Vibhuti A. Shah1, Manan Bajaj2, Khushali R. Tilvawala2
1Associate Professor, Department of Anesthesiology, AMC MET Medical College, Sheth LG Municipal General Hospital, Balvatika, Archana Society, Bhairavnath, Maninagar, Ahmedabad, Gujarat 380008, (India)
2Resident, Department of Anesthesiology, Smt. NHL Municipal Medical College, Kocharab, Paldi, Ahmedabad, Gujarat 380006 (India)
Correspondence: Dr Vibhuti A. Shah, Associate Professor, Department of Anesthesiology, AMC MET Medical College, Sheth LG Municipal General Hospital, Balvatika, Archana Society, Bhairavnath, Maninagar, Ahmedabad, Gujarat 380008, (India); E-mail: drpiyushpujara@gmail.com
ABSTRACT
Background: Abdominal field blocks with local anesthetic solutions have been suggested in postoperative analgesia in patients undergoing abdominal wall incisions. In the present study we assessed the analgesic efficacy of ultrasound guided rectus sheath and transversus abdominis plane blocks over first 24 postoperative hours after cesarean deliveries performed through pfannensteil or midline incisions.
Methodology: Sixty women undergoing elective or emergency cesarean delivery were enrolled in this randomized, controlled, double-blind trial, and then randomized either to undergo ultrasound guided rectus sheath and transversus abdominis plane blocks with bupivacaine (n=30) or no block (n=30). Inj diclofenac and inj. paracetamol 1 G, were given to all patients, and inj tramadol was given on request as a rescue analgesic. All patients received a spinal anesthesia with 0.5% heavy bupivacaine, and at the end of surgery (after the skin sutures) bilateral rectus sheath and transversus abdominis plane blocks were performed using 15 to 20 ml of 0.25% bupivacaine in each block on either side (to maximal dose of 3 mg/kg) and no block in the control patients. Each patient was evaluated postoperatively by a blinded investigator at 2, 4, 6, 12 and 24 h postoperatively.
Results: Ultrasound guided abdominal field blocks with 0.25% bupivacaine reduced the total tramadol requirement in the first 24 postoperative hours (157 ± 50.709 vs 386.67 ± 29.16 mg) and also the visual analogue pain scores at 2 (2 vs 8) ,4 (2 vs 8),6 (2 vs 8),12 (4 vs 7) and 24 (4 vs 7) hours postoperatively. No significant difference was found between groups in the incidence of nausea. Sedation was reduced in the patients who received the blocks. There were no complications attributed to the blocks.
Conclusion: Ultrasound guided abdominal field blocks, as a part of a multimodal analgesic regimen, provided greater analgesia up to 24 h postoperatively after elective or emergency cesarean delivery.
Key words: Abdominal field blocks; Lower segment cesarean delivery; Rectus sheath block; Transversus abdominis plane block.
Citation: Shah VA, Bajaj M, Tilvawala KR. Ultrasound guided abdominal field blocks improve postoperative pain relief in cesarean delivery: a prospective randomized controlled study. Anaesth Pain & Intensive Care 2017;21(2):218-223
Received: 9 November 2016; Reviewed: 15 November 2017, 6 April 2017; Corrected: 1 December 2016, 9 April 2017; Accepted: 14 June 2017
INTRODUCTION
Cesarean delivery is one of the mainly widespread surgical procedures performed worldwide.1 Pregnancy is linked with augmented excitability of mechanosensitive afferent nerve fibers innervating the uterine cervix and lower uterine corpus. The change in sensitivity of the nerve fibers is probably, at least in part, due to elevated oestrogen levels during pregnancy.2,3 Whether skin and visceral nociception are transmitted by dissimilar fibre subgroups is controversial.4 The uterine (visceral) afferent fibers stimulated by pressure and vasoconstriction primarily comprise C fibers and some A-delta fibers. By contrast, the majority of afferent fibers that communicate nociceptive stimuli from the skin are A-delta fibers. Post-cesarean pain results from straight trauma to nerve endings and/or following inflammation induced by tissue injury. Local and systemic inflammatory cytokines act to sensitize the peripheral nerves and improve pain perception.5 Inflammation, possibly plays an important role in pain after delivery because inflammatory cytokines are elevated as a part of the normal labor and delivery process.6,7 Multimodal therapies are commonly used to treat postoperative pain after cesarean delivery.
Recently, the use of ultrasound guided abdominal field blocks have been popular. This technique delivers local anesthetic accurately into the transversus abdominis fascial plane and posterior rectus sheath. These are commonly used for operations that involve incision of the abdominal wall. For midline or paramedian incision extending above the umbilicus, rectus sheath block is used. Median incision requires bilateral rectus sheath block (RSB) while paramedian incision (over a single rectus muscle) requires a unilateral RSB in the surgical side. For transverse or pfannenstiel incisions below the umbilicus a standard TAP block and for transverse or Kocher incision above the umbilicus an oblique subcostal TAP block is used (Figure 1).
Most of the studies till date compare intrathecal morphine or diamorphine use with or without TAP blocks to postoperative morphine requirements. Low resource countries also face challenge of lack of supply of long acting preservative free opioids and monitoring issues when hydrophilic opioids are used.
Our hospital receives a number of previous cesarean deliveries/laparotomies which were done with a midline incision. Sometimes the incision reached the umbilicus and sometimes crossing the umbilicus, so we thought of combining the two abdominal field blocks for all patients.
The present study was designed to assess the analgesic efficacy of combined TAP block and RSB in reducing post cesarean delivery pain and opioid requirements.
METHODOLOGY
The study was designed as a prospective, randomized, double blind study comprising of ASA I/II/III adult female patients undergoing elective or emergency cesarean delivery at Seth LG Hospital, Ahmedabad. The study was performed from April 2015 to June 2015. Patients were blinded to the treatment as was the anesthesiologist involved in postoperative data collection. Patients allergic to local anesthetics, those with skin conditions precluding the block, preoperative chronic dependence on opioid medication, or procedural difficulties in visualising and performing TAP or RS blocks and conversion to general anesthesia, were excluded from the study. The allocation sequence was achieved by a computer generated table of random numbers. Patients were randomly allocated into two groups: Group RTS, allocated with the ultrasound guided rectus sheath & transversus abdominis plane block with spinal anesthesia, and Group S, spinal anesthesia group.
All patients received subarachnoid block with 2 ml of 0.5% heavy bupivacaine. A 25 G spinal needle was used for the same.
At the end of the surgery (after the completion of skin sutures), the Group RTS received bilateral transversus abdominis plane and rectus sheath blocks. The blocks were performed by one of the two anesthesiologists with expertise in ultrasound guided blocks.
Ultrasound guided rectus sheath block technique: The skin was disinfected and a high-frequency linear array transducer 13-6 MHz (HFL38x) was connected to portable USG machine (M-Turbo; Sonosite, Bothell, Washington, USA) placed immediately lateral to the planned incision in a transverse direction. The needle (23G L 90 mm; BD spinal needle) was inserted through cephalad to caudad direction, all the way through the subcutaneous tissue, to stab through the anterior rectus sheath. The needle was advanced through the body of the muscle until the tip rested on the posterior rectus sheath. After negative aspiration, hydro-dissection was done (with 1-2 ml of the drug) to verify needle tip location. When injection of local anesthetic appeared intramuscular, the needle was more advanced 1-2 mm and its location was rechecked by hydro-dissection. This was repeated until the correct needle position was achieved. 15 to 20 ml of 0.25% bupivacaine was injected on each side (Figure 1).
Figure 1: Hypoechoic area showing drug spread in posterior rectus sheath (black arrows)
Ultrasound guided transversus abdominis plane block (posterior injection) technique: The high frequency linear array transducer 6 -13MHz (HFL38x) was placed horizontally athwart the abdomen. The muscle layers in the antero-lateral part of the abdomen could be traced by scanning from midline to the area between the iliac crest and the coastal margin, in the mid-axillary line. The rectus abdominis muscle was recognized, just off the midline, as an oval / elliptical structure. As we scanned laterally the rectus abdominis muscle abuts a fascial plane (linea semilunaris). This fascial plane then gives increase to 3 muscle layers: external oblique, internal oblique and transversus abdominis. The ultrasound transducer was enthused to scan laterally where the 3 muscle layers can be seen running parallel to one another. The transducer was moved posteriorly, aiming to view the point where the transversus abdominis muscle begins to tail off. With sufficient ultrasound image, the needle (23G L 90mm; BD spinal needle) was inserted anterior to the transducer. This allows an in-plane view of the needle as the transversus abdominis plane was pierced. The local anesthetic was then gradually injected. If the needle was accurately positioned, the fascial plane was seen to separate and form a well-defined, hypoechoic, elliptical shape between the internal oblique and transversus abdominis muscles. 15 to 20 ml of 0.25% bupivacaine per side was injected (Figure 2).
The total amount of drug was always less than 3 mg/kg.
Group S only received spinal anesthesia with 0.5% heavy bupivacaine.
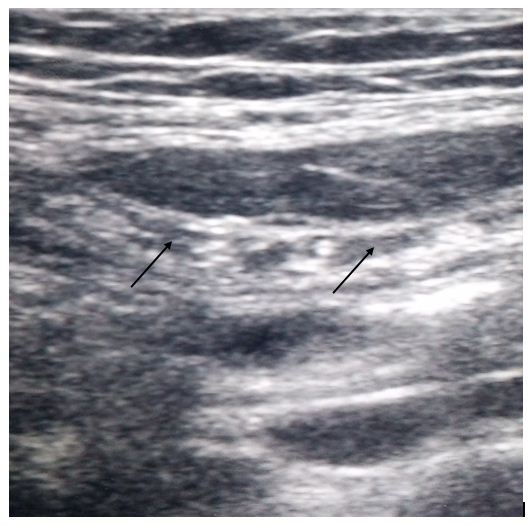
Figure 2: Hypoechoic area showing drug spread in transversus abdominis plane (black arrows)
Postoperatively, patients were transferred to the recovery unit. In the recovery unit, all patients received postoperative analgesia in the form of 1 g of paracetamol and 75 mg of diclofenac intravenously every 8 h. Additional analgesia for breakthrough pain in the form of 100 mg tramadol intravenously was given.
Outcome data were collected by a third anesthesiologist who was blinded to the treatment group of individual patients. First demand for analgesia and the total tramadol requirements were noted. The occurrence and severity of pain, nausea and sedation were assessed systematically. These evaluations were performed in the recovery unit at 2, 4, 6, 12 and 24 h postoperatively. All patients were requested to provide scores for their pain at rest. Pain severity was calculated by using visual analogue scale VAS was explained to the patient just before giving the block. The patients were enquired about the complaint of nausea and sedation. Rescue anti-emetics were accessible to any patient who complained of nausea and vomiting. The study finished 24 h after blockade (Figure 3).
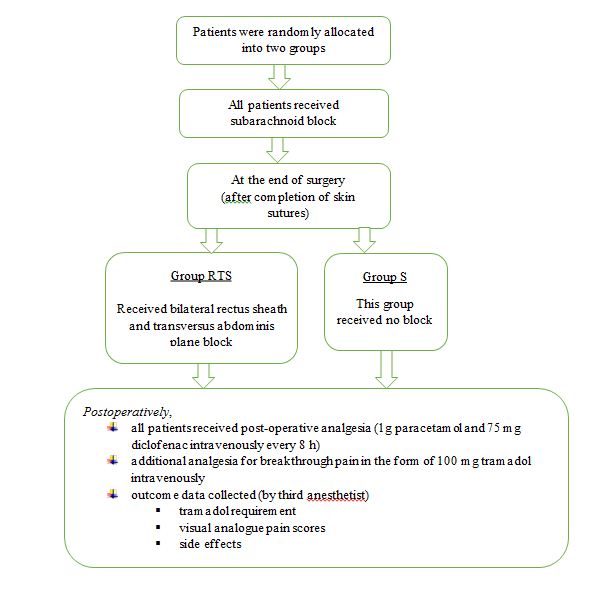
Figure 3: Flow chart of the study
The chief outcome measured in this study was 24 h tramadol requirement. Secondary outcome measures included time to first request for tramadol, visual analogue scores and side effects connected with tramadol consumption.
Discrete categorical data were presented as n (%); continuous data was written as either in the form of its mean and standard deviation or in the form of its median and interquartile range, as per the requirement. The normality of quantitative data was tartan by measures of Kolmogorov-Smirnov tests for normality. For normally distributed (AGE BMI) t-test was applied for statistical analysis of 2 groups. For ordinal data Visual analogue pain scores non parametric Mann-Whitney U-test was used for statistical analysis of 2 groups. For categorical data, comparisons were made by Pearson Chi-square or Fisher’s exact test as appropriate. All the statistical tests were two-sided and were performed at a significance level of α = 0.05. Analysis was conducted using IBM SPSS STATISTICS software (version 22.0). Sample size was estimated based on mean total utilization of tramadol in milligrams at 48 hours as 6.1. To detect a 30% decrease in consumption with standard deviation (SD) of 2.5 our sample size came out to be 28 per group at a power of 80% & confidence interval of 95%. For likely attrition, it was decided to include 30 patients per group.
RESULTS
Sixty parturients undergoing elective or emergency cesarean delivery were included in the study, thirty received ultrasound guided abdominal field blocks and thirty did not.
Groups were similar in terms of age and BMI (Table 1).
In all patients’ transversus abdominis plane and posterior rectus sheath were identified and the blocks were performed without any complication.
Patients in Group RTS had reduced 24 h tramadol requirements (157 ± 50.709 vs 386.67 ± 29.16 mg) and a longer time for additional tramadol request (10.48 ± 1.887 vs 2.88 ± 0.703 h) compared with the Group S at all-time points (Table 1).
Table 1: Postoperative tramadol requirement (mean ± SD)
| Variable | Group RTS
(n=30) |
Group S
(n=30) |
p value |
| Request to first analgesia (h) | 10.48 ± 1.887 | 2.88 ± 0.703 | < 0.001 |
| Total tramadol requirement (mg) | 157.14 ± 50.709 | 386.67 ± 29.16 | < 0.001 |
Postoperative visual analogue pain scores at rest were reduced in Group RTS at all-time points assessed (Table 2).
Table 2: Postoperative visual analogue pain scores at rest – median (interquartile range)
| Group | Group RTS
(n=30) |
Group S
(n=30) |
p-value |
| 2 h | 2 (2.0-2.0) | 8 (7.0-8.25) | < 0.001 |
| 4 h | 2 (2.0-2.25) | 8 (7.0-8.0) | < 0.001 |
| 6 h | 2 (2.0-3.0) | 8 (7.0-8.0) | < 0.001 |
| 12 h | 4 (3.0-4.0) | 7 (7.0-8.0) | < 0.001 |
| 24 h | 4 (3.0-4.0) | 7 (6.75-7.0) | < 0.001 |
No significant difference was found between Group RTS and S in the incidence of nausea. Sedation was reduced in the Group RTS.
DISCUSSION
This randomized, double-blind, controlled study demonstrated that supplementing a standard multi-modal analgesic regimen with rectus sheath and transversus abdominis plane block resulted in reduced 24 h tramadol requirement and pain scores, as well as delayed demand for supplemental opioid analgesia, compared with the standard regimen alone.
Single shot neuraxial analgesic methods utilizing long acting opioids, or epidural opioid administration, create efficient analgesia, but these are associated with a high incidence of side effects, mainly nausea, vomiting and pruritus, which reduce overall patient satisfaction.8 In addition, there is a risk of delayed respiratory depression due to rostral spread of morphine.9 Also it is not always possible to offer neuraxial opioid analgesia due to logistic issues and/or due to medical contraindications.10,11 Even though morphine given through intravenous patient controlled analgesia (IV-PCA) improves patient control, and thereby results in high patient satisfaction levels, the analgesia produced is often incomplete, and opioid-mediated side effects stay common.9 Systemic administered lipophilic opioids such as meperidine have been linked to transfer in breast milk and create transient behavioral effects in the neonate.12 Given these issues; there is substantial potential for regional techniques such as TAP and rectus sheath blockade to include an effective component of a multimodal regimen for post-cesarean delivery analgesia. McDonnell et al. showed that landmark-based TAP block can be used successfully to provide pain relief after cesarean delivery.13
The dose of 0.25% bupivacaine (60 to 80 ml) was relatively high as compared to Bashandy et al.14 who used 40 ml. Our rationale for using a superior dose of local anesthetic stems from our aim to provide prolonged analgesia with a single shot rectus sheath and TAP blocks. Rectus sheath and TAP blocks are advanced level blocks; as significant needle-guidance skills are necessary to safely perform these blocks. Ultrasound guidance makes these blocks simpler and helps in accurate drug placement.
LIMITATIONS
There are a number of limitations to this study. First, the study has inadequate evaluation of postoperative analgesia to the first 24 postoperative hours. Second, there are problems in adequately blinding these type of studies, given that the TAP and rectus sheath block create loss of sensation of the abdominal wall. Although patients and the investigator conducting the postoperative assessments were technically blinded to group allocation, true blinding may not be possible. Third, the study was not large enough to measure safety. There is a risk of inadvertent peritoneal puncture with this block. Although the incidence is not known, if the blocks are performed as described, the danger of peritoneal puncture is low. A further limitation is that we did not measure the success rate of block or the extent of abdominal wall sensory blockade. This was done to preserve blinding of the assessor. Finally, we did not perform a dose-response study to conclude if a lower dose of bupivacaine would lead to the same result. These observations warrant more studies in the future.
CONCLUSION
We conclude that ultrasound guided TAP (posterior injection) and rectus sheath block grasps significant promise as part of a multimodal analgesic regimen for post cesarean delivery analgesia. Ultrasound made rectus sheath and TAP blocks simple to perform, and provided reliable analgesia in this study; no difficulties due to the blocks being detected.
Conflict of interest: None declared.
Sources of funding: Nil.
Authors’ contribution:
VS: Concept of the study, Manuscript Drafting
MB: Data Collection, Manuscript Drafting
KT: Statistical Analysis
REFERENCES
- Villar J, Vallandares E, Wojdyla D, Zavaleta N, Carroli G, Velazaco A, et al. Caesarean delivery rates and pregnancy outcome: The 2005 WHO global survey on maternal and perinatal health in Latin America. Lancet 2006;367:1819-29. [PubMed] [Free full text]
- Liu B, Tong C, Eisenach JC. Pregnancy increases excitability of mechanosensitive afferents innervating the uterine cervix. Anesthesiology 2008;108:1087-92. [PubMed] [Free full text] doi: 10.1097/ALN.0b013e31817302e0.
- Yan T, Liu B, Du D, Eisenach JC, Tong C. Oestrogen amplifies pain responses to uterine cervical distension in rats by altering transient receptor potential-1 function. Anesth Analg 2007;104:1246-50. [PubMed] [Free full text] doi: 10.1213/01.ane.0000263270.39480.a2
- Brierly SM. Molecular basis of mechanosensitivity. Auton Neurosci 2010;153:58-68. [PubMed] [Free full text] doi: 10.1016/j.autneu.2009.07.017
- Woolf CJ; American College of Physicians; American Physiological Society. Pain: moving from symptom control toward mechanism-specific pharmacologic management. Ann Intern Med 2004;140;441-51. [PubMed] [Free full text] DOI: 10.7326/0003-4819-140-8-200404200-00010
- Smith R. Parturition. N Eng J Med 2007;356:271-83. [PubMed] [Free full text] DOI:
- 10.1056/NEJMra061360
- Unal ER, Cierny JT, Roedner C, Newman R, Goetzl L. Maternal inflammation in spontaneous term labor. Am J Obstet Gynecol 2011;204;223-5 [PubMed] [Free full text] doi: 10.1016/j.ajog.2011.01.002.
- Farragher RA, Laffey JG. Postoperative pain management following caesarean section. In: Shorten G, Carr D, Harmon D, et al. Postoperative pain management: an evidence-based guide to practice. 1st ed. Philidelphia PA: Saunders Elsevier, 2006:225-38. [PubMed] [Free full text]
- Dahl JB, Jeppesen IS, Jorgensen H, Wetterslev J, Moiniche S. Intraoperative and postoperative analgesia efficacy and adverse effects of intrathecal opioids in patients undergoing cesarean section with spinal anesthesia: a qualitative and quantitative systemic review of randomized controlled trials. Anesthesiology 1999;91:1919-27 [PubMed] [Free full text]
- Werawatganon T, Charuluxanun S. Patient controlled intravenous opioid analgesia for pain after intra-abdominal surgery. Cochrane Database Syst Rev 2005 Jan 25;(1):CD004088 [PubMed] [Free full text] DOI: 10.1002/14651858.CD004088.pub2
- Fortiadis RJ, Badvie S, Weston MD, Allen-Mersh TG. Epidural analgesia in gastrointestinal surgery. Br J Surg 2004;91:828-41[PubMed] [Free full text]
- Wittels B, Scott DT, Sinatra RS. Exogenous opioids in human breast milk and acute neonatal neurobehavior: a preliminary study. Anesthesiology 1990;73:864-9. [PubMed] [Free full text]
- McDonnell JG, Curley G, Carney J, Benton A, Costello J, Maharaj CH, Laffey JG. The analgesic efficacy of transversus abdominis plane block after caesarean delivery: A randomized controlled trial. Obstetric Anesthesiology 2008;106:186-191. [PubMed] [Free full text] doi: 10.1213/01.ane.0000290294.64090.f3.
- Bashandy GMN, Elkholy AHH. Reducing postoperative opioid consumption by adding an ultrasound guided rectus sheath block to multimodal analgesia for abdominal cancer surgery with midline incision. Anesth Pain Med. 2014 August;4(3):e18263. [PubMed] [Free full text] DOI: 10.5812/aapm.18263.

