Gauhar Afshan1, Ali Sarfraz Siddiqui2
1Professor; 2Assistant Professor,
Department of Anesthesiology, Aga Khan University, Karachi, (Pakistan)
Correspondence: Professor Gauhar Afshan, Department of Anesthesiology, Aga Khan University, Stadium Road, Karachi, Karachi City, Sindh 74800 (Pakistan); Phone: +92 2134864635;
E-mail: gauhar.afshan@aku.edu
ABSTRACT
We attempted to review the published literature to find out the status of pain assessment in critically ill patients (CIPs) managing in ICUs of low resource countries. We used broad electronic database (2004-2018) from common search engines. Evidence showed that 33%-61% of the patients in ICU experienced pain at rest and among them 10%-33% of patients experienced moderate to severe pain in developed countries. Prevalence of pain is expected to be high in low resource countries due to huge disease burden of CIPs.
The gold standard of pain assessment is self-reporting; however, this is not possible when patients in ICU are unable to communicate. Alternatively, Behavioral Pain Scale (BPS) and Critical Care Pain Observation Tool (CPOT) can be used in this population. These methods/tools are being used in developed countries, however, no evidence is available in low resource countries. The dynamic nature of pain in ICU patients justifies regular pain assessment in all ICU settings. Authors strongly recommend that pain should be objectively assessed in all ICU patients regardless of age and gender using reliable and validated tools like BPS or CPOT.
Key words: Pain; Pain assessment; Critically ill; Critical Care Pain Observation Tool; Behavioral Pain Scale; Low resource; Intensive Care; ICU
Citation: Afshan G, Siddiqui S. Pain assessment in critically ill patients in low resource countries. Anaesth Pain & Intensive Care 2018;22 Suppl 1:S83─S87
Received: 26 Oct 2018, Reviewed & Accepted: 3 Nov 2018
INTRODUCTION
Access to critical care is very crucial in low resource countries due to lack of infrastructure and trained healthcare providers. There has been huge burden of critical illness in low resource countries and unfortunately 50% of these countries lack any published data on health care provision for critically ill patients (CIPs) in Intensive Care Units (ICU) .1
Pain assessment in CIPs has been neglected across the world. This is mainly due to the fact that CIPs are unable to express or report their pain. We know unrelieved pain may evoke a cascade of stress related response e.g. tachycardia, hypertension, increased myocardial oxygen consumption, hypercoagulability, immune-suppression, and persistent catabolism resulting in long stay in ICU.2 Current published data shows that pre-existing and underlying chronic diseases, associated wounds and drains, presence of an endotracheal tube, routine nursing procedures e.g. patient’s positioning and airway suctioning are the common causes of pain in CIPs regardless of their indication of ICU admission.2
Recently pain assessment in CIPs has been globally recognized. The gold standard in pain assessment is patient’s self-reporting which is often not possible in CIPs. It has been suggested that the severity of pain is underestimated in ICU patients particularly those who are sedated or unable to communicate or self-report.3 Current data shows that “Behavioral Pain Scale (BPS)” and the “Critical Care Pain Observation Tool (CPOT)” are reliable and validated best available objective assessment tools for those who are unable to self-report pain in intensive care units .4
There is a general perception that patients are not being assessed for pain in ICUs of low resource countries. In addition, the capacity to provide pain assessment in ICUs in low resource countries is also not known. Our objectives were to review the published literature to find out the current status of assessing pain in ICUs of low resource countries and to know the most suitable pain assessment method (cost effective) in these countries considering the existing infrastructure and lack of health care providers.
SEARCH METHODOLOGY
We used broad electronic database (2004-2018) through search engines of Pub Med, Google Chrome, Cochrane, EMBASE, UpToDate and MD Consult with no language restrictions. Eight key words /terms were used to capture all relevant studies considering the overall objectives of the review.
With consensus of both authors, we included studies of any design catering adult critical ill patients managing in ICU and provided relevant information to answer our objectives. Reviews were also included when they provided recent and relevant data. We excluded studies catering patients in pediatric and neonatal age group.
PREVALENCE OF PAIN IN CIPS
Patients in ICU often experience moderate-to-severe pain at rest and during care related procedures, however those who are unable to self- report have a higher risk of underestimated pain. Currently very limited literature focuses on pain prevalence in critical care ill patients managing in ICUs. However no evidence is available about the prevalence studies in low resource countries.
A recent study of developed world suggests that around 33% of the patients in ICU experienced pain at rest and approximately 10% of them experienced moderate to severe pain .6 However an earlier study reported that 61% of patients experienced pain at rest while 33% experienced moderate to severe pain. 7There is no significant correlation of severity of pain with gender and age, however a recent study suggests that young patients experience more pain than geriatric group 8,9.
Generally patients in ICU require sedation as they experience anxiety and agitation due to their critical illness and care-related procedures. It has been shown that patients with lower sedation score are predicted to have higher levels of pain at rest and care related procedures than patients who are asleep.7
As no specific data is available for low resource countries so we extrapolated the prevalence rate (based on the data of published literature of developed countries) is 60% or more considering the increase disease burden (trauma, sepsis and cancer etc.) and poor infrastructure and lack of health care professional in critical care areas.
CAUSES OF PAIN IN CIPS
Pain, the most traumatic memorable experience in ICU patients, is subjective in nature and multifactorial. It is commonly experienced at rest and during care- related procedures e.g. change in position, suction of oral cavity and bronchial tree, wound care, removal of drain, insertion of catheters, intravenous accesses, intubation and other therapeutic or mini-surgical interventions. It can further be divided into four categories 10
There is a general consensus that pain is “complex” in CIPs due to the involvement of multiple organs / systems. Unrelieved pain increases the concentrations of catecholamine, which led to vasoconstriction, impaired tissue perfusion and decreased partial pressure of oxygen in the tissues resulting in distressing experience of pain.
Hyper metabolism in CIPs causes hyper glycaemia, lipolysis or protein catabolism resulting in impaired wound healing and increases risk of infections. This is one of the reasons of pain experienced in ICU. Un-relieved pain also causes immune system disorders by inhibiting the NK cell activity and decreasing cytotoxic T-lymphocyte count resulting in persistent pain.11 Causes of pain in ICU of low resource countries are similar to the existing published data of developed countries considering the patho-physiology and patients demographics of critical ill patients.
NEED OF PAIN ASSESSMENT IN ICU
Recent evidence shows that lack of appropriate management (assessment and treatment) of pain in CIPs is associated with negative patient outcomes e.g. longer duration of mechanical ventilation and length of stay in ICU and increased morbidity and mortality.10
Patients, who are sedated and intubated in ICU, are unable to self-report the pain (verbally or by pointing at visual analogue pain scales). Physiological indicators like heart rate and blood pressure may increase with pain in such patients. However, these cardiovascular changes can occur for reasons other than pain, especially in CIPs requiring ICU care. There is no strong evidence to support the use of physiological indicators in isolation to assess pain and this can be considered in ICU patients of low resource countries.12
American Society for Pain Management Nursing (ASPMN) proposed a 4-step approach for the assessment of pain as follows11
Behavioral Pain Assessment Tools
A long list of behavioral pain assessment tools has been used in ICUs of developed countries. These are Behavioral Pain Scale-non-intubated (BPS-NI), Critical Care Pain Observation Tool (CPOT), Non-verbal Pain Scale (NVPS), Pain Behavioral Assessment Tool (PBAT) and Pain assessment, Intervention, and Notation (PAIN) algorithm. However the most recent evidence shows that Behavioral Pain Scale (BPS) and Critical Care Pain Observation Tool (CPOT) are the most reliable and the best validated scales in patients who are unable to self-report their pain11. In contrast to the developed countries data, no evidence is available about using any pain assessment tools in low resource countries.
It is also evident that Behavioral Pain Scales have some limitations in specific group of population in ICU e.g. patients with brain injury, burns, delirium and a cognitive deficit. In addition these scales cannot discriminate severity of pain i.e. mild, moderate and severe. These assessment tools are not recommended in patients with spinal injuries and those receiving neuromuscular blocking agents.12
Behavioral Pain Scale (BPS)
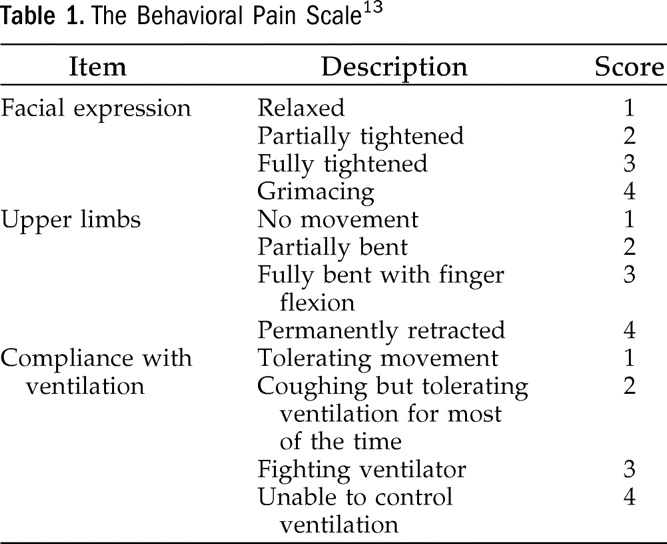
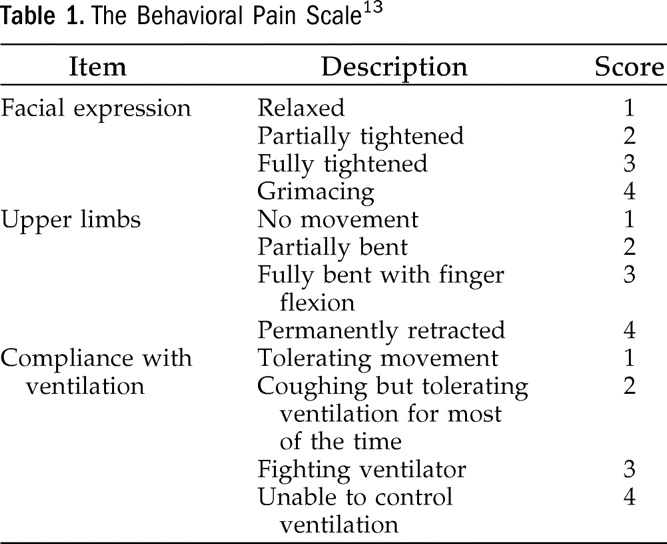
The Behavioral Pain Scale (BPS), introduced in 2001, is the most widely used pain assessment tool for unconscious and mechanically ventilated patients in developed world. It is based on three types of behaviors i.e. facial expressions, upper limb movements and compliance with ventilator. In facial expression domain, assessment will be described and scored as relaxed, partially tightened (brow lowering), fully tightened (eyelid closing) and grimacing. As shown in Table 1, each patient’s behavior score is from 1 to 4 and total score varies from 3 (no pain) to 12 (maximum pain). There is strong evidence to support the reliability and validity of the BPS as this tool has been tested in a variety of ICU settings.12 Considering the resources required to do BPS, we believe that it can easily be done by the bed side nurses of ICU in low resource countries.
Table 1: Behavioral Pain Scale
Critical Care Pain Observation Tool (CPOT)
CPOT was introduced in 2006 and developed earlier in French language only. Later it was translated into other languages including commonly used English. The tool was designed to detect pain in CIPs and includes four behavioral categories i.e. facial expressions, body movements, muscle tension and compliance with ventilator (for intubated patients) or verbalization (for un-intubated patients), as shown in Table 2.
Table 2: The Critical Pain Observation Tool (CPOT)
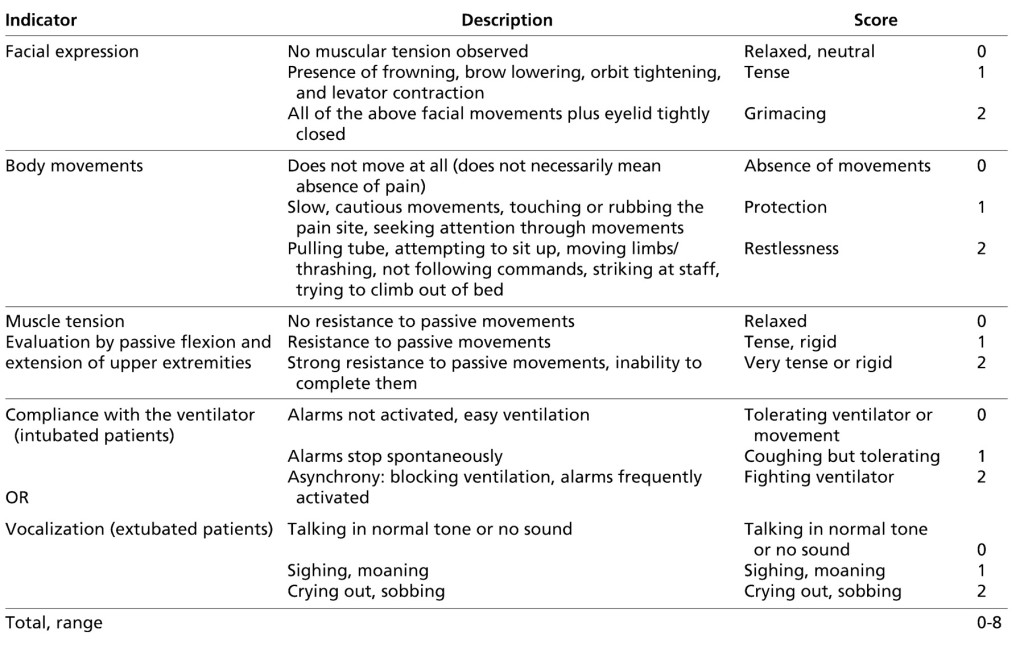
(Source: Gélinas C, Fillion L, Puntillo KA, Viens C, Martine Fortier M. Validation of the Critical-Care Pain Observation Tool in Adult PatientsAm J Crit Care July 2006 15:420-427)
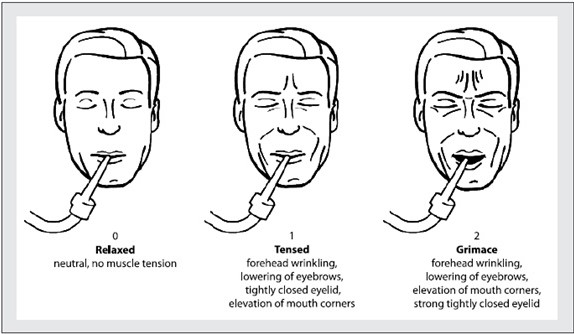
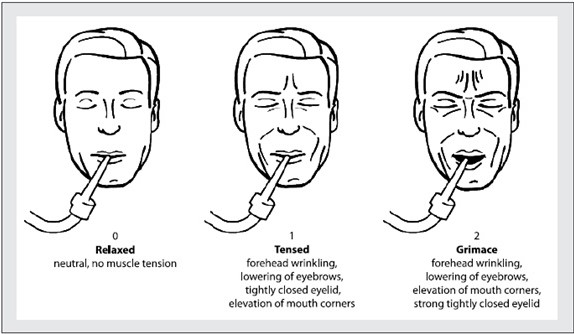
Each patient’s behavior scores from 0 to 2 and total score varies from 0 (no pain) to 8 (maximum pain). Facial expression and scoring using CPOT is shown in Figure 1. The CPOT has shown good reliability and validity in all aspects in recent evidence. 13 This can be implemented in ICU of low resource countries after appropriate training of staff without any extra cost required.
Figure 1: Facial Expression in Critical Care Pain Observation Tool
OUTCOME OF PAIN ASSESSMENT IN ICU
It has been proven that regular assessment of pain intensity improves pain management, quality of life of patients in ICU and after discharge from ICU. A recent systematic review described positive impact of pain assessment on CIPs’ outcomes, including duration of mechanical ventilation, ICU length of stay, adverse events and mortality.14 This indicates that pain assessment may increase the overall outcome of the patients resulting in less health care burden in low resource countries.
NURSING STAFF TRAINING AND PRACTICE CHANGE
Nurses are the first responders and regularly involved in ICU patients. They face numerous challenges in assessing pain in patients who are unable to self-report due to altered level of consciousness (LOC), sedation and mechanical ventilation. In addition some neurological and mental disorders e.g. aphasia, dementia, delirium and psychoses made the process complex. Lack of a systematic and standardized method for assessing pain prevents the comparison of pain scores and effectiveness of patients’ analgesic regimes. 12
Literature review suggests that pain assessment tools like, BPS or CPOT are applied clinically to measure pain in ICU patients in a systematic and comparable way. Assessment of pain severity allows nurses and other health care professionals to identify patient’s pain severity and administer analgesia accordingly. This would prevent distressing patho-physiological and harmful consequences of un-relieved pain.
CURRENT STATUS & PRACTICE RECOMMENDATIONS
Pain in ICU patients is a silent reality and regular pain assessment is necessary for optimal care and better outcome. As per available published literature; no evidence shows that assessment of pain is routinely done in ICU patients of low resource countries in spite of high prevalence rate of Pain (more than 60%) due to huge disease burden.
Physiological parameters e.g. heart rate, blood pressure, respiratory rate are usually misleading for pain assessment in ICU patients who are unable to self-report .Alternatively objective assessment tools e.g. BPS and CPOT are being successfully used in developed countries and authors recommend that these can be used in ICU setting of low resource countries.
It has been suggested that analgesia must be administered at rest and prior/during care related procedures according to regular pain assessment using BPS or CPOT. Nursing staff and physicians involved in the management of ICU patients need to undergo special training using appropriate pain assessment tool (BPS or CPOT) in their routine practice.
We believe that improvements of health care in low resource countries require a commitment to learn from the research of the same region. Authors strongly feel the urgent need of pain assessment research in CIPs of low resource countries to face the pain assessment challenges in ICU.
Conflict of interest: Nil declared by the authors
Authors’ contribution: Both authors contributed equally in the preparation of this manuscript
REFERENCES
1. Murthy S, Leligdowicz A, Adhikari NK. Intensive Care Unit Capacity in Low-Income Countries: A Systematic Review. PLOS one. 2015 24; 10 (1): e0116949. [PubMed]
1Professor; 2Assistant Professor,
Department of Anesthesiology, Aga Khan University, Karachi, (Pakistan)
Correspondence: Professor Gauhar Afshan, Department of Anesthesiology, Aga Khan University, Stadium Road, Karachi, Karachi City, Sindh 74800 (Pakistan); Phone: +92 2134864635;
E-mail: gauhar.afshan@aku.edu
ABSTRACT
We attempted to review the published literature to find out the status of pain assessment in critically ill patients (CIPs) managing in ICUs of low resource countries. We used broad electronic database (2004-2018) from common search engines. Evidence showed that 33%-61% of the patients in ICU experienced pain at rest and among them 10%-33% of patients experienced moderate to severe pain in developed countries. Prevalence of pain is expected to be high in low resource countries due to huge disease burden of CIPs.
The gold standard of pain assessment is self-reporting; however, this is not possible when patients in ICU are unable to communicate. Alternatively, Behavioral Pain Scale (BPS) and Critical Care Pain Observation Tool (CPOT) can be used in this population. These methods/tools are being used in developed countries, however, no evidence is available in low resource countries. The dynamic nature of pain in ICU patients justifies regular pain assessment in all ICU settings. Authors strongly recommend that pain should be objectively assessed in all ICU patients regardless of age and gender using reliable and validated tools like BPS or CPOT.
Key words: Pain; Pain assessment; Critically ill; Critical Care Pain Observation Tool; Behavioral Pain Scale; Low resource; Intensive Care; ICU
Citation: Afshan G, Siddiqui S. Pain assessment in critically ill patients in low resource countries. Anaesth Pain & Intensive Care 2018;22 Suppl 1:S83─S87
Received: 26 Oct 2018, Reviewed & Accepted: 3 Nov 2018
INTRODUCTION
Access to critical care is very crucial in low resource countries due to lack of infrastructure and trained healthcare providers. There has been huge burden of critical illness in low resource countries and unfortunately 50% of these countries lack any published data on health care provision for critically ill patients (CIPs) in Intensive Care Units (ICU) .1
Pain assessment in CIPs has been neglected across the world. This is mainly due to the fact that CIPs are unable to express or report their pain. We know unrelieved pain may evoke a cascade of stress related response e.g. tachycardia, hypertension, increased myocardial oxygen consumption, hypercoagulability, immune-suppression, and persistent catabolism resulting in long stay in ICU.2 Current published data shows that pre-existing and underlying chronic diseases, associated wounds and drains, presence of an endotracheal tube, routine nursing procedures e.g. patient’s positioning and airway suctioning are the common causes of pain in CIPs regardless of their indication of ICU admission.2
Recently pain assessment in CIPs has been globally recognized. The gold standard in pain assessment is patient’s self-reporting which is often not possible in CIPs. It has been suggested that the severity of pain is underestimated in ICU patients particularly those who are sedated or unable to communicate or self-report.3 Current data shows that “Behavioral Pain Scale (BPS)” and the “Critical Care Pain Observation Tool (CPOT)” are reliable and validated best available objective assessment tools for those who are unable to self-report pain in intensive care units .4
There is a general perception that patients are not being assessed for pain in ICUs of low resource countries. In addition, the capacity to provide pain assessment in ICUs in low resource countries is also not known. Our objectives were to review the published literature to find out the current status of assessing pain in ICUs of low resource countries and to know the most suitable pain assessment method (cost effective) in these countries considering the existing infrastructure and lack of health care providers.
SEARCH METHODOLOGY
We used broad electronic database (2004-2018) through search engines of Pub Med, Google Chrome, Cochrane, EMBASE, UpToDate and MD Consult with no language restrictions. Eight key words /terms were used to capture all relevant studies considering the overall objectives of the review.
With consensus of both authors, we included studies of any design catering adult critical ill patients managing in ICU and provided relevant information to answer our objectives. Reviews were also included when they provided recent and relevant data. We excluded studies catering patients in pediatric and neonatal age group.
PREVALENCE OF PAIN IN CIPS
Patients in ICU often experience moderate-to-severe pain at rest and during care related procedures, however those who are unable to self- report have a higher risk of underestimated pain. Currently very limited literature focuses on pain prevalence in critical care ill patients managing in ICUs. However no evidence is available about the prevalence studies in low resource countries.
A recent study of developed world suggests that around 33% of the patients in ICU experienced pain at rest and approximately 10% of them experienced moderate to severe pain .6 However an earlier study reported that 61% of patients experienced pain at rest while 33% experienced moderate to severe pain. 7There is no significant correlation of severity of pain with gender and age, however a recent study suggests that young patients experience more pain than geriatric group 8,9.
Generally patients in ICU require sedation as they experience anxiety and agitation due to their critical illness and care-related procedures. It has been shown that patients with lower sedation score are predicted to have higher levels of pain at rest and care related procedures than patients who are asleep.7
As no specific data is available for low resource countries so we extrapolated the prevalence rate (based on the data of published literature of developed countries) is 60% or more considering the increase disease burden (trauma, sepsis and cancer etc.) and poor infrastructure and lack of health care professional in critical care areas.
CAUSES OF PAIN IN CIPS
Pain, the most traumatic memorable experience in ICU patients, is subjective in nature and multifactorial. It is commonly experienced at rest and during care- related procedures e.g. change in position, suction of oral cavity and bronchial tree, wound care, removal of drain, insertion of catheters, intravenous accesses, intubation and other therapeutic or mini-surgical interventions. It can further be divided into four categories 10
- Persistent pain associated with invasive procedures
- Acute pain related to an ongoing disease
- Intermittent pain associated with ICU procedures
- Chronic pain occurring before ICU admission
There is a general consensus that pain is “complex” in CIPs due to the involvement of multiple organs / systems. Unrelieved pain increases the concentrations of catecholamine, which led to vasoconstriction, impaired tissue perfusion and decreased partial pressure of oxygen in the tissues resulting in distressing experience of pain.
Hyper metabolism in CIPs causes hyper glycaemia, lipolysis or protein catabolism resulting in impaired wound healing and increases risk of infections. This is one of the reasons of pain experienced in ICU. Un-relieved pain also causes immune system disorders by inhibiting the NK cell activity and decreasing cytotoxic T-lymphocyte count resulting in persistent pain.11 Causes of pain in ICU of low resource countries are similar to the existing published data of developed countries considering the patho-physiology and patients demographics of critical ill patients.
NEED OF PAIN ASSESSMENT IN ICU
Recent evidence shows that lack of appropriate management (assessment and treatment) of pain in CIPs is associated with negative patient outcomes e.g. longer duration of mechanical ventilation and length of stay in ICU and increased morbidity and mortality.10
Patients, who are sedated and intubated in ICU, are unable to self-report the pain (verbally or by pointing at visual analogue pain scales). Physiological indicators like heart rate and blood pressure may increase with pain in such patients. However, these cardiovascular changes can occur for reasons other than pain, especially in CIPs requiring ICU care. There is no strong evidence to support the use of physiological indicators in isolation to assess pain and this can be considered in ICU patients of low resource countries.12
American Society for Pain Management Nursing (ASPMN) proposed a 4-step approach for the assessment of pain as follows11
- Always attempt to obtain the patient’s self-report of pain
- Use a validated behavioral pain scale
- Ask the family or caregiver about the patient’s pain behaviors
- Attempt an analgesic trial when pain is suspected and re-assess pain
Behavioral Pain Assessment Tools
A long list of behavioral pain assessment tools has been used in ICUs of developed countries. These are Behavioral Pain Scale-non-intubated (BPS-NI), Critical Care Pain Observation Tool (CPOT), Non-verbal Pain Scale (NVPS), Pain Behavioral Assessment Tool (PBAT) and Pain assessment, Intervention, and Notation (PAIN) algorithm. However the most recent evidence shows that Behavioral Pain Scale (BPS) and Critical Care Pain Observation Tool (CPOT) are the most reliable and the best validated scales in patients who are unable to self-report their pain11. In contrast to the developed countries data, no evidence is available about using any pain assessment tools in low resource countries.
It is also evident that Behavioral Pain Scales have some limitations in specific group of population in ICU e.g. patients with brain injury, burns, delirium and a cognitive deficit. In addition these scales cannot discriminate severity of pain i.e. mild, moderate and severe. These assessment tools are not recommended in patients with spinal injuries and those receiving neuromuscular blocking agents.12
Behavioral Pain Scale (BPS)
The Behavioral Pain Scale (BPS), introduced in 2001, is the most widely used pain assessment tool for unconscious and mechanically ventilated patients in developed world. It is based on three types of behaviors i.e. facial expressions, upper limb movements and compliance with ventilator. In facial expression domain, assessment will be described and scored as relaxed, partially tightened (brow lowering), fully tightened (eyelid closing) and grimacing. As shown in Table 1, each patient’s behavior score is from 1 to 4 and total score varies from 3 (no pain) to 12 (maximum pain). There is strong evidence to support the reliability and validity of the BPS as this tool has been tested in a variety of ICU settings.12 Considering the resources required to do BPS, we believe that it can easily be done by the bed side nurses of ICU in low resource countries.
Table 1: Behavioral Pain Scale
(Source: The Use of the Behavioral Pain Scale to Assess Pain in Conscious Sedated Patients
Anesthesia & Analgesia110(1):127-133, January 2010.)Critical Care Pain Observation Tool (CPOT)
CPOT was introduced in 2006 and developed earlier in French language only. Later it was translated into other languages including commonly used English. The tool was designed to detect pain in CIPs and includes four behavioral categories i.e. facial expressions, body movements, muscle tension and compliance with ventilator (for intubated patients) or verbalization (for un-intubated patients), as shown in Table 2.
Table 2: The Critical Pain Observation Tool (CPOT)
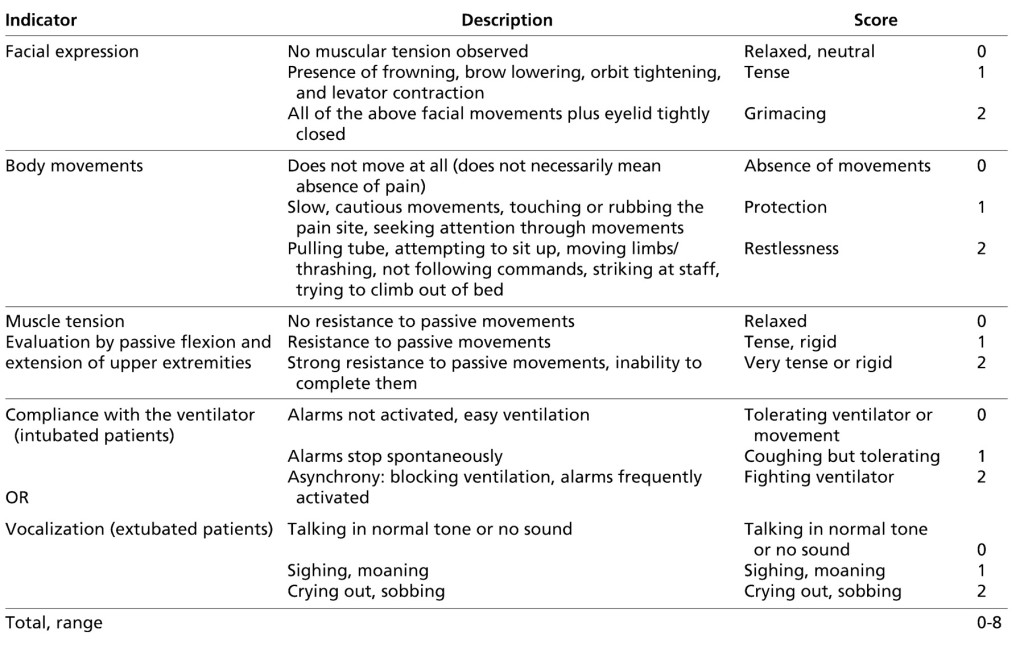
(Source: Gélinas C, Fillion L, Puntillo KA, Viens C, Martine Fortier M. Validation of the Critical-Care Pain Observation Tool in Adult PatientsAm J Crit Care July 2006 15:420-427)
Each patient’s behavior scores from 0 to 2 and total score varies from 0 (no pain) to 8 (maximum pain). Facial expression and scoring using CPOT is shown in Figure 1. The CPOT has shown good reliability and validity in all aspects in recent evidence. 13 This can be implemented in ICU of low resource countries after appropriate training of staff without any extra cost required.
Figure 1: Facial Expression in Critical Care Pain Observation Tool
OUTCOME OF PAIN ASSESSMENT IN ICU
It has been proven that regular assessment of pain intensity improves pain management, quality of life of patients in ICU and after discharge from ICU. A recent systematic review described positive impact of pain assessment on CIPs’ outcomes, including duration of mechanical ventilation, ICU length of stay, adverse events and mortality.14 This indicates that pain assessment may increase the overall outcome of the patients resulting in less health care burden in low resource countries.
NURSING STAFF TRAINING AND PRACTICE CHANGE
Nurses are the first responders and regularly involved in ICU patients. They face numerous challenges in assessing pain in patients who are unable to self-report due to altered level of consciousness (LOC), sedation and mechanical ventilation. In addition some neurological and mental disorders e.g. aphasia, dementia, delirium and psychoses made the process complex. Lack of a systematic and standardized method for assessing pain prevents the comparison of pain scores and effectiveness of patients’ analgesic regimes. 12
Literature review suggests that pain assessment tools like, BPS or CPOT are applied clinically to measure pain in ICU patients in a systematic and comparable way. Assessment of pain severity allows nurses and other health care professionals to identify patient’s pain severity and administer analgesia accordingly. This would prevent distressing patho-physiological and harmful consequences of un-relieved pain.
CURRENT STATUS & PRACTICE RECOMMENDATIONS
Pain in ICU patients is a silent reality and regular pain assessment is necessary for optimal care and better outcome. As per available published literature; no evidence shows that assessment of pain is routinely done in ICU patients of low resource countries in spite of high prevalence rate of Pain (more than 60%) due to huge disease burden.
Physiological parameters e.g. heart rate, blood pressure, respiratory rate are usually misleading for pain assessment in ICU patients who are unable to self-report .Alternatively objective assessment tools e.g. BPS and CPOT are being successfully used in developed countries and authors recommend that these can be used in ICU setting of low resource countries.
It has been suggested that analgesia must be administered at rest and prior/during care related procedures according to regular pain assessment using BPS or CPOT. Nursing staff and physicians involved in the management of ICU patients need to undergo special training using appropriate pain assessment tool (BPS or CPOT) in their routine practice.
We believe that improvements of health care in low resource countries require a commitment to learn from the research of the same region. Authors strongly feel the urgent need of pain assessment research in CIPs of low resource countries to face the pain assessment challenges in ICU.
Conflict of interest: Nil declared by the authors
Authors’ contribution: Both authors contributed equally in the preparation of this manuscript
REFERENCES
1. Murthy S, Leligdowicz A, Adhikari NK. Intensive Care Unit Capacity in Low-Income Countries: A Systematic Review. PLOS one. 2015 24; 10 (1): e0116949. [PubMed]
- Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Am J Health Syst Pharm 2013;70(1):53-8. [PubMed]
- Kotfis K, Zegan-Barańska M, Szydłowski L, Żukowski M, Ely EW.Methods of pain assessment in adult intensive care unit patients — Polish version of the CPOT (Critical Care Pain Observation Tool) and BPS (Behavioral Pain Scale). Anaesthesiol Intensive 2017;49(1):66-72. [Free Full Text]. DOI: 10.5603/AIT.2017.0010
- Payen JF, Bru O, Bosson JL, Lagrasta A, Novel E, Deschaux I, Lavagne P, Jacquot C. Assessing pain in critically ill sedated patients by using a behavioral pain scale. Crit Care Med. 2001;29(12):2258–63. [PubMed].
- Phillips ML, Kuruvilla V, Bailey M. Implementation of the Critical Care Pain Observation Tool increases the frequency of pain assessment for non-communicative ICU patients. Australian Critical Care. 2018 Oct 9. [PubMed]
- Ayasrah SM. Pain among non-verbal critically Ill mechanically ventilated patients: Prevalence, correlates and predictors. Journal of critical care. 2018;49:14-20. [PubMed]
- Ayasrah SM, O'Neil TM, Abdalrahim MS, Sutary MM, Kharabsheh MS. Pain assessment and management in critically ill intubated patients in Jordan: A prospective study. Int J Health Sci (Qassim) 2014;8(3):287- 98. [PubMed].
- Al-Sutari MM, Abdalrahim MS, Hamdan-Mansur AM, Ayasrah SM. Pain among mechanically ventilated patients in critical care units. J Res Med Sci. 2014;19(8):726-32. [PubMed]
- Puntillo KA, Max A, Timsit JF, Vignoud L, Chanques G, Robleda G, Roche -Campo F, Mancebo J, Divatia JV, Soares M, Lonescu DC. Determinants of procedural pain intensity in the intensive care unit: the European Am J Respir Crit Care Med 2014;189(1):39–47. [PubMed]
- Gélinas C. Pain assessment in the critically ill adult: recent evidence and new trends. Intensive Crit Care Nurs. 2016;34:1-11. [PubMed] DOI: 1016/j.iccn.2016.03.001
- Kotfis K, Zegan-Baranska M, Szydlowski L, Zukowski M, Ely EW. Methods of pain assessment in adult intensive care unit patients- Polish version of the CPOT (Critical Care Pain Observation Tool) and BPS (Behavioral Pain Scale). Anaesthesiol Intensive Ther. 2017;49(1):66–72. [PubMed]
- Cade CH. Clinical tools for the assessment of pain in sedated critically ill adults. Nurs Crit Care 2008;13(6):288-97. [PubMed] DOI: 1111/j.1478-5153.2008.00294.x
- Gelinas C, Johnston C. Pain assessment in the critically ill ventilated adult: validation of the Critical-Care Pain Observation Tool and Physiologic Indicators. The Clin J Pain 2007;23 (6):497–505. [PubMed]
- Georgiou E, Hadjibalassi M, Lambrinou E, Andreou P, Papathanassoglou ED. The impact of pain assessment on critically ill patients’ Outcomes: A Systematic Review. Biomed Res Int. 2015;2015:503830. doi: 10.1155/2015/503830. [PubMed]