Kewal Krishan Gupta, MD1, Joginder Pal Attri, MD2*, Amanjot Singh, MD1
1Assistant Professor, Department of Anesthesiology & ICU, Guru Gobind Singh (GGS) Medical College & Hospital, Faridkot, Punjab, (India)
2Associate Professor, Department of Anesthesiology & ICU, Government Medical College (GMC) Amritsar, Punjab, (India)
Correspondence: Dr. Kewal Krishan Gupta, House No. 204, Medical Campus, Faridkot- 151203, Punjab, (India); Tel: +91-9988316306; E-mail: doc_krishan31@yahoo.co.in
ABSTRACT
Upper limb procedures are commonly carried out under brachial plexus block alone or in combination with general anesthesia. . The brachial plexus block can be performed by either of the techniques – blind; nerve stimulator (NS)-guided or ultrasound (US)-guided technique. But the introduction of ultrasound has revolutionized the puncture techniques dramatically since last decade. For successful and safe block, direct visualization for diffusion areas of drugs is recommended than targeting the nerves directly. The aim of this article is to review the different ultrasound-guided approaches used for brachial plexus block.
Key words: Brachial plexus block; Ultrasound; Nerve stimulator
Citation: Gupta KK, Attri JP, Singh A. Ultrasound guided brachial plexus block. Anaesth Pain & Intensive Care 2016;20(2):187-192
INTRODUCTION
In anesthesia practice, efforts to incorporate ultrasound are fundamentally rooted in the goals of improving patient safety and interventional anesthesia efficacy. Currently a focus for anesthesia education is the use of ultrasound techniques for vascular access and regional anesthesia, but the introduction of this technology presents novel challenges of acquiring new knowledge and skill sets to achieve these goals. The use of imaging modalities to speed performance and improve the success rate of regional anesthesia is currently under trial.1,2
Proper identification of the nerve bundle is very important to inject local anesthetic. Various methods like paresthesia technique, nerve stimulator and ultrasound are being used to identify the nerve bundle. The oldest one is the paresthesia technique with complications like inadequate block, failed block, in-advertent vascular puncture and temporary damage of the nerve. To locate the nerve bundle with nerve stimulator, the equipment necessary is compact and relatively inexpensive. In skilled hands, it has been observed that high success rates are achievable when performing peripheral blocks guided by surface anatomy and neurostimulation.4,5 The disadvantages of nerve stimulator include patient discomfort requiring sedation5, lack of evoked response even when the needle to nerve distance is minimized, and complications due to penetration of adjacent vascular or other structures by the stimulating needle.
ADVANTAGES OF USG
Due to number of advantages (Table 1), Ultrasound has largely superseded others techniques within last few years. There is now level 1b evidence available demonstrating that ultrasound-guidance improves both the quality and the speed of block onset.6
| Table 1: Advantages of ultrasound
Direct real time image of neural structures Direct visualization of surrounding structures (blood vessels, bones) facilitating nerve identification Correct needle placement Direct observation of local anesthetic spread Less chances of intraneuronal / intravascular injection Decreased complications (e.g. pleural puncture) Rapid onset of block and use of less local anesthetic dosage Avoidance of fracture-site pain with nerve stimulation Compensation for anatomical variation with different approaches (not landmark dependent) |
However, to execute these advantages into a safe and effective regional anesthesia, an anesthesiologist must have a thorough knowledge of relevant sonoanatomy and better understanding in basic principles of ultrasound with related applications. Along with this, regular practice with ultrasound is also essential.
In this article, we will mainly review the various ultrasound-guided approaches used for brachial plexus block along with their relevant sonoanatomy and problem. In addition, a brief analysis of the literature about brachial plexus block is also provided.
TECHNICAL ASPECTS OF ULTRASOUND
A detailed discussion regarding physics and technical intricacies of ultrasound imaging is beyond the scope of this article; however certain basic aspects that strongly influence image quality are worth highlighting. Higher frequency probes can produce stunningly detailed images of superficial structures, including the brachial plexus at the interscalene, supraclavicular, axillary, and mid-humeral levels.7 However, higher spatial resolution is achieved at the expense of lower penetration, making deeper structures such as the brachial plexus at the infraclavicular level more difficult to visualize with a high frequency than with a low- or mid-frequency probe.8, Needle visualization is only possible when ultrasound is reflected from the needle back to the probe. Needle size, as well as the angle of introduction, also play an important role in determining the amount of ultrasound reflected back to the probe, with larger needles and shallower angles of introduction allowing better visualization.9 When viewed with ultrasound, nerves can be hyper- or hypoechoic, depending on the level and angle at which they are viewed, the density of surrounding structures, and individual variations.
- Interscalene brachial plexus block
Surgeries involving shoulder, proximal humerus and lateral clavicle are reliably performed under interscalene brachial block anesthesia. At interscalene level, target nerve roots of brachial plexus are sandwiched between the anterior and the middle scalene muscles. To perform this block, patient is positioned supine with head slightly elevated and turned towards opposite side of the block. The operator sits on the side of operative limb with ultrasound machine on opposite side of the patient table to align eye, probe, needle and screen in one direction.
A High frequency linear probe (8-13 MHz) is used to scan the neck transversely between the level of cricoid cartilage and supraclavicular fossa. At the interscalene level, the brachial plexus roots often appear as hypoechoic nodules arranged like peas in a pod between the anterior and middle scalene muscles (Figure 1). The lack of a vascular landmark may make localization of the nerve roots or trunks more difficult, especially for the beginner with ultrasound. So it may be useful to visualize the brachial plexus at the supraclavicular level, and then follow the nerves back up into the interscalene groove (Traceback approach). The block needle is then carefully inserted either parallel (in-plane technique) or perpendicular (out-of-plane technique) to the probe. For single injection nerve block, in-plane approach is commonly recommended but for siting a catheter between the two muscles for postoperative infusion analgesia, an out-of-plane approach (in caudal direction) may be useful. Earlier, higher drug volume (20-40 ml) was used for nerve stimulator or paraesthesia guided block. However, the advent of ultrasound has decreased the minimum effective drug volume i.e. 10-15 ml. Visualization of the nerve roots bathed in local anesthetic in an interscalene groove distended by the injected solution reliably predicts success. The rare, but disastrous pulmonary and neurological complications associated with old technique of interscalene brachial plexus block have made ultrasonography an attractive guidance modality.10,11

|
Figure 1- Interscalene region sonoanatomy showing brachial plexus roots (N) as hypoechoic nodules between two muscles. SCM= Sternoclediomastoid muscle, ScA= Anterior scalene muscle, ScM= Medial scalene muscle, N= nerve root. |
- Supraclavicular Brachial plexus block
Supraclavicular route of brachial plexus block is consider as ‘The Spinal of Arm’, in which local anesthetic agent is delivered at a point where the three trunks are compactly arranged and carry entire sensory, motor and sympathetic innervations of the upper extremity.12 This block is routinely performed to provide surgical anesthesia and analgesia for procedures from mid-arm proximally to the hand distally. Preparation of the patient is done in the same position as for the interscalene approach.
Here a linear ultrasound high-frequency probe is kept above the clavicle to scan the supraclavicular fossa in a coronal-oblique plane, to obtain the relevant short-axis view of the subclavian artery, first rib, pleura, and tightly packed nerve plexus, which are typically seen as a bunch of grapes lying cephalodorsally to the subclavian artery (Figure 2). While injecting the drug, ensure anterior displacement of nerve plexus and distribution of local anesthetics all around the nerves. .The multiple injection technique has been found comparable to the single-shot technique (at the junction between the artery and the first rib) which is easier to perform.13,14 However, many studies fail to demonstrate the reduction in minimum effective volume of local anesthetic to produce adequate blockade with US guided supraclavicular block. Almost all anesthesiologist are still using 30 mL of local anesthetic with a recent study reporting use of 32 ml as the minimum effective volume in 90% of patients.15 Although adjacent structures such as the lung and pleura are clearly visualized and, therefore, easy to avoid as long as the location of the needle tip is known. Subramanyam et al. found that the reluctance of the operators to place the needle tip close to the pleura for fear of pneumothorax have resulted in slower onset of ulnar nerve blockade and ulnar nerve sparing still remains an issue with this technique.16 Technical difficultly encountered in this approach is due to the presence of the supraclavicular depression, which has made manipulation of the probe and puncture needle more complex and demands solid experience with ultrasound guidance.
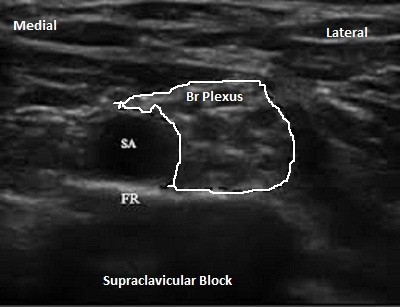
|
Figure 2: Supraclavicular region sonoanatomy showing brachial plexus as bunch of grapes superolaterally to subclavian artery. SA= Subclavian artery, FR= First rib. |
- Infraclavicular plexus block
As it was one of the less favored approach for block because of the complexity of anatomical landmarks and high incidence of vascular puncture, these days introduction of ultrasound has increased its popularity. Surgery involving lower arm, forearm and hand can reliably performed under this block. This approach is also preferred for placing the catheter for continuous infusion analgesia. Anatomically, the brachial plexus gets divided into 3 cords at this level which are compactly organized medially, laterally and inferiorly to the axillary artery. The patient is positioned supine with arm adducted and the operator stands on the head side of patient. The probe is placed in infaclavicular region, medial to the coracoid process and parallel to the rostrocaudal axis. In view of the increased depth of brachial plexus at this level with respect to other techniques, low frequency probe (5 to 7.5 MHz) may be preferred. On ultrasound, the three hyperechoic round cords of the plexus is seen around the axillary artery with axillary vein on medial side (Figure 3). The block needle is inserted below the clavicle by in-plane technique and the local anesthetic is injected postero-lateral to the axillary artery (5-7 o’clock position) ensuring a good spread (U shape) around the artery for successful block. This hypothesis has been supported by multiple clinical trials.17,18 A fascial click felt just before reaching the posterior aspect of the artery confirms right position of needle tip. Most authors use 30 mL of local anesthetic for this block. Major limitations for US guided infraclavicular block include technical difficulty in visualizing the plexus with block needle at this depth with high frequency probes and chances of vascular puncture due to anatomical variations.
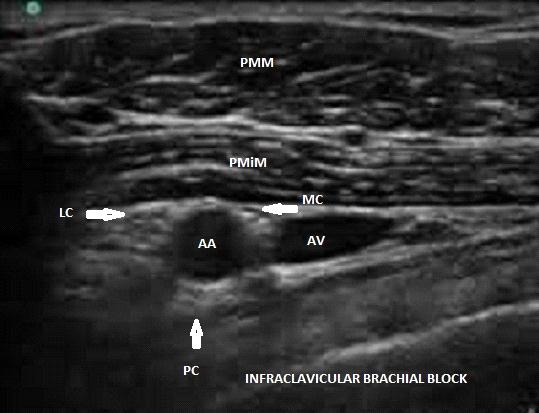
| Figure 3: Infraclavicular region sonoanatomy showing cords of brachial plexus as hyperechogenic structures around axillary artery.
PMM= Pectoralis major, PMiM= Pectoralis minor, AA= Axillary artery, AV= Axillary vein, MC= Medial cord, PC= Posterior cord, LC= Lateral cord. |
- Axillary block
This approach is routinely indicated for operative procedures involving elbow, forearm, and hand. Anatomically, in this region axillary artery is surrounded by the median, radial and ulnar nerves and the musculocutaneous nerve is usually found between coracobrachialis and the biceps bachialis muscle (Figure 4). The patient lays supine with arm extended and abducted by 90 degree. The anesthesiologist sits above the patient’s arm and the high frequency probe is placed perpendicularly to the arm’s axis to obtain short axis view of neurovascular structure. Rapid and precise depositions of local anesthetic on either side of the artery (vascular landmark technique) or directly next to individually identified nerves have shown good results. Success rate with two injections technique (one around the musculocutaneous nerve and another posterior to the axillary artery) has been compared and found equivalent to four injections technique by recent studies.19,20 A study by Gonzalez et al. found that the minimum effective volume to block the musculocutaneous nerve is 5.5 ml with a further 23.5 ml for perivascular injection to block the remaining nerves in 90% of patients.21 Due to increased ability of the operator to identify the anatomical variation with ultrasound in this region, has resulted in better success rate with this block. Beginner with ultrasound should practice this approach, as the possibility of lesser serious complications compared with other proximal approaches and the need for the multiple needle manipulation to block the individual nerves provides valuable practical experience. Major pitfalls of this approach include sparing of radial nerve due to poor visibility and inadvertent i.v local anesthetic injection due to loss of visualization of needle tip. Therefore repeated aspiration and incremental injection should always be practiced.
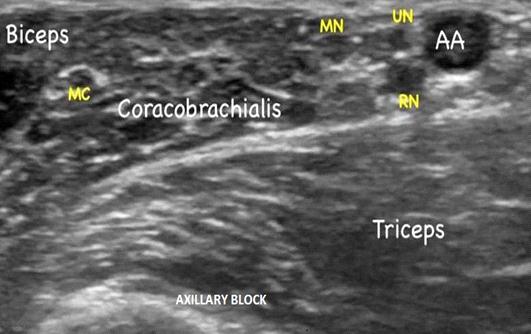
| Figure 4: Axillary region sonoanatomy showing different nerves of brachial plexus around axillary artery.
AA= Axillay artery, UN= Ulnar verve, RN= Radial nerve, MN= Median nerve, MC= Musculocutaneous nerve. |
DISCUSSION
The choice of technique for brachial plexus block varies depending upon the site of surgery, experience of the anesthesiologist and the patient’s clinical status. One has to remember that nerves are not blocked by the needle but by the local anesthetic. The older techniques used for nerve blocks have consistently failed to meet this perfectly logical requirement. As US guidance provides real-time image of the block needle, the brachial plexus, and its anatomical relationship to the surrounding vital structures; it has not only increased the success rates, but also has reduced the complication rates. Most of the studies show use of US guidance for performing brachial plexus block, results in near 100% success with or without complications. Though still in its infancy, US guided regional anesthesia has already demonstrated advantages over neurostimulation, whether it be in terms of block execution times or block quality.22
Mithun Duncan et. al concluded high success rate in US and NS group guidance for performing supraclavicular brachial plexus blocks and a decreased incidence of complications that are associated with the blind technique. The US-guided technique also have shown an edge over the NS-guided technique.23 Use of neurostimulation in conjuction with ultrasound has been practiced by some anesthesiologist but there is little evidence that this approach has improved the block quality in patients. Different studies have evaluated the minimum local anesthetics doses for individual blocks and found that lesser drug volume is required with ultrasound guidance in comparison to other traditional methods, although this finding was inconsistent with infraclavicular and supraclavicular approaches. Ferraro demonstrated that with the use of ultrasound it is possible to perform the brachial plexus block achieved by axillary approach with a minimum effective volume of 0.5% bupivacaine with 1:200,000 epinephrine (1.56 mL) for each nerve in hand surgery.24
N.S. Sandhu et al. demonstrated that ultrasound guided perineural deposition of drug, has improved the success rate and decreased the complications of infraclavicular brachial plexus block.8 An another study on infraclavicular block had also reported improved success rate (almost 100%) with the use of ultrasound guidance .25
Despite these potential benefits, studies on the comparison of long-term complications such as nerve injury and local anesthetic toxicity with ultrasound guidance compared with other standard techniques are still sparse. Although a recent prospective analysis by Sites et al. of 12668 ultrasound-guided nerve blocks over an 8-yr period had reported only one case of inadvertent intravascular injection of local anesthetic complicating into seizures.26 According to another study, the learning curves for neurostimulation guided blocks are long and it estimated that >60 brachial plexus blocks need to be performed to achieve a loosely defined success rate of 87%. In contrast, US guidance allows relatively inexperienced practitioners to achieve high success rates after only a few blocks.27
The dissemination of ultrasound guidance technique is mainly limited by the cost and the availability of ultrasound device. But no doubt, it is a onetime capital expense, that will be used over a large number of patients, becoming cost effective, especially when the time saved for each procedure and patient safety are taken into account.28
CONCLUSION
The rapid learning, less complication rate, low level of patient discomfort and more success rates with US-guided blocks have increased its use among anesthesiologist, all over the world. The benefits of direct visualization of targeted nerve structure and the distribution of local anesthetic are significant. In addition, uses of lower volume of drugs with ultrasound have increased patient’s safety profile. Although the learning curve is short, proficiency with US guided block is not instantaneous. So we recommend, novice anesthesiologists wishing to use ultrasound must give themselves, their hands, and their eyes time to practice the technique.
Conflict of interest: None declared by the authors
Author contribution: All of the authors took part in preparation of the manuscript
REFERENCES
- Mukherji SK, Wagle A, Armao DM, Dogra S. Brachial plexus nerve block with CT guidance for regional pain management: initial results. Radiology. 2000;216:886-90. [PubMed] [Free full text]
- Nishiyama M, Naganuma K, Amaki Y. A new approach for brachial plexus block under fluoroscopic guidance. Anesth Analg 1999;88:91-7. [PubMed]
- La Grange P, Foster PA, Pretorius L. Application of the doppler ultrasound blood flow detector in supraclavicular brachial plexus block. Br J Anaesth 1978; 50:965-7. [PubMed] [Free full text]
- Carles M, Pulcini A, Macchi P, Duflos P, Raucoules AM, Grimaud D. An evaluation of the brachial plexus block at the humeral canal using a neurostimulator (1417 patients): the efficacy, safety, and predictive criteria of failure. Anesth Analg. 2001;92:194-8. [PubMed]
- Fanelli G, Casati A, Garancini P, Torri G. Nerve stimulator and multiple injection technique for upper and lower limb blockade: failure rate, patient acceptance, and neurologic complications. Study Group on Regional Anesthesia. Anesth Analg 1999;88:847-52. [PubMed]
- Liu SS, Ngeow J, John RS. Evidence basis for ultrasound-guided block characteristics: onset, quality, and duration. Reg Anesth Pain Med. 2010 Mar-Apr;35(2 Suppl):S26-35.doi: 10.1097/AAP.0b013e3181d266f0. [PubMed]
- Perlas A, Chan VW, Simons M. Brachial plexus examination and localization using ultrasound and electrical stimulation: a volunteer study. Anesthesiology. 2003;99:429-35. [PubMed] [Free full text]
- Sandhu NS, Capan LM. Ultrasound-guided infraclavicular brachial plexus block. Br J Anaesth. 2002;89(2):254–9. [PubMed] [Free full text]
- Schafhalter-Zoppoth I, McCulloch CE, Gray AT. Ultrasound visibility of needles used for regional nerve block: an in vitro study. Reg Anesth Pain Med 2004;29:480-8. [PubMed]
- Childs SG. Tension pneumothorax: a pulmonary complication secondary to regional anesthesia from brachial plexus interscalene nerve block. J Perianesth Nurs 2002;17:404-10. [PubMed] [Free full text]
- Benumof JL. Permanent loss of cervical spinal cord function associated with interscalene block performed under general anesthesia. Anesthesiology 2000;93:1541-4. [PubMed] [Free full text]
- Morgan, GE; Mikhail, MS; Murray, MJ (2006). “Peripheral nerve blocks”. In Morgan, GE; Mikhail, MS; Murray, MJ. Clinical Anesthesiology (4th ed.). New York: McGraw-Hill Medical. pp. 283–308.
- Tran DQ, Munoz L, Zaouter C, Russo G, Finlayson RJ. A prospective, randomized comparison between single- and double injection, ultrasound-guided supraclavicular brachial plexus block. Reg Anesth Pain Med 2009;34: 420-4. doi: 10.1097/AAP.0b013e3181ae733a. [PubMed]
- Roy M, Nadeau MJ, Cote D, Levesque S, Dion N, Nicole PC et al. Comparison of a single- or double-injection technique for ultrasound-guided supraclavicular block: a prospective, randomized, blinded controlled study. Reg Anesth Pain Med 2012; 37: 55-9. doi: 10.1097/AAP.0b013e3182367b97. [PubMed]
- Tran de QH, Dugani S, Correa J, Dyachenko A, Alsenosy N, Finlayson RJ. Minimum effective volume of lidocaine for ultrasound-guided supraclavicular block. Reg Anesth Pain Med 2011; 36: 466–9. doi: 10.1097/AAP.0b013e3182289f59. [PubMed]
- Subramanyam R, Vaishnav V, Chan VWS, Brown SD, Brull R. Lateral versus medial needle approach for ultrasound-guided supraclavicular block: a randomised controlled trial. Reg Anesth Pain Med 2011; 36: 387–92. doi: 10.1097/AAP.0b013e318217ab1f. [PubMed]
- Desgagnes MC, Levesque S, Dion N, Nadeau MJ, Cote D, Brassard D et al. A comparison of a single or triple injection technique for ultrasound-guided infraclavicular block: a prospective randomized controlled study. Anesth Analg 2009; 109: 668-72. [PubMed]
- Tran DQ, Bertini P, Zaouter C, Munoz L, Finlayson RJ. A prospective, randomized comparison between single- and double injection ultrasound-guided infraclavicular brachial plexus block. Reg Anesth Pain Med 2010; 35: 16-21. doi: 10.1097/AAP.0b013e3181c7717c.[PubMed]
- Imasogie N, Ganapathy S, Singh S, Armstrong K, Armstrong P. A prospective, randomized, double-blinded comparison of ultrasound- guided axillary brachial plexus blocks using 2 versus 4 injections. Anesth Analg. 2010; 110: 1222-6. [PubMed]
- Bernucci F, Gonzalez AP, Finlayson RJ, Tran DQ. A prospective, randomized comparison between perivascular and perineural ultrasound-guided axillary brachial plexus block. Reg Anesth Pain Med 2012; 37: 473-7. doi: 10.1213/ANE.0b013e3181cb6791 [PubMed]
- Gonzalez AP, Bernucci F, Pham K, Correa JA, Finlayson RJ, Trande QH. Minimum effective volume of lidocaine for double-injection ultrasound guided axillary block. Reg Anesth Pain Med 2013; 38: 16–20. doi: 10.1097/AAP.0b013e3182707176. [PubMed]
- Williams SR, Couinard P, Arcand G, Harris P, Ruel M, Boudreault D, et al. Ultrasound guidance speeds execution and improves the quality of supraclavicuar block Anesth Analg 2003;97:1518–23. [PubMed]
- Duncan M, Shetti AN, Tripathy DK, Roshansingh D, Krishnaveni N. A comparative study of nerve stimulator versus ultrasound-guided supraclavicular brachial plexus block. Anesth Essays Res 2013;7(3):359-64. doi: 10.4103/0259-1162.123235. [PubMed] [Free full text]
- Takeda A, Ferraro LHC, Rezende AH, Sadatsune EJ, Falcão LFR, Tardelli MA. Minimum effective concentration of bupivacaine for axillary brachial plexus block guided by ultrasound. Revista Brasileira de Anestesiologia. 2015;65(3):163-9. [Free full text ]
- Ootaki C, Hayashi H, Amano M. Ultrasound-guided infraclavicular brachial plexus block: anlternative technique to anatomical landmark-guided approaches. Reg Anesth Pain Med. 2000;25(6):600–4. [PubMed]
- Sites BD, Taenzer AH, Herrick MD, Gilloon C, Antonakakis J, Richins J, et al. Incidence of local anaesthetic systemic toxicity and postoperative neurologic symptoms associated with 12,668 ultrasound-guided nerve blocks: an analysis from a prospective clinical registry. Reg Anesth Pain Med. 2012; 37: 478–82. [PubMed] doi: 10.1097/AAP.0b013e31825cb3d6.
- Konrad C, Schupfer G, Wietlisbach M, Gerber H. Learning manual skills in anesthesiology: Is there a recommended number of cases for anesthetic procedures? Anesth Analg 1998;86:635-9. [PubMed]
- Mehta SS, Shah S. Comparative study of supraclavicular brachial plexus block by nerve stimulator vs ultrasound guided method. NHL Journal of Medical Sciences 2015;4:49-52. [Free full text]

