suitable for physical training. Doctors, physiotherapists, physical education practitioners,. Phase II works with a physiotherapist and/or physical clinicians, nutritionists, and psychiatrists should be part of the ideal team education teacher supervising sessions. The training schedule must be individualized in terms of frequency, strength, duration, training modality, and development. In addition to the likelihood of ensuring oxygen saturation, ECG testing, and blood glucose assessment, there should still be means to calculate precise HR and BP. This process also involves an outreach program targeted at behavioral change, focusing on diet re-education and smoking cessation approaches.16,18 The goals of this Phase II are implementing an exercise program, safe and effective physical activity, supervising and monitoring for the detection of changes in clinical status, returning to daily, work, and recreational activities or modification according to clinical status, and educating patients and families to optimize secondary prevention with lifestyle modifications.
Types of training given in this phase include endurance and resistance training. Exercise can be given after an exercise stress test. The exercise stress test results can be used for counseling regarding daily activities at home, work, and recreational activities that can be carried out safely after the patient is discharged from the hospital. The functional capacity in METs is used to estimate the patient's tolerance for specific activities. In addition, phase II exercises can also be given resistance and flexibility exercise, which aim to increase the range of motion (ROM), relieve pain, and restore/increase muscle strength or endurance. In this phase, it is necessary to pay attention to sternal instability signs and symptoms when doing physical exercise.
Flexibility training can be started 3-5 weeks after the patient is discharged from the hospital. The goal of this exercise is to increase ROM and reduce the risk of injury. Resistance exercises can be started 8-12 weeks after the patient is discharged from the hospital. At the end of Phase II, a retraining test is carried out to determine the functional capacity with the target of achieving 5-6 METs.
Phase III Rehabilitation (maintenance phase)
This phase is the most important phase where the benefits obtained during Phase II can be lost if the patient stops doing physical exercise. The estimated duration of this phase is 6-24 months. This phase is not only direct follow-up care after Phase II, but can also be initiated at any phase of the patient where the patient may not have to follow the previous phase.16,18 The target functional capacity in this phase is 6-8 METs. The American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR) and the American College of Sports Medicine (ACSM) recommend the use of either hospital-based or community-based programs. Hospital-based programs are carried out in a structured manner and under the supervision of a physiotherapist. In contrast, community-based programs are only performed on low-risk patients. Aerobic and resistance training can be continued at this phase.
Phase IV Rehabilitation
Phase IV is a long-term program with unlimited duration. Activities are not necessarily monitored and must balance the availability of time regarding leisure physical activity with the continuation of the physical fitness program and patient needs. It is, therefore essential to consider the available supplies and human resources. At this point, the patient should be assessed and focused in practice with multiple controlled exercise sessions after each medical examination, especially when conducting an ergometric test. The period for the ergometric evaluation to be carried out does not extend one year. Improving and sustaining physical health is the main aim of this point. The CR team can routinely and consistently contact patients, including telephone, at least every six months.16,18
Each trainer may choose to conduct different activities during each cardiac session, including proper aerobic training that can be done with an ergo cycle, a sliding band, a climber or just a walk directed by qualified personnel, resistance training, strength training, balance training, endurance training and, in phases III and IV, specific exercises that are comparable to the dialy activity. As for aerobic exercise, two forms of training can be performed: CAT and IAT. The application of loads without delay, such that, without breaks or rest periods during work, is defined by CAT. This technique may be comprehensive or intensive, noticing variations in training strength between the two. The IAT approach requires periods for recovery. When the exercise is high or moderate intensity, the active interval is used. In contrast, if the patient's functional capacity is low, the passive recovery interval is used.
Benefits of physical exercise-based post-CABG cardiac rehabilitation
In the absence of adequate research to determine the impact of IAT versus CAT as a rehabilitation program on mortality or significant coronary events after CABG, some small sample size studies used hemodynamic proxy endpoints and ventilation parameters to measure the efficiency of exercise. In this way, VO2peak is strongly predictive of mortality and is assessed for four weeks and six months in patients completing IAT versus Continuous Mild Training (CMT) after CABG. The VO2 peak in the IAT and CMT groups was assessed at baseline, four weeks, and after six months, indicating similar short-term changes. However, there was a better long-term effect in the IAT group after CABG.20 In a bicycle ergometer protocol, another clinical trial tested the IAT vs CAT program for 3.5 weeks. Nine patients in each group did the exercises 24-26 days after CABG.21 The IAT encourages increased physical efficiency at the end of the protocol, lower resting HR (-9 bpm versus -4 bpm), lower intensity of pressurized products at rest, and lower lactate.21 Catecholamines did not vary between groups. The authors concluded that IAT is more acceptable for physical performance enhancement and is more effective than CAT in maintaining cardiac function.21 Others also tested rate pressure products, and their measurements on a comparable study of CAD patients attending CABG and then being trained. In either the CAT or IAT program found a significant reduction in rest and overall rate pressure products in the IAT group only. An indirect index of myocardial oxygen consumption in CAD patients is the rate-pressure product.
Endothelial activity is characterized by flow-mediated dilatation and acts as a prognostic marker for cardiovascular events. As found in experiments testing flow-mediated brachial artery dilatation after IAT in post-infarct heart failure, IAT also increases endothelial function.22 However, there is a lack of patient trials after CABG and IAT. A systematic analysis of patients with cardiovascular and cerebrovascular disease,23 involving 20 trials, has shown that high-intensity aerobic interval training (HIIAT) is equivalent to mild CAT by improving endothelial activity as assessed by flow-mediated dilatation, the bioavailability of nitric oxide and circulating biomarkers.
On the other hand, among many cardiac criteria assessed by echocardiography, there is debate about whether physical exercise can enhance cardiac function. One analysis tested patients after CABG 22 and found no increase in systolic annular velocity, mitral annular excursion, late diastolic mitral flow velocity (A wave), early diastolic mitral velocity, late diastolic mitral velocity, deceleration of early diastolic mitral velocity ejection fraction, end-diastolic volume, or end-systolic volume after four weeks of IAT. The findings were close to the baseline, except that after four weeks of IAT, the peak initial mitral diastolic flow velocity (E wave) showed a substantial decline. However, IAT demonstrated a decline in left ventricular end-diastolic and systolic volume in patients who experienced heart failure following infarction but did not undergo CABG and underwent physical exercise, and the left ventricular ejection fraction rose from 28 ± 7.3% to 38 ± 9.8%, with improved findings for IAT compared to CMT.22
Recommendations
On the basis of available data, we strongly recommend that the cardiac surgery teams incorporate the services of cardiac rehabilitation specialists with them for regular post CABG exercise-based programmes. The exercise programme may be strted immediately after a patient is off mechanical ventilation and is attentive nd can respond to the directions.
Conclusion
The cardiac rehabilitation program is a comprehensive, long-term program involving medical evaluation, supervised exercise, modification of cardiac risk factors, education, and counseling. Exercise-based cardiac rehabilitation of CABG restricts the physiological and psychological effects of heart disease, controls heart failure symptoms, stabilizes or reverses the atherosclerotic process, improves psychosocial status, and reduces the risk of sudden death recurrent infarction. Cardiac rehabilitation reduces risk factors, increases physical exercise capacity, medication adherence to secondary preventive therapy, and survival after CABG surgery.
Authors’ contribution
IPD and TT conceived the idea and designed the report.
IPD, KPD and EP were major contributors in writing the manuscript.
TT and MA supervised the article content.
All authors read and approved the final manuscript.
Conflict of interest
The authors declare no conflict of interest.
References
Author affiliations:
- Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia.
- Faculty of Medicine, Duta Wacana Christian University, Yogyakarta, Indonesia.
- Department of Cardiology and Vascular Medicine, Faculty of Medicine, Universitas Airlangga - Soetomo General Hospital, Surabaya, Indonesia.
- Department of Pulmonology and Respiratory Medicine, Dr. Soetomo General Hospital, Surabaya, Indonesia.
Abstract
Patients undergoing coronary artery bypass grafting (CABG) have a risk of postoperative complications resulting in long hospital stays and even death. In patients undergoing CABG, cardiac rehabilitation is recognized as an essential adjunct therapy for secondary prevention. Encouraging exercise-based cardiac rehabilitation might help speed up the postoperative recovery process, decrease in-hospital stay, prevent complications, and reduce public health costs. Exercise-based cardiac rehabilitation in both pre and post CABG surgery, consist of exercise or physical activity, education and counselling, inspiratory strength muscle conditioning, effective cough exercises, chest physiotherapy, breathing exercises, and gymnastics for respiratory muscle stretching. This literature review aims to analyze the exercise-based cardiac recovery of patients undergoing CABG and its effects in terms of physiological and clinical criteria, such as cardiovascular outcomes, aerobic ability, quality of life, and mortality.
Key words: Cardiac rehabilitation; Coronary artery bypass grafting; Exercise; Physical activity
Citation: Dewi IP, Dewi KP, Tanojo T, Mulia EPB, Adriana M. Pearls of exercise-based cardiac rehabilitation frame in post coronary artery bypass graft. Anaesth. pain intensive care 2021;25(3):367–375. DOI: 10.35975/apic.v25i3.1383
Received: November 2, 2020, Reviewed: February 22, 2021, Accepted: March 26, 2021
Introduction
Coronary artery disease (CAD) is a cardiac abnormality caused by narrowing or obstructing coronary arteries that supply blood to the heart. CAD is one of the cardiovascular diseases (CVD) responsible for 85% death worldwide.1 Since the 1960s, coronary artery bypass grafting (CABG) has been performed as a general surgery to stimulate blood supply in stenotic coronary arteries.2 The risk of future ischaemic events that could extend to atherosclerosis in the grafted veins can also be present in patients who have had CABG.3,4 Other problems that often occur after CABG are pain, sputum builds up, bronchopneumonia, pleural effusion, pericardial effusion, muscle spasm, lower extremity edema (if the graft is taken from the lower extremity), and surgical scar infection. Some patients may have difficulty returning to everyday daily life due to muscle weakness after surgery due to inactivity and the misconception that activity should be limited. This reason can ultimately harm the patient quality of life and psychological status.5–7
Cardiac rehabilitation (CR) has shown significant advantages for post CABG patients. These advantages include >30% mortality reduction,8 acceptance rate of returns to normal dialy life,9–11 decreased major cardiovascular risk factors manifestation, including dyslipidemia, high blood pressure (BP), smoking, hyperglycemia,12 and adverse psychological outcomes.13,14 Therefore CR is crucial to maintain positive results and maintain a healthy life after surgery.
Several strategies are involved in cardiac recoveries, such as routine physical exercise, medical treatment (e.g., drugs), balanced diet, risk factor management education, and stress management.14,15 This literature review aims to describe exercise-based cardiac rehabilitation in patients undergoing CABG surgery.
Physiology of physical exercise
The physiology of physical exercise uses several basic principles and the following terms:
- physical activity as body movement
- aerobic physical exercise that emphasizes the oxygen transport system
- endurance training which emphasizes the musculoskeletal system
- repeated exercise to strengthen the cardiovascular function (aerobic) or musculoskeletal system (resistance)
The term VO2 peak should be favored when patients do not exceed their VO2 max.17 In people who are awake at rest, the metabolic equivalent (MET) is defined as the need for oxygen. MET is 3.5 ml/kg body weight/min equivalent.
When patients do not reach their VO2 max, and the term VO2 peak should be preferred. VO2 peak is the highest level achieved by patients if they do not meet the VO2 max criteria.17 A metabolic equivalent (MET) is defined as the oxygen demand in individuals who are awake at rest. MET is equal to 3.5 ml/kg body weight/min.
By multiplying the heart rate (HR) and systolic BP, MO2 can be measured. MO2 is determined not by external work-level preparation but by preparation work speed compared to full training ability. VT is the VO2 curve's divergence and the carbon dioxide (VCO2) production curve, which is due to lactic acid production. Training resistance is shown by VT, which reflects the highest continuous working speed that can be sustained during submaximal exercise.
Cardiac rehabilitation frame post-CABG
Cardiac rehabilitation pays more attention to current clinical status and cardiac pumps, such as left ventricular ejection fraction (LVEF). During hospitalization, treadmill or ergo cycle monitoring is not regularly performed. It is unacceptable to stop exercise based on maximum HR. Moreover, beta-blocker treatment is given to most patients, but their HR response to exercise will decrease. Several clinical criteria, such as BP variations, signs of arrhythmia, dyspnea (Borg scale > 14), rales, syncope or pre-syncope, and angina or claudication, should be considered during exercise. Besides, for surgical knitting, upper body movement should be preserved for four weeks. Three or four months push-ups and other strenuous exercises s needed.
To evaluate baseline perfusion after CABG, some physicians need functional imaging tests such as cardiac scintigraphy. Scintigraphy can be performed with pharmacological stress or treadmill test. This data may be viewed as supplementary information on cardiovascular physiological status, such as chronotropic balance, maximum HR achieved, METs and VO2,16,18 whether the measurement is conducted in combination with a treadmill examination.
Cardiac rehabilitation is a comprehensive long-term service that includes medical evaluation, prescribing exercises, modifying cardiac risk factors, education, counseling, and behavior intervention. The role of CR has started since the pre-CABG procedure and continued after the CABG procedure. The goals of CR include returning patients to optimal physical, mental, social, and vocational conditions, increasing their functional capacity, increasing coronary blood flow/ collateral system, improving the efficiency of the cardiovascular system, improving risk factors, increasing daily life activities, and increasing quality of life.
Traditionally, the CR program can be divided into several phases: Phase I performed when the patient was admitted to the hospital before, and after CABG, phase II to phase III / IV was carried out by post-CABG patients who had been discharged from the hospital which could be beneficial for preventing recurrence (Figure 1).
Phase I Rehabilitation (inpatient phase)
 .
.During the hospitalization, phase I was carried out. This phase's focus is to ensure that the patient is discharged in the best psychological and physical state condition. Rehabilitation in Phase I will bring a healthy and efficient life for the patient. In this step, a mix of physical activity of moderate intensity and stress control strategies and risk factors education is demonstrated. Due to enhancement of clinical treatment and/or utilization of interventional techniques, phase 1 starts after the patient is considered clinically competent. Owing to shorter hospitalizations, the length of this stage has declined in recent years.16,18 It is also possible to split Phase I into two phases: pre- and post-CABG operation.
Pre-CABG procedure
The goal of pre-CABG rehabilitation is to prevent post-CABG complications, especially pulmonary complications. The advantages of pre-rehabilitation in CABG patients are reducing the duration of use of the ventilator, reducing pulmonary complications, and improving lung function.
This rehabilitation program is different for each patient, which is individualized. Prior to rehabilitation, patients can be evaluated first using a 6-minute walking test (6MWT). The objective of 6MWT is to determine the patient's functional ability using METs units. The assessment method is by measuring the distance traveled by the patient walking in a predetermined field within 6 minutes, then converted to the VO2max value and METs unit value. By knowing the patient's functional capacity as expressed by METs, an exercise program can be prescribed.
Cardiovascular rehabilitation programs that can be done pre-CABG include chest physiotherapy, breathing exercises consisting of deep breathing exercises and diaphragmatic breathing exercises, incentive spirometry exercises, cough exercises, and flexibility exercises for the head, neck, shoulder joints, upper and lower extremities.
Post-CABG procedure
The rehabilitation program begins with a patient assessment and educates the patient that the exercise is needed to prevent postoperative complications. Psychosocial management is also needed to manage the patient's psychology, anxiety, or fear of movement after CABG. Early mobilization and physical exercise / reconditioning are essential to restore and improve the condition of functional abilities and prevent complications due to prolonged bed rest. It is important to know that before exercising, we must pay attention to risk factors, namely blood pressure, lipid profile, blood sugar, whether the patient is a smoker or obese. Here also needs nutritional counseling to improve risk factors, occupational therapy to support appropriate physical activity, and provide vocational recommendations according to functional capacity progress.
Mobilization and exercises are carried out when the patient's condition is stable, including no new/recurring chest pain in the previous 8 hours, HR and electrocardiogram (ECG) are normal and stable in the previous 8 hours, no sign of decompensated heart failure (e.g., dyspnea), no elevation of cardiac marker enzymes (CK-MB or troponin). Types of physical exercise for Phase I in post-CABG patients include breathing exercises and chest expansion, coughing exercises to clear the sputum, incentive spirometry exercise, broad motion exercises for the upper and lower extremities, extensive exercises for neck and shoulder joint motion, ankle pumping exercises (especially when grafting taken from the lower leg), mobility training, and training activities of daily life. The target of physical training in Phase I is mainly to achieve the target of daily living activities, which 3-4 METs.
Physical training load using prescription according to FITT (frequency, intensity, time, type). The frequency is given 2-3 times a day. The intensity corresponds to resting HR+20 beats per minute (bpm) and rating of perceived exertion (RPE) 10-11. Time/duration 10-20 minutes, intermittent, and the load is increased gradually. During physical exercise, blood pressure, HR, ECG, O2 saturation, cardiac symptoms such as chest pain, palpitations, tightness, and fatigue should be monitored.
Early mobilization steps in post-CABG patients can be performed, as presented in Table 1.19 Criteria for physical exercise should be stopped if there are any of the following signs: an increase in systolic blood pressure greater than 40 mmHg or a decrease greater than 10 mmHg; HR increased by more than 30 bpm or HR greater than 130 bpm; ventricular/atrial arrhythmias, first or second-degree atrioventricular block; exercise intolerance, angina pectoris, dyspnea, palpitations; ECG changes leading to ischemia.
Before the patient is discharged from the hospital, it is necessary to evaluate functional capacity by performing 6MWT to evaluate activities of daily life that can be carried out safely. Also, education is also given on the modification of life habits before surgery for secondary prevention, including routine aerobic exercise, BP control, blood sugar and cholesterol levels, smoking cessation, and stress management.
Phase II Rehabilitation (outpatient phase)
Phase II is the first out-of-hospital training step. This phase starts shortly after and/or a few days after discharge, usually within 1-3 weeks, with physical activity supervision. Phase II duration is usually 3–6 months, and in some cases, maybe longer. This phase is carried out in a hospital gym or other environment suitable for physical training. Doctors, physiotherapists, physical education practitioners,. Phase II works with a physiotherapist and/or physical clinicians, nutritionists, and psychiatrists should be part of the ideal team education teacher supervising suitable for physical training. Doctors, physiotherapists, physical education practitioners,. Phase II works with a physiotherapist and/or physical clinicians, nutritionists, and psychiatrists should be part of the ideal team education teacher supervising sessions. The training schedule must be individualized in terms of frequency, strength, duration, training modality, and development. In addition to the likelihood of ensuring oxygen saturation, ECG testing, and blood glucose assessment, there should still be means to calculate precise HR and BP. This process also involves an outreach program targeted at behavioral change, focusing on diet re-education and smoking cessation approaches.16,18 The goals of this Phase II are implementing an exercise program, safe and effective physical activity, supervising and monitoring for the detection of changes in clinical status, returning to daily, work, and recreational activities or modification according to clinical status, and educating patients and families to optimize secondary prevention with lifestyle modifications.
Types of training given in this phase include endurance and resistance training. Exercise can be given after an exercise stress test. The exercise stress test results can be used for counseling regarding daily activities at home, work, and recreational activities that can be carried out safely after the patient is discharged from the hospital. The functional capacity in METs is used to estimate the patient's tolerance for specific activities. In addition, phase II exercises can also be given resistance and flexibility exercise, which aim to increase the range of motion (ROM), relieve pain, and restore/increase muscle strength or endurance. In this phase, it is necessary to pay attention to sternal instability signs and symptoms when doing physical exercise.
Flexibility training can be started 3-5 weeks after the patient is discharged from the hospital. The goal of this exercise is to increase ROM and reduce the risk of injury. Resistance exercises can be started 8-12 weeks after the patient is discharged from the hospital. At the end of Phase II, a retraining test is carried out to determine the functional capacity with the target of achieving 5-6 METs.
Phase III Rehabilitation (maintenance phase)
This phase is the most important phase where the benefits obtained during Phase II can be lost if the patient stops doing physical exercise. The estimated duration of this phase is 6-24 months. This phase is not only direct follow-up care after Phase II, but can also be initiated at any phase of the patient where the patient may not have to follow the previous phase.16,18 The target functional capacity in this phase is 6-8 METs. The American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR) and the American College of Sports Medicine (ACSM) recommend the use of either hospital-based or community-based programs. Hospital-based programs are carried out in a structured manner and under the supervision of a physiotherapist. In contrast, community-based programs are only performed on low-risk patients. Aerobic and resistance training can be continued at this phase.
Phase IV Rehabilitation
Phase IV is a long-term program with unlimited duration. Activities are not necessarily monitored and must balance the availability of time regarding leisure physical activity with the continuation of the physical fitness program and patient needs. It is, therefore essential to consider the available supplies and human resources. At this point, the patient should be assessed and focused in practice with multiple controlled exercise sessions after each medical examination, especially when conducting an ergometric test. The period for the ergometric evaluation to be carried out does not extend one year. Improving and sustaining physical health is the main aim of this point. The CR team can routinely and consistently contact patients, including telephone, at least every six months.16,18
Each trainer may choose to conduct different activities during each cardiac session, including proper aerobic training that can be done with an ergo cycle, a sliding band, a climber or just a walk directed by qualified personnel, resistance training, strength training, balance training, endurance training and, in phases III and IV, specific exercises that are comparable to the dialy activity. As for aerobic exercise, two forms of training can be performed: CAT and IAT. The application of loads without delay, such that, without breaks or rest periods during work, is defined by CAT. This technique may be comprehensive or intensive, noticing variations in training strength between the two. The IAT approach requires periods for recovery. When the exercise is high or moderate intensity, the active interval is used. In contrast, if the patient's functional capacity is low, the passive recovery interval is used.
Benefits of physical exercise-based post-CABG cardiac rehabilitation
In the absence of adequate research to determine the impact of IAT versus CAT as a rehabilitation program on mortality or significant coronary events after CABG, some small sample size studies used hemodynamic proxy endpoints and ventilation parameters to measure the efficiency of exercise. In this way, VO2peak is strongly predictive of mortality and is assessed for four weeks and six months in patients completing IAT versus Continuous Mild Training (CMT) after CABG. The VO2 peak in the IAT and CMT groups was assessed at baseline, four weeks, and after six months, indicating similar short-term changes. However, there was a better long-term effect in the IAT group after CABG.20 In a bicycle ergometer protocol, another clinical trial tested the IAT vs CAT program for 3.5 weeks. Nine patients in each group did the exercises 24-26 days after CABG.21 The IAT encourages increased physical efficiency at the end of the protocol, lower resting HR (-9 bpm versus -4 bpm), lower intensity of pressurized products at rest, and lower lactate.21 Catecholamines did not vary between groups. The authors concluded that IAT is more acceptable for physical performance enhancement and is more effective than CAT in maintaining cardiac function.21 Others also tested rate pressure products, and their measurements on a comparable study of CAD patients attending CABG and then being trained. In either the CAT or IAT program found a significant reduction in rest and overall rate pressure products in the IAT group only. An indirect index of myocardial oxygen consumption in CAD patients is the rate-pressure product.
Endothelial activity is characterized by flow-mediated dilatation and acts as a prognostic marker for cardiovascular events. As found in experiments testing flow-mediated brachial artery dilatation after IAT in post-infarct heart failure, IAT also increases endothelial function.22 However, there is a lack of patient trials after CABG and IAT. A systematic analysis of patients with cardiovascular and cerebrovascular disease,23 involving 20 trials, has shown that high-intensity aerobic interval training (HIIAT) is equivalent to mild CAT by improving endothelial activity as assessed by flow-mediated dilatation, the bioavailability of nitric oxide and circulating biomarkers.
On the other hand, among many cardiac criteria assessed by echocardiography, there is debate about whether physical exercise can enhance cardiac function. One analysis tested patients after CABG 22 and found no increase in systolic annular velocity, mitral annular excursion, late diastolic mitral flow velocity (A wave), early diastolic mitral velocity, late diastolic mitral velocity, deceleration of early diastolic mitral velocity ejection fraction, end-diastolic volume, or end-systolic volume after four weeks of IAT. The findings were close to the baseline, except that after four weeks of IAT, the peak initial mitral diastolic flow velocity (E wave) showed a substantial decline. However, IAT demonstrated a decline in left ventricular end-diastolic and systolic volume in patients who experienced heart failure following infarction but did not undergo CABG and underwent physical exercise, and the left ventricular ejection fraction rose from 28 ± 7.3% to 38 ± 9.8%, with improved findings for IAT compared to CMT.22
Recommendations
On the basis of available data, we strongly recommend that the cardiac surgery teams incorporate the services of cardiac rehabilitation specialists with them for regular post CABG exercise-based programmes. The exercise programme may be strted immediately after a patient is off mechanical ventilation and is attentive nd can respond to the directions.
Conclusion
The cardiac rehabilitation program is a comprehensive, long-term program involving medical evaluation, supervised exercise, modification of cardiac risk factors, education, and counseling. Exercise-based cardiac rehabilitation of CABG restricts the physiological and psychological effects of heart disease, controls heart failure symptoms, stabilizes or reverses the atherosclerotic process, improves psychosocial status, and reduces the risk of sudden death recurrent infarction. Cardiac rehabilitation reduces risk factors, increases physical exercise capacity, medication adherence to secondary preventive therapy, and survival after CABG surgery.
Authors’ contribution
IPD and TT conceived the idea and designed the report.
IPD, KPD and EP were major contributors in writing the manuscript.
TT and MA supervised the article content.
All authors read and approved the final manuscript.
Conflict of interest
The authors declare no conflict of interest.
References
- Mendis S, Puska P, Norrving B. Global atlas on cardiovascular disease prevention and control. World Health Organization; 2011.
- Reenan J. Indications for bypass surgery. Virtual Mentor. 2004 Feb;6(2):78–81. [PubMed] DOI: 10.1001/virtualmentor.2004.6.2.cprl1-0402
- Smith SC, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update. J Am Coll Cardiol. 2011 Nov;58(23):2432–46. [PubMed] DOI: 10.1016/j.jacc.2011.10.824
- Kulik A, Ruel M, Jneid H, Ferguson TB, Hiratzka LF, Ikonomidis JS, et al. Secondary prevention after coronary artery bypass graft surgery: A scientific statement from the American Heart Association. Circulation. 2015;131(10):927–64. [PubMed] DOI: 10.1161/CIR.0000000000000182
- Parker RD, Adams J. Activity restrictions and recovery after open chest surgery: understanding the patient’s perspective. Baylor Univ Med Cent Proc. 2008 Oct;21(4):421–5. [PubMed] DOI: 10.1080/08998280.2008.11928442
- Firouzabadi MG, Sherafat A, Vafaeenasab M. Effect of physical activity on the life quality of coronary artery bypass graft patients. J Med Life. 2014 Jun;7(2):260–3. [PubMed]
- Perrotti A, Ecarnot F, Monaco F, Dorigo E, Monteleone P, Besch G, et al. quality of life 10 years after cardiac surgery in adults: A long-term follow-up study. Health Qual Life Outcomes. 2019 May;17(1):88. [PubMed] DOI: 10.1186/s12955-019-1160-7
- Goel K, Lennon RJ, Tilbury RT, Squires RW, Thomas RJ. Impact of cardiac rehabilitation on mortality and cardiovascular events after percutaneous coronary intervention in the community. Circulation. 2011 May;123(21):2344–52. [PubMed] DOI: 10.1161/CIRCULATIONAHA.110.983536
- Heran BS, Chen JM, Ebrahim S, Moxham T, Oldridge N, Rees K, et al. Exercise-based cardiac rehabilitation for coronary heart disease. In: Cochrane Database of Systematic Reviews. John Wiley & Sons, Ltd; 2011.
- Thomas E, Lotfaliany M, Grace SL, Oldenburg B, Taylor CB, Hare DL, et al. Effect of cardiac rehabilitation on 24-month all-cause hospital readmissions: A prospective cohort study. Eur J Cardiovasc Nurs. 2019 Mar;18(3):234–44. [PubMed] DOI: 10.1177/1474515118820176
- Flynn KE, Piña IL, Whellan DJ, Lin L, Blumenthal JA, Ellis SJ, et al. Effects of exercise training on health status in patients with chronic heart failure HF-ACTION randomized controlled trial. JAMA - J Am Med Assoc. 2009 Apr;301(14):1451–9. [PubMed] DOI: 10.1001/jama.2009.457
- Gaeini AA, Fallahi AA, Kazemi F. Effects of aerobic continuous and interval training on rate-pressure product in patients after CABG surgery. J Sport Med Phys Fit. 2015;55(1–2):76–83. [PubMed]
- Pourafkari L, Ghaffari S, Shahamfar J, Tokhmechian L, Nader D. The psychological effects of cardiac rehabilitation after coronary revascularization Koroner revaskülarizasyon sonrası kardiyak rehabilitasyonun psikolojik etkileri. Turk Kardiyol Dern Ars. 2016;44(3):228–36. [PubMed] DOI: 10.5543/tkda.2015.56846
- Niebauer J. Treatment after coronary artery bypass surgery remains incomplete without rehabilitation. Circulation. 2016 Jun;133(24):2529–37. [PubMed] DOI: 10.1161/CIRCULATIONAHA.116.021348
- Balady GJ, Arena R, Sietsema K, Myers J, Coke L, Fletcher GF, et al. Clinician’s guide to cardiopulmonary exercise testing in adults: A scientific statement from the American heart association. Circulation. 2010 Jul 13;122(2):191-225. [PubMed] DOI: 10.1161/CIR.0b013e3181e52e69
- Priscila A, Kondo NN, Guillermo M, Gomes PR, Silva PF da. Physical Training Programs After Coronary Artery Bypass Grafting. In: Aronow WS, editor. Coronary Artery Bypass Graft Surgery [Internet]. InTech; 2017 [cited 2020 Aug 25]. DOI: 10.5772/intechopen.71978
- McArdle A, Vasilaki A, Jackson M. Exercise and skeletal muscle ageing: Cellular and molecular mechanisms. Ageing Res Rev. 2002 Feb;1(1):79-93. [PubMed] DOI: 10.1016/s0047-6374(01)00368-2
- Aguillar Cortez A, Ferraz A, Cláudio Lucas da Nóbrega A, Fernando Brunetto A, Haddad Herdy A, Alberto Cordeiro Hossri C, et al. Cardiopulmonary and metabolic rehabilitation guidelines: practical aspects and responsibilities. Arq Bras Cardiol. 2006;86(1). DOI: 10.1590/S0066-782X2006000100011
- da Costa Torres D, dos Santos PMR, Reis HJL, Paisani DM, Chiavegato LD. Effectiveness of an early mobilization program on functional capacity after coronary artery bypass surgery: A randomized controlled trial protocol. SAGE Open Med. 2016 Dec 14;4:2050312116682256. [PubMed] DOI: 10.1177/2050312116682256
- Moholdt TT, Amundsen BH, Rustad LA, Wahba A, Løvø KT, Gullikstad LR, et al. Aerobic interval training versus continuous moderate exercise after coronary artery bypass surgery: A randomized study of cardiovascular effects and quality of life. Am Heart J. 2009;Dec;158(6):1031–7. [PubMed] DOI: 10.1016/j.ahj.2009.10.003
- Meyer K, Lehmann M, Sünder G, Keul J, Weidemann H. Interval versus continuous exercise training after coronary bypass surgery: A comparison of training‐induced acute reactions with respect to the effectiveness of the exercise methods. Clin Cardiol. 1990;13(12):851–61. [PubMed] DOI: 10.1002/clc.4960131208
- Wisløff U, Støylen A, Loennechen JP, Bruvold M, Rognmo Ø, Haram PM, et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: A randomized study. Circulation. 2007 Jun;115(24):3086–94. [PubMed] DOI: 10.1161/CIRCULATIONAHA.106.675041
- Kolmos M, Krawcyk RS, Kruuse C. Effect of high-intensity training on endothelial function in patients with cardiovascular and cerebrovascular disease: A systematic review. SAGE Open Med. 2016 Jan;4:205031211668225. [PubMed] DOI: 10.1177/2050312116682253