Muhammad Fuad Bangash, MD, FCCP
Medical Director, ICU Chief, Pulmonology, Critical Care and Sleep Medicine Steward Healthcare, Norwood Hospital, Norwood, 02062 (USA)
Correspondence: Muhammad Fuad Bangash, MD, FCCP
Medical Director, ICU Chief, Pulmonology, Critical Care and Sleep Medicine Steward Healthcare, Norwood Hospital, 800 Washington Av, Norwood, 02062 (USA)
Cell: 857-329-2397, E-mail: MuhammadFuad.Bangash@steward.org
Received – 6 March 2020, Reviewed & Accepted – 9 March 2020
ABSTRACT
We present a case of COVID-19 patient, who had multiple comorbidities, including diabetes mellitus, bronchial asthma, morbid obesity (BMI:48) and obstructive sleep apnea. She had good compliance with CPAP treatment. After a vacation, she developed typical symptoms of COVID-19, including fever, cough with blood tinged sputum and shortness of breath. She had to be treated with polypharmacy for all of her concurrent diseases. Her hypoxia responded well to oxygen therapy. Laboratory reports and chest x-rays presented a typical picture of COVID-19, including lymphopenia and lung infiltrates. Patient received inj. ceftriaxone, inj. azithromycin and hydroxychloroquine, to which her response was quite satisfactory and after two weeks, she was discharged and shifted to home.
Key words: COVID-19; comorbidities; Hypoxia; Lymphopenia; Hypoxia; Acute lung injury; Azithromycin; Hydroxychloroquine
Citation: Bangash MF. COVID-19 pandemic: An intensivist’s perspective. Anaesth. pain intensive care 2019;24(2):230-233
DOI: https://doi.org/10.35975/apic.v24i2.1263
INTRODUCTION
COVID-19 is perhaps the most versatile disease which the human race has ever come across. Right from the day a patient is diagnosed to be suffering from this viral disease, the treating physicians remain perplexed about the course of the disease, and regarding the best-fit management of this menace. The risk factors identified to be associated with increased mortality in COVID-19 patients, have been age over 50 y, history of diabetes mellitus, hypertension, cardiovascular disease, morbid obesity, immunocompromise and male gender.1,2,3 The patients needing mechanical ventilation were also found to higher mortality than the non-ventilated ones.3
Our patient was unique, as other than being a female, he had had multiple risk factors for increased morbidity and mortality. She had a short course of moderate to severe disease, was put on ventilator and ultimately recovered to be discharged within two weeks.
CASE REPORT
Patient 1: A® 47-year-old female patient with past medical history of type 2 diabetes mellitus, asthma, morbid obesity (BMI 48) and obstructive sleep apnea with good compliance with CPAP treatment, presented to a Community Hospital in Massachusetts on March 23, 2020. Patient had arrived from a vacation in Florida and had symptoms of fever (101○ F), cough with blood tinged sputum and shortness of breath of 1 week duration. She was brought to Emergency Department in ambulance and her pulse oxygen saturation (SpO2) was 82% on room air which improved to 95% on 5 L/min oxygen via nasal cannula.
Home medications: The patient had been taking multiple drugs for her comorbid diseases; e.g., aspirin 81 mg PO OD, atorvastatin calcium 80 mg PO, clopidogrel [Plavix®] 75 mg PO OD, fluticasone/salmeterol 250/50 [Advair 250/50 Diskus®] BID, losartan potassium 25 mg PO OD, metoprolol succinate 12.5 mg PO OD, montelukast sodium [Singulair] 10 mg PO DAILY, trazodone 50 mg PO QPM, glipizide [Glipizide®] 10 mg PO OD, metformin [Glucophage®] 500 mg PO BID, sitagliptin [Januvia®] 1 tab PO OD.
Physical examination: Physical examination findings showed a normal cardiac exam and no wheezes or crackles on lung auscultation.
Lab Data: Laboratory investigations showed a WBC count of 8700 / µL with lymphopenia (absolute lymphocyte count: 900), serum creatinine was normal. Serum ferritin was elevated 893 ng/ml (normal 11-306 ng/ml), LDH 645 u/L (normal 119-251 u/L), CRP 21.5 mg/dL (normal < 0.5 mg/dL) and procalcitonin 0.15 ng/mL (normal ≤ 0.1 ng/mL) and coronavirus PCR positive.
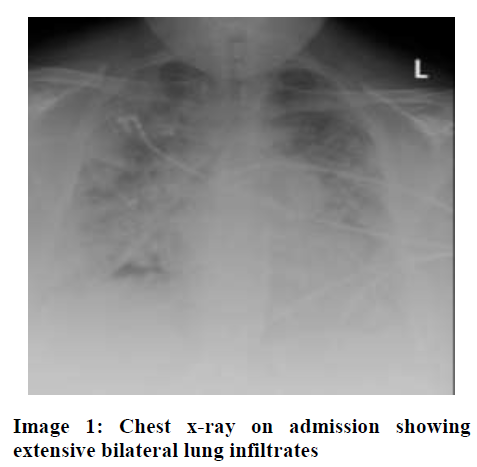
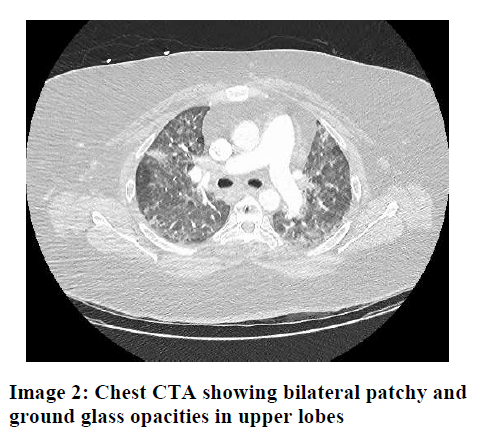
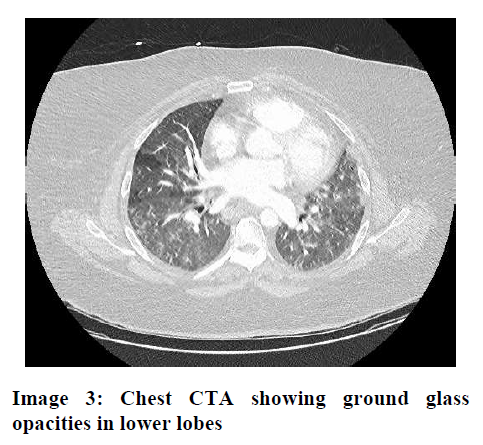
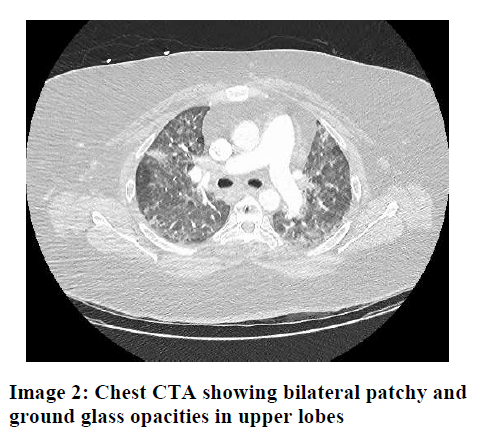
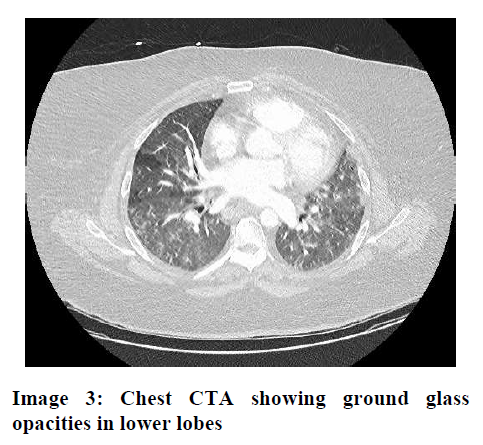
Radiologic Data: Chest x-ray showed extensive bilateral lung infiltrates (Image 1), and computed tomography angiography (CTA) showed chest bilateral patchy and ground glass opacities in the upper and lower lobes of both lungs (Images 2 and 3).
Hospital Course: Patient received ceftriaxone and azithromycin IV and was admitted to medical floor and placed in isolation with mask/gown precautions. Critical Care Service was consulted on hospitalization day 2 due to increasing oxygen requirements to 7 L/min. Patient was transferred to ICU for close monitoring in a negative airflow room with airborne precautions for nursing staff. Hydroxychloroquine was prescribed at a dose of 400 mg BID orally on Day 1 and 200 mg BID on Day 2-5. Chest x-ray and computed tomography angiography (CTA) chest images are as below. Patient’s oxygenation requirements stabilized and she was transferred out of ICU and eventually discharged home on April 6, 2020
DISCUSSION
COVID-19 pandemic started in Wuhan, China in December 2019, and spread like fire throughout the world over the next 3 months. Although eastern
states of USA reported only a few cases in January and February, there was an exponential increase in new cases during the month of March. As a critical care physician, this patient who has been reported above was one of my first patients in a community hospital in Massachusetts.
The epidemiological characteristics of the patients of COVID-19 have been well documented by Wu et al. in a recent paper in JAMA.2 There is extensive literature from China available online to guide the proper diagnosis and treatment of patients with COVID-19 (http://www.chinacdc.cn/en/COVID19/).3
SARS novel coronavirus is a highly infectious agent with 95% similarity to SARS and MERS viruses. With its origins in a wet market in Wuhan, it spread across China and eventually travelled to all parts of the world including Massachusetts.
Although elderly and those with chronic medical problems like diabetes, asthma, COPD and immunocompromised patients are at higher risk of being critically ill, young and middle-aged patients are no exception and can also be severely affected. In my brief period of taking care of patients over the past month, I have seen a 30-yr-old male previously healthy pizza delivery man, who required mechanical ventilation and responded to IV Tocilizumab. I also have taken care of a 61-year-old male patient with no past medical history presenting with respiratory failure and pancytopenia.4,5
Most protocols for management note that patients have either a low WBC count or lymphopenia. An absolute neutrophil-lymphocyte ration of greater than 3.13 is a marker of severe illness. Marked leukocytosis can also be seen. High ferritin, LDH, D-Dimer, CRP and prolactin are noted in these patients.4,5 Patients can range from asymptomatic to mildly symptomatic to rapidly progressive hypoxic respiratory failure as noted in numerous case series from China.
Clinical management includes usual care with admission to hospital into isolation units with supplemental O2. Approximately 5-10% of patients will require ICU care including mechanical ventilation. The mortality is very high 60-80% for patients who require mechanical ventilation. In my opinion, standard management of these patients can improve outcomes but it is more a question of resources available due to surge of patients. For example Italy, Spain and New York had a terrible surge so even with best healthcare systems many patients died to lack of availability of standard ICU care. In contrast, in Massachusetts we have more than 10,000 cases but most hospitals are able to provide ICU care and are not overwhelmed.
Specific treatment plans include the now well-known but yet unproven combo of hydroxychloroquine, azithromycin and atorvastatin with variable success. Specific antivirals include remdesivir used in China and USA, favipinavir in Japan and lately tocilizumab in USA. There are ongoing clinical trials of each of these agents and data will be available in next few weeks.
There are anecdotal reports of microthrombosis in the pulmonary circulation, which is very much possible given the high D-dimer noted in COVID-19 patients. This could lead to pulmonary hypertension and right sided heart failure. So strategies of anti-coagulation and use of epoprostenol in those with refractory respiratory failure are being looked at in tertiary care hospitals.
Several of my cardiology colleagues have noted elevated troponins, myocarditis, cardiogenic shock in COVID 19 patients. A few case reports of STEMI, with no thrombosis seen during cardiac catheterization, have also been reported. Thrombolytics are being used more often then our previous practice of primary PCI. In our patient we used triple drug regimen with good results, including inj. ceftriaxone, inj. azithromycin and hydroxychloroquine.
It is very important to discuss the social and humanitarian aspects of COVID-19 pandemic. As China showed the whole world, strict isolation of patients and contacts is the only measure that can stop the rapid spread. This is hard to do and especially hard on children and elderly, but unfortunately we have no choice but to practice social distancing and quarantine as much as possible as once you are one of the almost 20% of critically ill patients, things can get worse rapidly.
Patients with COVID-19 are isolated! How hard it must be to suffer from a novel life-threatening illness and not be able to be taken care of like a usual patient. Families are restricted from visitation and even if they visit are covered in PPE and are fearful for their own lives. Healthcare providers are busy and also covered in PPE, so my heart goes out each patient and what they are going through along with their families who have to watch them from afar.
But, like every storm, there are silver linings too. I have discovered a newfound passion of taking care of my patients even more so than before. I know it can be overwhelming for many of us, but just take one patient at a time and help them as you can. We may focus on heroic measures like intubation techniques and latest vent protocols, but we must not overlook the human being in front of you. A kind look, a soft touch and a soft spoken “I am here for you” will go a long way.
In conclusion, it is the honest dedication to the profession and a well-coordinated teamwork, which will benefit our patients. The healthcare team…the nurse who is in PPE for 12 h straight, the RT who is doing vent checks round the clock, the unit secretary who is taking so many calls from patient families, and the housekeeping staff, who are cleaning more thoroughly and do huge loads of work with a smiling face, in addition to the physician in-charge, all play equal part in the triumphs and the failures in an ICU.
Conflict of interest: None declared by the author
Author’s contribution: The author was the solely responsible for writing this case report and literature search.
REFERENCES
[Free full text] DOI: https://doi.org/10.35975/apic.v24i1.1216
Medical Director, ICU Chief, Pulmonology, Critical Care and Sleep Medicine Steward Healthcare, Norwood Hospital, Norwood, 02062 (USA)
Correspondence: Muhammad Fuad Bangash, MD, FCCP
Medical Director, ICU Chief, Pulmonology, Critical Care and Sleep Medicine Steward Healthcare, Norwood Hospital, 800 Washington Av, Norwood, 02062 (USA)
Cell: 857-329-2397, E-mail: MuhammadFuad.Bangash@steward.org
Received – 6 March 2020, Reviewed & Accepted – 9 March 2020
ABSTRACT
We present a case of COVID-19 patient, who had multiple comorbidities, including diabetes mellitus, bronchial asthma, morbid obesity (BMI:48) and obstructive sleep apnea. She had good compliance with CPAP treatment. After a vacation, she developed typical symptoms of COVID-19, including fever, cough with blood tinged sputum and shortness of breath. She had to be treated with polypharmacy for all of her concurrent diseases. Her hypoxia responded well to oxygen therapy. Laboratory reports and chest x-rays presented a typical picture of COVID-19, including lymphopenia and lung infiltrates. Patient received inj. ceftriaxone, inj. azithromycin and hydroxychloroquine, to which her response was quite satisfactory and after two weeks, she was discharged and shifted to home.
Key words: COVID-19; comorbidities; Hypoxia; Lymphopenia; Hypoxia; Acute lung injury; Azithromycin; Hydroxychloroquine
Citation: Bangash MF. COVID-19 pandemic: An intensivist’s perspective. Anaesth. pain intensive care 2019;24(2):230-233
DOI: https://doi.org/10.35975/apic.v24i2.1263
INTRODUCTION
COVID-19 is perhaps the most versatile disease which the human race has ever come across. Right from the day a patient is diagnosed to be suffering from this viral disease, the treating physicians remain perplexed about the course of the disease, and regarding the best-fit management of this menace. The risk factors identified to be associated with increased mortality in COVID-19 patients, have been age over 50 y, history of diabetes mellitus, hypertension, cardiovascular disease, morbid obesity, immunocompromise and male gender.1,2,3 The patients needing mechanical ventilation were also found to higher mortality than the non-ventilated ones.3
Our patient was unique, as other than being a female, he had had multiple risk factors for increased morbidity and mortality. She had a short course of moderate to severe disease, was put on ventilator and ultimately recovered to be discharged within two weeks.
CASE REPORT
Patient 1: A® 47-year-old female patient with past medical history of type 2 diabetes mellitus, asthma, morbid obesity (BMI 48) and obstructive sleep apnea with good compliance with CPAP treatment, presented to a Community Hospital in Massachusetts on March 23, 2020. Patient had arrived from a vacation in Florida and had symptoms of fever (101○ F), cough with blood tinged sputum and shortness of breath of 1 week duration. She was brought to Emergency Department in ambulance and her pulse oxygen saturation (SpO2) was 82% on room air which improved to 95% on 5 L/min oxygen via nasal cannula.
Home medications: The patient had been taking multiple drugs for her comorbid diseases; e.g., aspirin 81 mg PO OD, atorvastatin calcium 80 mg PO, clopidogrel [Plavix®] 75 mg PO OD, fluticasone/salmeterol 250/50 [Advair 250/50 Diskus®] BID, losartan potassium 25 mg PO OD, metoprolol succinate 12.5 mg PO OD, montelukast sodium [Singulair] 10 mg PO DAILY, trazodone 50 mg PO QPM, glipizide [Glipizide®] 10 mg PO OD, metformin [Glucophage®] 500 mg PO BID, sitagliptin [Januvia®] 1 tab PO OD.
Physical examination: Physical examination findings showed a normal cardiac exam and no wheezes or crackles on lung auscultation.
Lab Data: Laboratory investigations showed a WBC count of 8700 / µL with lymphopenia (absolute lymphocyte count: 900), serum creatinine was normal. Serum ferritin was elevated 893 ng/ml (normal 11-306 ng/ml), LDH 645 u/L (normal 119-251 u/L), CRP 21.5 mg/dL (normal < 0.5 mg/dL) and procalcitonin 0.15 ng/mL (normal ≤ 0.1 ng/mL) and coronavirus PCR positive.
Radiologic Data: Chest x-ray showed extensive bilateral lung infiltrates (Image 1), and computed tomography angiography (CTA) showed chest bilateral patchy and ground glass opacities in the upper and lower lobes of both lungs (Images 2 and 3).
Hospital Course: Patient received ceftriaxone and azithromycin IV and was admitted to medical floor and placed in isolation with mask/gown precautions. Critical Care Service was consulted on hospitalization day 2 due to increasing oxygen requirements to 7 L/min. Patient was transferred to ICU for close monitoring in a negative airflow room with airborne precautions for nursing staff. Hydroxychloroquine was prescribed at a dose of 400 mg BID orally on Day 1 and 200 mg BID on Day 2-5. Chest x-ray and computed tomography angiography (CTA) chest images are as below. Patient’s oxygenation requirements stabilized and she was transferred out of ICU and eventually discharged home on April 6, 2020
DISCUSSION
COVID-19 pandemic started in Wuhan, China in December 2019, and spread like fire throughout the world over the next 3 months. Although eastern
states of USA reported only a few cases in January and February, there was an exponential increase in new cases during the month of March. As a critical care physician, this patient who has been reported above was one of my first patients in a community hospital in Massachusetts.
The epidemiological characteristics of the patients of COVID-19 have been well documented by Wu et al. in a recent paper in JAMA.2 There is extensive literature from China available online to guide the proper diagnosis and treatment of patients with COVID-19 (http://www.chinacdc.cn/en/COVID19/).3
SARS novel coronavirus is a highly infectious agent with 95% similarity to SARS and MERS viruses. With its origins in a wet market in Wuhan, it spread across China and eventually travelled to all parts of the world including Massachusetts.
Although elderly and those with chronic medical problems like diabetes, asthma, COPD and immunocompromised patients are at higher risk of being critically ill, young and middle-aged patients are no exception and can also be severely affected. In my brief period of taking care of patients over the past month, I have seen a 30-yr-old male previously healthy pizza delivery man, who required mechanical ventilation and responded to IV Tocilizumab. I also have taken care of a 61-year-old male patient with no past medical history presenting with respiratory failure and pancytopenia.4,5
Most protocols for management note that patients have either a low WBC count or lymphopenia. An absolute neutrophil-lymphocyte ration of greater than 3.13 is a marker of severe illness. Marked leukocytosis can also be seen. High ferritin, LDH, D-Dimer, CRP and prolactin are noted in these patients.4,5 Patients can range from asymptomatic to mildly symptomatic to rapidly progressive hypoxic respiratory failure as noted in numerous case series from China.
Clinical management includes usual care with admission to hospital into isolation units with supplemental O2. Approximately 5-10% of patients will require ICU care including mechanical ventilation. The mortality is very high 60-80% for patients who require mechanical ventilation. In my opinion, standard management of these patients can improve outcomes but it is more a question of resources available due to surge of patients. For example Italy, Spain and New York had a terrible surge so even with best healthcare systems many patients died to lack of availability of standard ICU care. In contrast, in Massachusetts we have more than 10,000 cases but most hospitals are able to provide ICU care and are not overwhelmed.
Specific treatment plans include the now well-known but yet unproven combo of hydroxychloroquine, azithromycin and atorvastatin with variable success. Specific antivirals include remdesivir used in China and USA, favipinavir in Japan and lately tocilizumab in USA. There are ongoing clinical trials of each of these agents and data will be available in next few weeks.
There are anecdotal reports of microthrombosis in the pulmonary circulation, which is very much possible given the high D-dimer noted in COVID-19 patients. This could lead to pulmonary hypertension and right sided heart failure. So strategies of anti-coagulation and use of epoprostenol in those with refractory respiratory failure are being looked at in tertiary care hospitals.
Several of my cardiology colleagues have noted elevated troponins, myocarditis, cardiogenic shock in COVID 19 patients. A few case reports of STEMI, with no thrombosis seen during cardiac catheterization, have also been reported. Thrombolytics are being used more often then our previous practice of primary PCI. In our patient we used triple drug regimen with good results, including inj. ceftriaxone, inj. azithromycin and hydroxychloroquine.
It is very important to discuss the social and humanitarian aspects of COVID-19 pandemic. As China showed the whole world, strict isolation of patients and contacts is the only measure that can stop the rapid spread. This is hard to do and especially hard on children and elderly, but unfortunately we have no choice but to practice social distancing and quarantine as much as possible as once you are one of the almost 20% of critically ill patients, things can get worse rapidly.
Patients with COVID-19 are isolated! How hard it must be to suffer from a novel life-threatening illness and not be able to be taken care of like a usual patient. Families are restricted from visitation and even if they visit are covered in PPE and are fearful for their own lives. Healthcare providers are busy and also covered in PPE, so my heart goes out each patient and what they are going through along with their families who have to watch them from afar.
But, like every storm, there are silver linings too. I have discovered a newfound passion of taking care of my patients even more so than before. I know it can be overwhelming for many of us, but just take one patient at a time and help them as you can. We may focus on heroic measures like intubation techniques and latest vent protocols, but we must not overlook the human being in front of you. A kind look, a soft touch and a soft spoken “I am here for you” will go a long way.
In conclusion, it is the honest dedication to the profession and a well-coordinated teamwork, which will benefit our patients. The healthcare team…the nurse who is in PPE for 12 h straight, the RT who is doing vent checks round the clock, the unit secretary who is taking so many calls from patient families, and the housekeeping staff, who are cleaning more thoroughly and do huge loads of work with a smiling face, in addition to the physician in-charge, all play equal part in the triumphs and the failures in an ICU.
Conflict of interest: None declared by the author
Author’s contribution: The author was the solely responsible for writing this case report and literature search.
REFERENCES
- Bashir MA, Durrani RS. Novel coronavirus (COVID-19): Its implications for anesthesia. Anaesth. pain intensive care 2020;24(1):1-3 [Free full text] DOI: https://doi.org/10.35975/apic.v24i1.1214
- Wu Z, McGoogan JM. JAMA. Published online February 24, 2020. doi:10.1001/jama.2020.2648
- Chinese Center for Disease Control and Prevention. COVID19. Available on http://www.chinacdc.cn/en/COVID19/ . (Accessed on23 March 2020)
- Majeed A, Shajar MA. Is hemoglobin the missing link in the
[Free full text] DOI: https://doi.org/10.35975/apic.v24i1.1216
- Liu J, Liu Y, Xiang P, Pu L, Xiong H, Li C, et al. Neutrophil-to-Lymphocyte Ratio Predicts Severe Illness Patients with 2019 Novel Coronavirus in the Early Stage. Available on preprint data website dhttps://www.medrxiv.org/content/10.1101/2020.02.10.20021584v1 (Accessed on 20 March 2020)