Mohd Saif Khan1, Vaibhav B. Sabnis2, Dilip Shankar Phansalkar3, Smiksha P. Prasad4, Ali Hasan Faiz Karnam5
1Assistant Professor & Consultant Intensivist, Department of Anesthesiology, Emergency and Critical Care, Pondicherry Institute of Medical Sciences, Pondicherry-605014, (India)
2Assistant Professor; 3Professor and Head
Department of Radiodiagnosis, Pondicherry Institute of Medical Sciences, Pondicherry-605014, (India)
4Assistant Professor; 5Assistant Professor and Head
Department of Emergency and Critical Care, Pondicherry Institute of Medical Sciences, Pondicherry-605014, (India)
Correspondence: Dr. Mohd Saif Khan, Assistant Professor & Consultant Intensivist, Department of Anesthesiology, Emergency and Critical Care, Pondicherry Institute of Medical Sciences, Pondicherry-605014, (India)
ABSTRACT
Peripheral venous access is a routine procedure in emergency and critical care areas. However, not all procedures are successful due to altered venous anatomy, varied patient characteristics and blind nature of procedure. Sometimes, this seemingly easy procedure may become difficult, time-consuming, and exasperating. Needle punctures in the process to obtain peripheral venous access can lead to inadvertent arterial punctures, pain, extravasation, localized swelling and patient discomfort. Use of ultrasound improves the probability of achievingvenous access and decreases the rate ofunwanted central line insertions and associated complications. This review will present latest evidence into the use of ultrasound guided peripheral venous access and briefly describe the indications, method and contraindications of this technique in emergency and critical care settings.
Key words: Adult;Vein, Peripheral;Catheterization, Peripheral;Venous access; Ultrasound; Ultrasonics;
Ultrasonography, Interventional/methods; Intensive Care; Catheterization, Central Venous/instrumentation
Citation: Khan MS, Sabnis VB, Phansalkar DS, Prasad SP, Karnam AHF. Use of ultrasound in peripheral venous catheterization in adult emergency and critical care units. Anaesth Pain & Intensive Care 2015;19(3):303-310
INTRODUCTION
Peripheral venous access is the most commonly employed procedure to sample blood and to infuse intravenous medications and fluids. Venous access is an essential prerequisite before performing any procedure in critically ill patients. However, incidence of failed peripheral venous access in the first attempt is about 10% to 21% among emergency department patients.1,2 Intensivists and anesthesiologists are called upon when multiple attempts by nurses and other physicians at accessing peripheral veins fail. There are certain patient groups (e.g. IV drug abusers, obese adults, patients on chemotherapy, severely dehydrated, in-shock, edematous patients, patients with extensive burns) in which peripheral venous access is often limited by the ability to locate the vessel by landmark technique.3In chronically ill patients all accessible peripheral veins have been usually exhausted (thrombosed) and central vascular access or venous cut down seem to be only available choices. Needle punctures in the process to obtain peripheral venous access can lead to inadvertent arterial punctures, pain, extravasations, localized swelling and patient discomfort. In this review, authors attempt to review the latest evidence regarding the use of ultrasound guided peripheral venous (USGPIV) access and also narrate the best practice of USGPIV in the light of current evidence.
LITERATURE REVIEW
Several studies including recent meta-analyses and systematic reviews have shown that the use of bedside ultrasound decreases the number of needle insertion attempts, the number of potentially unnecessary central line placements, and increasedpatient satisfaction scores.4-9 Tables 1 and 2 summarizethe inferences from recent studies and systematic analyses.
Table 1: Studies regarding the use of ultrasound in peripheral venous access
|
First Author, year |
Study design, number of subjects |
Main findings |
| Keyes,4 1999 | Prospective study, 101 patients with difficult IV access |
91% success in cannulating the brachial and basilic veins in ED (Emergency Department) patients with difficult intravenous access |
| Brannam,5 2004 | Prospective, observational study, 321 difficult-to-stick patients. | Emergency nurses had a high success rate (87%) with the use of ultrasound guidance for peripheral vascular access after 45 min of training. |
| Constantino,6 2005 | prospective, systematically allocated study on 60 patients with defineddifficult intravenous access/ | Study revealed a significant increase in success rate (97%) and overall less time (13 minutes) for cannulation of peripheral veins under ultrasound guidance. |
| Bauman,7 2009 | Prospective cohort study on 75 ED patients with difficult IV access | USG guidance improved speed and patient satisfaction with fewer skin punctures and complications. However success rates were similar for both traditional and ultrasound-guided approaches to peripheral access by ED technicians. |
| Stein J,8 2009 | Prospective randomized trial, 59 patients randomized. | Ultrasound guided peripheral intravenous cannulation did not decrease the number of attempts or the time to successful catheterization, nor did it improve patient satisfaction compared with the group that did not use ultrasonography. |
| Gregg,9 2010 | Retrospective cohort review of 77 requests for USGPIV access | Near absolute success rate (99%) was achieved with the use of USGPIV. Thirty four central lines were avoided and 40 central lines were removed as a result of ultrasound-guided peripheral intravenous access being obtained |
| Dargin,10 2010 | Prospective observational study on 75 adult ED patients with difficult IV access who underwent USGPIV access | The overall IV survival rate was 56% with a median survival of 26 hours. |
| Schoenfeld,11 2011 | Questionnaire based survey of 146 patients receiving US-guided IVs | Patient satisfaction with US-guided IVs was very high (9.2 of 10). |
| Au,12 2012 | prospective, observational study, 100 patients with inability to establish IV access | Ultrasound prevented the need for CVC placement in 85% of patients with difficult IV access. |
| Shokoohi,13 2013 | Time-series analysis of 401,532 patients | Marked reduction (by 80%) in central venous catheter use was noted in noncritically ill emergency department patients during the implementation of an ultrasound-guided peripheral intravenous access program. |
Table 2: Input from systematic analysis
|
Main investigator, year |
Design |
Findings |
| Heinrichs J,14 2013 | This review identified 4,664 citations, assessed 403 full texts for eligibility, and included 9 trials. | Ultrasonography may decrease peripheral intravenous cannulation attempts and procedure time in children in ED and operating room settings. Few outcomes reached statistical significance. Larger well-controlled trials are needed. |
| Egan G,15 2013 | Seven papers were eligible to review. | They found ultrasound guidance increased the likelihood of successful cannulation in difficult-access patients, just as the original studies had found (odds ratio 2.42; 95% confidence interval 1.26–4.68). |
| Liu YT,16 2014 |
Six randomized studies could qualify the selection criteria enrolling 316 patients. | The six studies included were found to vary significantly in the definition of difficult venous access, recording of procedure time, definition of success rate, and other important factors, making a meta-analysis inappropriate. |
| Stolz LA,17 2015 |
Seven studies were selected for final analysis. | Ultrasound guidance increased success rates of peripheral venous placement when compared with traditional techniques in patients with difficult peripheral venous access but it had no effect on time to successful cannulation or number of punctures required for successful cannulation. |
TECHNIQUE OF USGPIV ACCESS
Articles to be arranged:
Catheter based cannula (angiocath) of appropriate size (20/18 G), local anesthetic (Lignociane 2%), sterile drape, PPEs, betadine and chlorhexidine prepp solutions. Few sterile gauze pieces, heparinized saline, extension tubing with three-way connector, two tourniquets, sterile ultrasound jelly or betadine solution as contact medium for probe and TegadermTM (10X12 cm; 3M, St. Paul, MN).
Selection of appropriate transducer:
Transducers with High frequency (5-12 MHz) linear array and small footprint are the best for vascular imaging as they can provide higher resolution of the superficial areas of soft tissue (about 2-4 cm below the skin surface).18
Covering the probe to prevent cross contamination
There are various barrier methods described. One method is to apply gel over the transducer’s scanning surface and then put on a sterile glove (or medical condom) over it using no-touch technique. The transducer’s cable can be draped and secured. Another method is to use sterile transparent Tegaderm™ over transducer as shown in Figure 1.
Figure 1: Covering the scanning surface of probe with sterile Tegaderm™ to prevent cross contamination
Orientation of USG probe:
When scanning for vessels in short axis, the indicator should be located to the patient’s right so that the left side of the ultrasound screen corresponds to the left side of the transducer. Any movement of the transducer in the horizontal plane will parallel the same movement on the ultrasound screen.
Optimal scanning modes
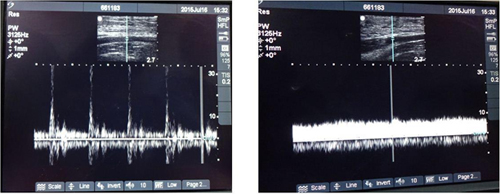
B-Mode and color Doppler are the main ultrasound modes used for the purpose of venous access. B-mode ultrasound produces recognizable two dimensional (2D) gray scale images. Doppler can differentiate arterial (pulsatile) flow from venous (non pulsatile) flow.
Optimizing image quality
Additional settings, which can further enhance the image quality include, gain, depth, focus and frequency. By decreasing the depth setting, the target vessel gets larger. However, a depth setting which is too shallowmay cause important structuresin the vicinity of the target vessel (such as a neighboring artery) to be missed. It is therefore imperative to select the appropriate depth setting according to the target vessel location. Gain (brightness) settings should be just appropriate to visualize the vessel of interest. The gain should be adjusted till the point where slight fill-in with echoes, or white flecks in the vein are visible.19 Veins appear black or anechoic, free of echoes. Excess gain can markedly deteriorate the quality of images owing to enhanced noise artifact. Focus markers should be placed at the level of the area of interest.
Peripheral venous sonoanatomy:
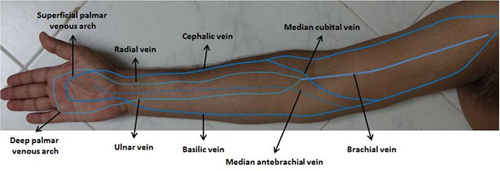
The upper extremity consists of two types of venous channels, superficial and deep which anastomose at various levels via perforating veins. Deep veins accompany arteries. On the back of the hand dorsal arch of superficial veins empties into cephalic and basilic veins on the lateraland medial aspects of the forearm respectively. (Figure 2) The median cubital vein joins the cephalic and the basilic veins on the ventral surface of the elbow. In the upper arm, the cephalic vein terminates in the infraclavicular fossa, and empty into the axillary vein. Basilic vein runs at the medial aspect of the wrist and forearm then penetrates the deep fascia as it courses past the elbow in the upper arm. It then joins with the deep brachial veins to become the axillary vein. The axillary vein becomes the subclavian vein at the lateral border of the first rib. The Brachial vein formed by theulnar and radial veins in front of cubital area, runs in close proximity to brachial artery.
Figure 2: Venous network over ventral aspect of upper limb consisting of deep and superficial venous systems. Deep veins are not visible to naked eyes and hence are the veins of choice for USGPIV access when superficial veins are inaccessible
IDENTIFICATION OF STRUCTURES
Compressibility of veins is the simplest way to distinguish artery from vein. Veins, being thin walled, typically cave in with minimal pressure applied from the probe, while arteries are not compressible and retain original size and shape. The color Doppler is an excellent tool to differentiate artery from vein. Arteries have pulsatile flow visualized on pulse wave Doppler, while the vein has minimal flow(Figure 2).
Figure 3: Use of Doppler to differentiate brachial artery from brachial vein at cubital area. a) Arterial flow is fast pulsatile. b) Venous flow is slow and nonpulsatile
Selection of optimal vein for cannulation:
Before a venepuncture,USG should be performed to assess the size and depth of veins over the forearm and cubital areas. Success rate with USG-PIV has been shown to be higher in veins with larger lumens (≥0.4 cm) and at moderate depth (3-15 mm).24Use of tourniquet can increase the diameter of the vein remarkably.
Catheter selection:
Sandhu and Sidhu advocatethe use ofSeldinger technique to place a catheter longer than two inches inside the vein to prevent catheter dislodgment associated with patient’s limb movements.3 Guidewire based catheters inserted with Seldinger’s technique have better success ratethan normal cannula based catheters (Angiocath™).25A better survival rate for longer catheters has been shown by a latest study.26The only constraint in using guidewire based catheters is the cost, which is relatively lowif the patient comfort and long survival rate of the catheter are taken into consideration.
Procedure:
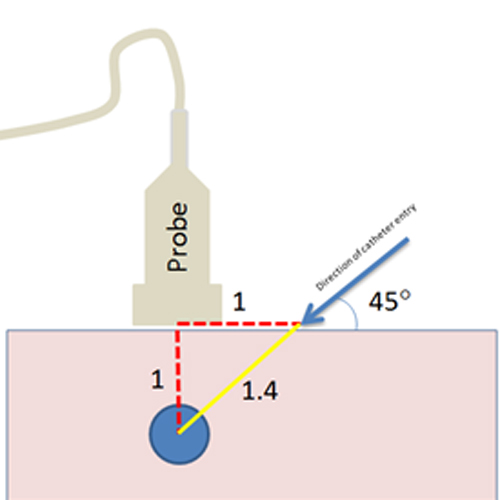
Under aseptic precautions, place the probe over the selected vein using short axis approach and move the probe to keep the vein in the middle of screen. Using short axis technique, operator measures the depth of the vein from the center of the probe using thecursor on the USG screen and the needle entry point is taken at exactlythesame distance from the center of the probe as the depth measured. According to Pythagoras theorem, in any right triangle, the hypotenuse is 1.4 times the length of the equilateral sides of an isosceles-right triangle. Therefore, the distance travelled by the needle to reach the vein will be 1.4 times the depth of vein from the center of the probe. (Figure 4) The angulation of needle entry should be 45°. The tip of theneedle is seen as a hyperechoic structure while advancingtowards the vein. You will stop advancing your needle as soon as target sign is achieved. A flush of backflow of blood will be visible in the hub of catheter, at this point withdraw the introducer needle slightly and advance the catheter over the introducer needle all the way in. Remove the needle and connect the catheter with pre-flushed three-way extension line. Flush the whole system with heparinized saline and apply tegaderm dressing.
Figure 4:Using short axis technique, operator measures the depth of vein from center of the probe using cursor on USG screen and needle entry point is taken exactly atthe same distance from the center of the probe as the depth measured. According to Pythagoras theorem, in any right angle triangle, the hypotenuse* is 1.4 times the length of equilateral sides of an isosceles-right triangle. Therefore, the distance travelled by the needle to reach the vein will be 1.4 times the depth of vein from the center of the probe. The angulation of needle entry should be 45°.[*Hypotenuse is the longest side of a right-angled triangle, the side opposite of the right angle; **A right triangle with the two legs (and their corresponding angles) equal]
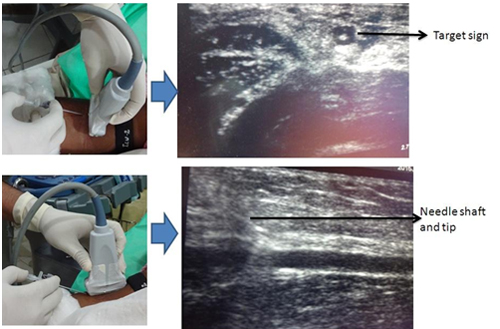
Optimal scanning view
Adjacent structures including arteries and nervesin the area are better visualized with thetransverse (out-of-plane) view; hence it should be the initial scanning view. With this approach, the needle tip is visualized within the vessel lumen as a hyperechoic structure, also known as the“target sign”. As soon as target sign is obtained, the angle between the needle and skin should be dropped and both the needle and catheter are advanced 1 mm to 2 mm farther while keeping the target sign centered and visualized within the vessel.20 One drawback of this approach is unrecognized posterior wall puncture. Long axis (in-plane) view is the gold standard to visualize the tip and shaft of the needle and to track its insertion. However, this approach can also miss the lateral (off track)entry to surrounding structures (artery or nerve). The out-of-plane technique has been shown to be more readily used by less experienced operators.21 In-plane technique is more frequently used by experienced operators.22 However, it is advised to switch between the two views during the procedure as needed to optimize correct needle advancement toward the target vessel. In 2009, a third scanning view was described which was named as oblique view.23 The oblique approach is a cross-angle approach between the transverse and longitudinal approaches which combines the advantages and eliminates the limitations of the two approaches (Figure 5).
Figure 5: Scanning views of peripheral vein. a) Transverse view is obtained when probe’s long axis is perpendicular to needle’s long axis and when needle is inside the vein a hyperechoic dot inside the vein is seen (target sign). b) Longitudinal view (out-of-plane) is obtained when probe’s long axis is parallel to needle’s long axis and needle shaft is clearly visible.
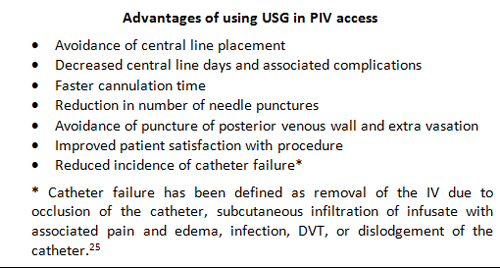
Box 1: Advantages of using USG in PIV access
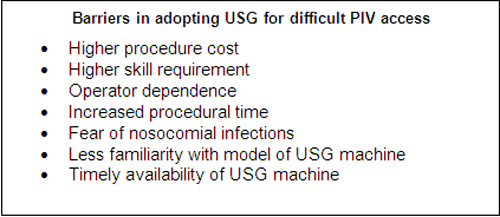
Box 2: Barriers in adopting USG for difficult PIV access:
Advantages of using USG in PIV access
USG guided technique has demonstrable advantages over blind technique in difficult peripheral venous access(Box 1). It clearly cuts short the number of central line insertions, central line days and associated complications.9 It also reduces the number of attempts and needle puncture and hence incidence of extravasations, edema, hematoma, nerve injury and other complications. Incidence of catheter failure is significantly dropped with the use of USG and longercatheters (12 cm).26 USG enhances the success rate of cannulation and increased satisfaction scores among operators as well as in patients.7,11,17
Barriers in adopting USG for difficult PIV access
In spite of growing body of evidence on use of USGPIV access, the technique could not gain expected popularity among ICU residents and physicians. There is a slightly higher preference for central lines as compared to peripheral lines in situations of difficult PIV access due to perceived barriers (Box 2). Till date, we do not have randomized or prospective study looking at the cost effectiveness of USGPIV access. However, Stone et al calculated the averageprocedural cost ($10.38) in his case series and argued that cost of USGPIV access should be weighed against the cost of continuing a standard approach: additional intravenous catheters, increased time to cannulation, and increased patient discomfort.27USGPIV may be presumed to be a difficult skill but can be learnt in a few hours in atraining workshop on phantom models by medical students, ED technicians and nurses.7 The technique’s success depends onoperator’s experience. The success of the technique depends on the experience of the operator. Overall procedural time can be shortened by adopting well structured protocols and checklists. Actual procedure-time is lesser using USG as compared with landmark technique.
COMPLICATIONS
Ultrasound guided peripheral intravenous cannulation is an extremely safe procedure. Paresthesia due to nerve irritation caused bylocal infiltration is the most common complication. However there is no long-term nerve damage reported.28Vascular complications in USGPIV, which are similar to those related to blindapproach but with lesser prevalence, include inadvertent arterial puncture and formation of hematoma, extravasations of fluid, superficial or deep vein thrombosis. The most common infectious complications with US guided IV access are phlebitis and cellulitis. Soft tissue swelling and superficial vein thrombosis can mimicinfection at IV site.
CONCLUSION
Technology of ultrasound is improving in design, robustness of model and imaging quality with each passing day as are the operators with increasing interest and confidence inits use. USGPIV is a simple technique with proven advantages and, therefore, should be routinely practiced in the emergency and critical care settings by nurses, techniciansand doctors in the ED and ICU followingadequate training sessionson phantom models.
REFERENCES
- Fields JM, Piela NE, Au AK, Ku BS. Risk factors associated with difficult venous access in adult ED patients. Am J Emerg Med. 2014 Oct;32(10):1179-82.[PubMed] doi: 10.1016/j.ajem.2014.07.008.
- Sebbane M, Claret PG, Lefebvre S, Mercier G, Rubenovitch J, Jreige R, et al. Predicting peripheral venous access difficulty in the emergency department using body mass index and a clinical evaluation of venous accessibility. J Emerg Med. 2013 Feb;44(2):299-305. [PubMed] doi: 10.1016/j.jemermed.2012.07.051.
- Sandhu NP, Sidhu DS. Mid-arm approach to basilic and cephalicvein cannulationusingultrasoundguidance.BrJ Anaesth. 2004 Aug;93(2):292-4. [PubMed] [Free full text]doi: 10.1093/bja/aeh179.
- Keyes LE, Frazee BW, Snoey ER, Simon BC, Christy D. Ultrasound-guided brachial and basilic vein cannulation in emergency department patients with difficult intravenous access. Ann Emerg Med. 1999 Dec;34(6):711–4. [PubMed]
- Brannam L, Blaivas M, Lyon M, Flake M. Emergency nurses’ utilization of ultrasound guidance for placement of peripheral intravenous lines in difficult access patients. Acad of Emerg Med. 2004 Dec,11(12):1361–3. [PubMed] [Free full text]doi: 10.1197/j.aem.2004.08.027.
- Costantino TG, Parikh AK, Satz WA, Fojtik JP. Ultrasonography-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Ann Emerg Med. 2005;46(5):456–61. [PubMed] doi: 1016/j.annemergmed.2004.12.026.
- Bauman M, Braude D, Crandall C. Ultrasound-guidance vs. standard technique in difficult vascular access patients by ED technicians. Am J Emerg Med. 2009 Feb.27(2):135–40. [PubMed] doi: 10.1016/j.ajem.2008.02.005.
- Stein J, George B, River G, Hebig A, McDermott D. Ultrasonographically guided peripheral intravenous cannulation in emergency department patients with difficult intravenous access: a randomized trial. Ann Emerg Med. 2009 Jul;54(1):33-40. [PubMed]doi: 10.1016/j.annemergmed.2008.07.048.
- Gregg SC, Murthi SB, Sisley AC, Stein DM, Scalea TM. Ultrasound-guided peripheral intravenous access in the intensive care unit. J Crit Care. 2010 Sep;25(3):514-9. [PubMed] doi: 10.1016/j.jcrc.2009.09.003.
- Dargin JM, Rebholz CM, Lowenstein RA, Mitchell PM, Feldman JA. Ultrasonography-guided peripheral intravenous catheter survival in ED patients with difficult access. Am J Emerg Med. 2010 Jan;28(1):1-7. [PubMed] doi: 10.1016/j.ajem.2008.09.001.
- Schoenfeld E, Shokoohi H, Boniface K. Ultrasound-guided peripheral intravenous access in the emergency department: patient-centered survey. West J Emerg Med. 2011 Nov;12(4):475–7. [PubMed] [Free full text] doi: 10.5811/westjem.2011.3.1920.
- Au AK, Rotte MJ, Grzybowski RJ, Ku BS, Fields JM. Decrease in central venous catheter placement due to use of ultrasound guidance for peripheral intravenous catheters. Am J Emerg Med. 2012 Nov;30(9):1950–4. [PubMed] doi: 10.1016/j.ajem.2012.04.016.
- Shokoohi H, Boniface K, McCarthy M, Khedir Al-tiae T, Sattarian M, Ding R, et al. Ultrasound guided peripheral intravenous access program is associated with a marked reduction in central venous catheter use in noncritically ill emergency department patients. Ann Emerg Med. 2013 Feb;61(2):198–203.[PubMed] [Free full text]doi: 10.1016/j.annemergmed.2012.09.016.
- Heinrichs J, Fritze Z, Vandermeer B, Klassen T, Curtis S. Ultrasonographically guided peripheral intravenous cannulation of children and adults: a systematic review and meta-analysis. Ann Emerg Med. 2013 Apr;61(4):444-454.e1. [PubMed] doi: 10.1016/j.annemergmed.2012.11.014.
- Egan G, Healy D, O’Neill H, Clarke-Moloney M, Grace PA, Walsh SR. Ultrasound guidance for difficult peripheral venous access: systematic review and meta-analysis. Emerg Med J. 2013 Jul;30(7):521-6. [PubMed] doi: 10.1136/emermed-2012-201652.
- Liu YT, Alsaawi A, Bjornsson HM. Ultrasound-guided peripheral venous access: a systematic review of randomized-controlled trials. Eur J Emerg Med. 2014 Feb;21(1):18-23. [PubMed] doi: 10.1097/MEJ.0b013e328363bebc.
- Stolz LA, Stolz U, Howe C, Farrell IJ, Adhikari S. Ultrasound-guided peripheral venous access: a meta-analysis and systematic review. J Vasc Access. 2015 Jul 20;16(4):321-6. [PubMed] [Free full text] doi: 10.5301/jva.5000346.
- Resnick JR, Cydulka R, Jones R. Comparison of two transducers for ultrasound-guided vascular access in long axis. J Emerg Med. 2007 Oct;33(3):273-6. [PubMed]
- Jessica R. Ultrasound-Guided Peripheral Venous Access. Israeli Journal of Emergency Medicine. 2006;6(4):46-52 [Free full text]
- Korley F. Ultrasound for Venous Access. In: Carmody KA, Moore CL, Feller-Kopman D, (eds.). Handbook of Critical Care & Emergency Ultrasound. New York, NY: McGraw Hill, 2011, pp. 219–34
- Joing S, Strote S, Caroon L,Wall C, Hess J, Roline C, et al. Videos in clinical medicine. Ultrasound-guided peripheral i.v. placement. N Engl J Med. 2012 Jun;366(25):e38 [PubMed][Free full text] doi:10.1056/NEJMvcm1005951.
- Thomas S, Moore CL. The vanishing target sign: confirmation of intraluminal needle position for ultrasound guided vascular access. Acad Emerg Med. 2013 Oct;20(10):e17-8. [PubMed][Free full text] doi: 10.1111/acem.12228.
- Phelan M, Hagerty D. The oblique view: an alternative approach for ultrasound-guided central line placement. JEmerg Med. 2009 Nov;37(4):403–8. [PubMed] doi: 10.1016/j.jemermed.2008.02.061.
- Witting MD, Schenkel SM, Lawner BJ, Euerle BD. Effects of vein width and depth on ultrasound-guided peripheral intravenous success rates. J Emerg Med. 2010 Jul;39(1):70-5. [PubMed] doi: 10.1016/j.jemermed.2009.01.003.
- El-Shafey EM, Tammam TF. Ultrasonography-Guided Peripheral Intravenous Access: Regular Technique Versus Seldinger Technique in Patients with Difficult Vascular Access. Eur J Gen Med 2012 Nov;9(4):216-22. [Article Online]
- Elia F, Ferrari G, Molino P, Converso M, De Filippi G, Milan A, et al. Standard-length catheters vs long catheters in ultrasound-guided peripheral vein cannulation. Am J Emerg Med. 2012 Jun;30(5):712-6. [PubMed] doi: 10.1016/j.ajem.2011.04.019.
- Stone BA. Ultrasound Guidance for Peripheral Venous Access: a simplified seldinger technique. Anesthesiology 2007 Aug;107(2):195. [Free full text] doi:10.1097/01.anes.0000271927.37624.63.
- Mills CN, Liebmann O, Stone MB, Frazee BW. Ultrasonographically guided insertion of a 15-cm catheter into the deep brachial or basilic vein in patients with difficult intravenousaccess. Ann Emerg Med 2007 Jul;50(1):68-72. [PubMed]