Shiv Kumar Singh
Consultant Anaesthesia, Department of Anaesthesia, Royal Liverpool University Hospitals, Liverpool, (UK)
Correspondence: Dr. Shiv Kumar Singh, Consultant Anaesthesia, Department of Anaesthesia, Royal Liverpool University Hospitals, 11th Floor Prescot Street, Liverpool L7 8XP, (UK); E-mail: Shiv.singh@rlbuht.nhs.uk
ABSTRACT
Cervical plexus has a complex anatomy and is considered as a plexus of loops. It is often described as deep and superficial cervical plexus. The deep plexus provides the muscular branches and the superficial plexus provides the innervation of the skin of the head and neck. Ultrasound guided blocks for cervical plexus are fairly new entrant and are easier to understand with knowledge of the landmark techniques that are briefly described in this article. The superficial and intermediate plexus blocks are fairly easy to perform. The deep plexus block is described in various forms, from extension of brachial plexus block, injection around the carotid and lastly the classical deep cervical plexus block. The C4 transverse process is the key to performing the deep plexus block and in this article we, for the first time, describe the “thumbs up” sign that helps to easily identify C4 level and perform this block. The article also describes the complications that can be expected with these blocks and how they can be avoided.
Key words: Carotid endarterectomy; Endarterectomy; Vascular Surgical Procedures; Nerve Block; Anesthesia, Local; Cervical plexus block; Ultrasound; Ultrasonography; Ultrasound Imaging; Ultrasonography, Interventional
Citation: Singh SK, The cervical plexus: anatomy and ultrasound guided blocks. Anaesth Pain & Intensive Care 2015;19(3):323-332
INTRODUCTION
Carotid endarterectomy still remains the commonest indication for cervical plexus block. Other than carotid endarterectomy there are many other procedures on the neck where this block can be utilised, including procedures on the neck region like internal jugular venous cannulation, lymph node biopsies, thyroid and parathyroid surgeries. The block is also finding its place in the emergency department for simple procedures for soft tissue and bone injuries such as injuries to the ear, neck and clavicular region including fractures and dislocations. Recently use of this block has also been described for cervicogenic headaches. There are three main approaches to this block, and the blocks can be done using landmark techniques alone. More recently use of ultrasound has been described for performing these blocks. Deep cervical block has been associated with some serious complications; so superficial cervical plexus block is often thought to be sufficient for most procedures on the neck region. Bilateral deep cervical plexus blocks should never be performed but bilateral superficial cervical blocks can be safely performed for surgeries or for postoperative analgesia. In this article we describe the anatomy of the cervical plexus, indications for the blocks and how the blocks can be performed using landmark techniques and ultrasound guidance. We also describe the complications associated with these blocks and how they should be managed.
CERVICAL PLEXUS ANATOMY
The cervical plexus is formed by the ventral rami of the upper four cervical (C1-C4) nerves. The rami emerge between the anterior and posterior tubercles of the transverse processes of the cervical vertebrae, creating a groove on the costotransverse bars (Figure 1). The four roots forming the plexus connect to each other to form three loops.
The plexus is related posteriorly to the muscles that arise from the posterior tubercle of the transverse process i.e. the levator scapulae and scalenus medius; and anteriorly, to the prevertebral fascia, the internal jugular vein and the sternocleidomastoid.1,2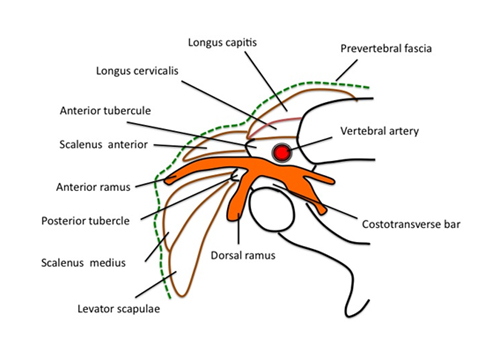
Figure 1: The primary rami of the cervical roots lying on the costo transverse bar between the anterior and posterior tubercle
The branches of the superficial cervical plexus innervate the skin and superficial structures of the head, neck and shoulder. The deep branches of the cervical plexus innervate the deeper structures of the neck, including the muscles of the anterior neck and the diaphragm (phrenic nerve). The third and fourth cervical nerves typically send a branch to the spinal accessory nerve, or directly into the deep surface of the trapezius to supply sensory fibres to this muscle. The fourth cervical nerve may send a branch downward to join the fifth cervical nerve and participate in the formation of the brachial plexus (pre-fix).
FORMATION OF CERVICAL PLEXUS
The upper four cervical nerves unite by a series of loops to form the cervical plexus. The loops are three in numbers, C1-2, C2-3, C3-4, with a further loop (C4-5) often present to connect the cervical plexus with the brachial plexus.
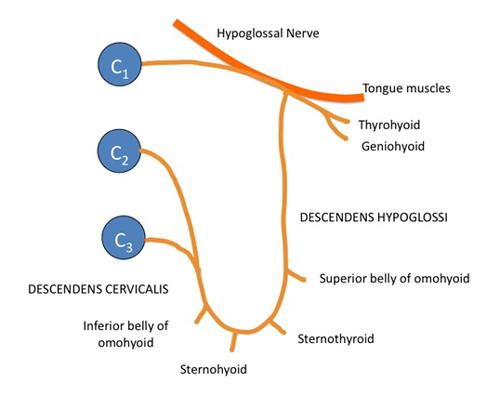
The anterior primary ramus of C1 is entirely motor. The nerve descends to form a loop with the ascending branch of C2 in front of the transverse process of the atlas. The majority of the fibres in this loop run forward to join the hypoglossal nerve (XII CN) and through this, C1 supplies the geniohyoid and thyrohyoid muscles, then runs downwards as the descendens hypoglossi, from which the nerve to the superior belly of the omohyoid muscle is derived (Figure 2).
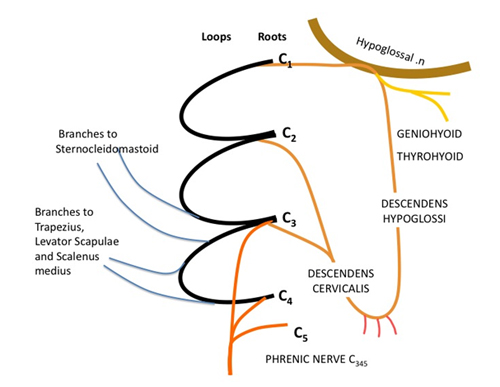
Figure 2: Formation of the ansa cervicalis by the descendens hypoglossi and descendens cervicalis and the motor branches (modified from Ellis and Feldman)
Descendens hypoglossi joins descendens cervicalis, derived from C2 and 3, to form a loop termed the ansa cervicalis, which lies on the carotid sheath. From the ansa, nerve fibres pass to supply sternohyoid, sternothyroid and the inferior belly of omohyoid (Figure 3).
Figure 3: The ansa cervicalis and its branches to the strap muscles of the neck (modified from Ellis and Feldman)
The anterior primary ramus of C2 divides into an ascending branch, which joins C1, and a descending branch, which loops to join C3 (Loop 2). Loop 3 is formed by the anterior primary ramus of C3 and C4. Branches from this loop join C5 to give rise to the phrenic nerve (Figure 2).
Each root also receives a grey ramus communicans from the superior cervical ganglion.
Summary of the Branches of Cervical Plexus
The branches of the cervical plexus can be divided into four groups.
- Communicating branches:
- Grey rami pass from superior cervical ganglion to the roots of C1-4 nerves.
- Branch from C1 that joins the hypoglossal nerve
- Branch from C2 to sternocleidomastoid and
- Branches from C3 and 4 to the spinal accessory nerve which supplies the trapezius muscle
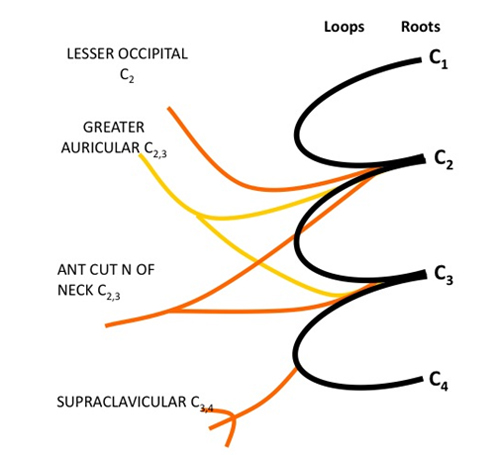
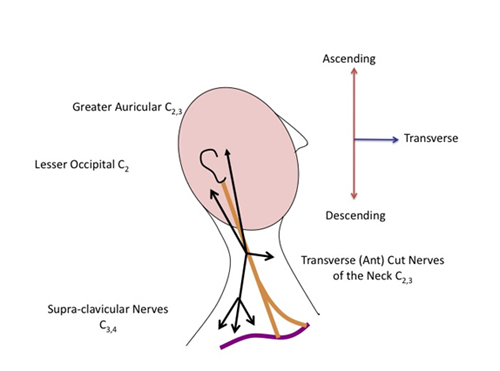
- Superficial (cutaneous) branches, which supply cutaneous fibres to the neck (Figure 4 and 5).
- Ascending branches; Lesser occipital (C2) and Greater auricular (C2,3)
- Transverse branch; Transverse (anterior) cutaneous nerve of the neck (C2,3)
- Descending branches; Supraclavicular (C3,4)
- Deep branches, to the neck muscles.
- The phrenic nerve, which is the motor nerve of the diaphragm
Figure 4: Superficial branches of the cervical plexus
Figure 5: Schematic of the superficial branches of the cervical plexus and their distribution
INDICATIONS FOR CERVICAL PLEXUS BLOCK
The cervical plexus block provides anesthesia and analgesia to the head and neck region. Depending on the type of surgery, the plexus can be blocked either at a superficial or a deep level or both. The superficial branches of the plexus innervate the skin and superficial structures of the head, neck, and shoulder. The deep branches innervate the muscles of the deep anterior neck and the diaphragm.
Carotid endarterectomy still remains the commonest indication for the cervical plexus block, with anaesthetists performing it under superficial or intermediate plexus block alone and some may prefer to do it under combined superficial and deep cervical plexus block.3-8
The deep cervical plexus block can also be used for deeper surgeries of the head and neck, such as vocal cord surgeries, dental abscess, lymph node dissections and plastic repairs.9,10
Cervical plexus block is often a side effect of the interscalene approach ( with large volumes) to the brachial plexus, that is used as an advantage for shoulder surgery but in cases where supra or infra-clavicular approach are used in order to avoid phrenic nerve block, these blocks can be supplemented with superficial cervical plexus block for complete analgesia for shoulder surgeries.11,12
Bilateral blocks (superficial) can be used for thyroid and parathyroid surgeries. These blocks have been used as sole anaesthetics in high-risk patient under monitored anesthesia care (MAC) as well as for post-op analgesia.13-15
Unilateral superficial cervical blocks are underutilised, they provide anesthesia not only to the neck but also to the subcutaneous tissue over the clavicle (via supraclavicular nerves). The block can be utilised for central venous cannulation via the internal jugular or subclavian routes.16
Superficial cervical plexus block can also be safely used in the emergency departments for soft tissue and bony injuries such as injuries to the ear, neck and clavicular region including clavicular fractures and acromioclavicular dislocations.17
Recently, deep cervical plexus block has also been described for management of cervicogenic headaches; the block helps in differentiating it from headaches due to migraine.18
APPROACHES TO CERVICAL PLEXUS BLOCKS
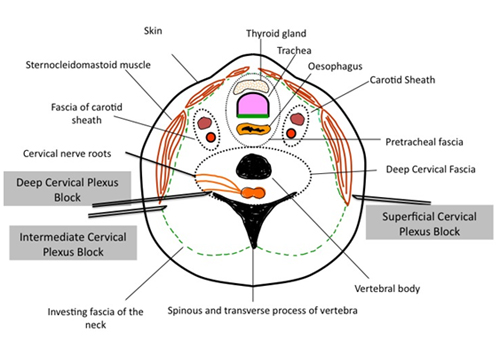
In 2004, following a cadaveric study by Pandit and colleagues,22 Telford and Stoneham proposed a nomenclature for the cervical plexus blocks.19 The ‘superficial cervical plexus’ block consists of a subcutaneous injection of local anesthetic (LA) just under the skin. Next is what is termed an ‘intermediate’ or ‘subfascial’ block as suggested by Pandit and colleagues, which is somewhat a deeper injection under the investing fascia of the neck. The ‘deep cervical plexus’ block is the deepest injection and involves deposition of LA beneath the deep cervical fascia (i.e. close to the transverse processes of the cervical vertebrae), and it can be performed either as a single or as multiple injections technique.
Basis of Cervical Plexus Blocks
To understand the basis of the various approaches to cervical plexus blocks it is important to understand the classical approaches to these blocks and the landmarks used. The various approaches to the cervical plexus are described in a schematic diagram in Figure -7.
SUPERFICIAL CERVICAL PLEXUS BLOCK
Murphy20 and Scott21 described the classical technique of superficial cervical plexus block, which involves subcutaneous (superficial) injection of LA. This block can also be considered as a field block and is often performed using a large volume of LA.
DEEP CERVICAL PLEXUS BLOCK
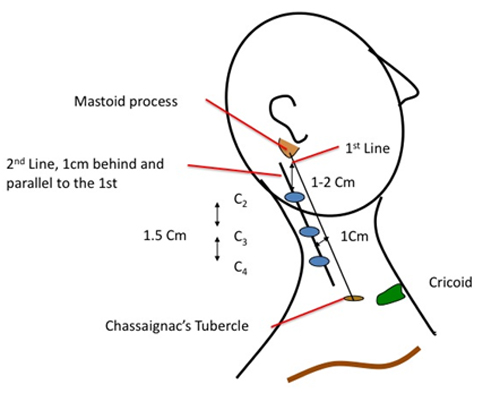
Deep cervical plexus block is a complex regional technique. This technique involves blocking the nerve roots of C2, C3 and C4. The roots of cervical nerves 1 to 7 emerge superior to the transverse process of each cervical vertebra. In an adult, the larynx overlies cervical vertebrae 4 to 6. The upper border of the larynx (C4) is palpable as the notch in the thyroid cartilage. The lower border of the larynx (C6) is the cricoid cartilage. The external jugular vein often crosses the posterior border of the sternocleidomastoid muscle at the level of C6.
There are two methods by which deep cervical plexus can be blocked. The first method involves three injections at C2, C3 and C4; and in the second method a single injection is done at the C4 level.
The Classical Approach:
With the patients’ head turned to the contra-lateral side, a line is drawn from tip of mastoid process to transverse process of C6 (Chassaignac’s tubercle). A second line is then drawn 1 cm posterior and parallel to the first line. The transverse process of C2 is located 1-2 cm caudal to the mastoid process on this second line. The transverse processes of C3, and C4 are at a distance of 1.5 cm from C2 and from each other (Figure 6).
After drawing out the positions of the transverse processes, the neck is prepared using anti-septic solution and draped. Using a 22G, 1.5 inch (4 cm) needle, the transverse processes are located by entering perpendicular to the skin. The depth of the transverse process varies with the body habitus of the patient (1.5-3.0 cm deep). Once bone is contacted, the needle is pulled back slightly, and directed in the cephalad direction. This is repeated until the needle is walked off the bone. Moving cephalad will help ensure that the needle is close to the desired nerve root. It is important to only walk off the bone a millimeter or two at a time, because going any further can result in entering the subarachnoid space or the vertebral artery. After careful aspiration for blood and/or CSF, 5 ml of LA is injected slowly; elicitation of paresthesia, as sought by some is not necessary for the block. The needle should be withdrawn before injection of the LA, if paresthesia is obtained. This is repeated at the other two transverse processes. During injection, verbal contact should be maintained continuously throughout the procedure, to help detect a change in mental status that could occur with the intravascular injection.
Figure 6: Deep cervical plexus block using the classical approach, the landmarks are described in this schematic diagram.
INTERMEDIATE CERVICAL PLEXUS BLOCK
Pandit and colleagues in their cadaveric study demonstrated that injections placed below the investing fascia of the neck diffuse into the deep space, whereas injections placed subcutaneously did not. They termed the injection deep to the investing layer of the neck as the ‘intermediate’ cervical plexus block.22
For the intermediate block, after the usual skin preparation with anti-septic, the needle is inserted in a perpendicular plane at the midpoint of the posterior border of the sternocleidomastoid muscle until a ‘loss of resistance’ or ‘pop’ is felt as the needle passed through the investing layer of the cervical fascia (at ????1–2 cm depth). The needle is then fixed and around 15-20 ml of LA is slowly injected after careful aspiration. It is our personal observation that in most patients if the LA is in the right plane a longitudinal swelling just behind the posterior border of the sternocleidomastoid can be noticed. Some anesthetists like to use ‘fanning’ of the injectate but this should be avoided to reduce the chance of inadvertent intravascular injections.
Nash and colleagues 23 have disputed the presence of the investing fascia in their study using a combination of dissection, E12 sheet plastination (a technique or process used in anatomy to preserve bodies or body parts. The water and fat are replaced by certain plastics, yielding specimens that can be touched, do not smell or decay, and even retain most properties of the original sample), and confocal microscopy in 10 adult human cadavers. They concluded that the so-called investing cervical fascia does not exist in the anterior triangle of the neck.
Ramachandran and colleagues in their very recent study compared intermediate and superficial cervical plexus block and concluded that both, the superficial and intermediate cervical plexus blocks are equally effective for carotid endarterectomy surgery.24
Figure 7: The three described techniques for the cervical plexus block (modified from Pandit et al)
ULTRASOUND GUIDED CERVICAL PLEXUS BLOCK
Ultrasound can be confidently used for performing the superficial cervical plexus block but experience with ultrasound-guided deep cervical plexus is still in its infancy and not well described in the literature. The cervical plexus blocks are normally performed in supine or semi-recumbent position with the patients’ head turned to the contra-lateral side (Figure 8).
Figure 8: The patient lies in a supine or semi-recumbent position with head turned to the contra-lateral side for cervical plexus blocks.
Superficial Cervical Plexus Block
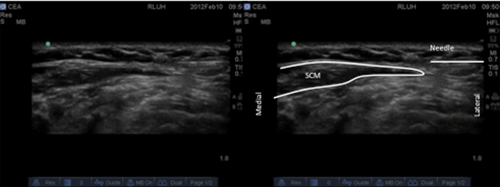
Ultrasound guided superficial plexus block is not only easy but may also increases the success rate on one hand and on the other, avoids too deep needle insertion and/or inadvertent injections into the important surrounding structures in the neck.17 Even though landmark based block is easy, the advantage of ultrasound lies in its ability to ensure the spread of LA in the correct plane.
The block is normally performed in supine or semi-recumbent position with the patients’ head turned to the contra-lateral side. Once the skin is appropriately cleaned and prepared with anti-septic, the transducer is placed over the lateral side of the neck at the midpoint of the posterior border of the sternocleidomastoid muscle (SCM). The transducer is positioned such that the tapering end (posterior border on the ultrasound image) of the SCM is in the centre of the screen (Figure 9). The needle is then introduced from the posterior aspect through the skin and platysma and 5-10 ml of LA deposited just behind this landmark. The LA can be seen spreading along the post border of the SCM and this can be visualized by placing the probe transversely along the post border of the SCM or alternatively, LA can be injected using long axis, in-plane approach by keeping the probe in transverse position. This will involve two injections, starting from mid-point of SCM, one from caudal to cranial end and the second one from cranial to caudal end.
Figure 9: Superficial cervical plexus block, subcutaneous injection at the posterior border of the sternocleidomastoid, the needle can be seen approaching from the right (lateral) side of the screen.
Deep Cervical Plexus Block
As mentioned earlier, the literature is sparse in relation to this block and various descriptions exist in the literature. This may be due to the fact that most of the surgeries can be accomplished with either superficial or intermediate cervical plexus blocks without going into the complexity of the deep block and its associated complications.
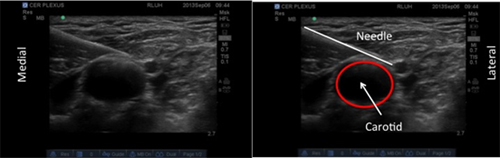
Deep Cervical Plexus: Approach-1:
The first approach takes a very simple view, in this approach LA is deposited just behind the carotid sheath at the level of the carotid bifurcation (Figure 10). The injection is not as deep as described for classical deep cervical plexus block. Even though there are no publications based on this approach, combined with superficial plexus block, this might work very well. The advantage of this approach is the simplicity and safety. It is important to visualize the needle tip through out the procedure and aspirate before each injection so that intra-vascular injection into the carotid or the internal jugular can be avoided.
Figure 10: Deep cervical plexus block, LA is deposited behind the carotid sheath
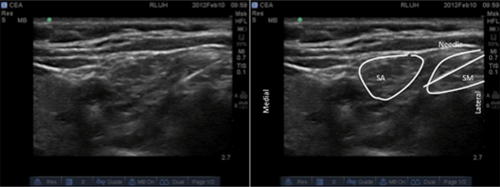
Deep Cervical Plexus: Approach-2:
The second approach uses the findings of Winnie and colleagues.25 They suggested following the interscalene groove cranially and depositing the LA anesthetic in this groove (Figure 11). For those who regularly perform interscalene brachial plexus block, this is a logical approach, as we all know that the cervical plexus is blocked when LA overspills and this is used to its advantage for the shoulder surgeries.
Figure 11: Ultrasound approach based on Winnie’s description, LA is deposited between the scalenus anterior (SA) and medius (SM) at C4 level.
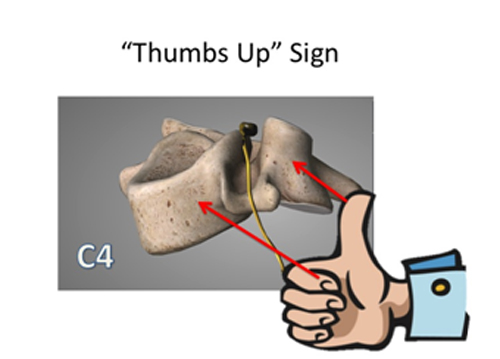
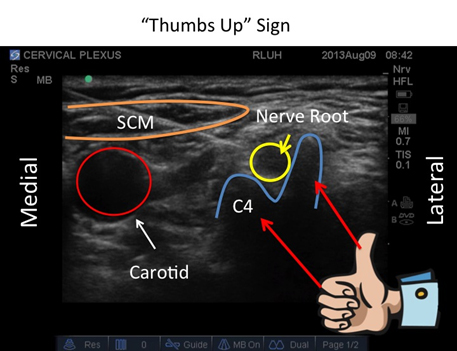
Deep Cervical Plexus: Approach-3, ‘Thumbs Up’ Sign:
The last approach follows the classical description of deep cervical plexus block. In this technique the C4 level is marked and the transducer is placed laterally at this point and moved posteriorly till the transverse process of C4 is identified.
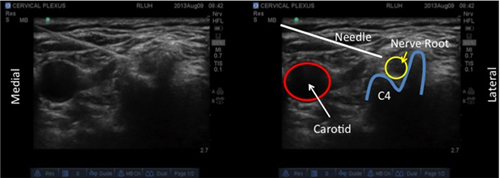
The appearance of C4 transverse process is typical and we describe it as ‘Thumbs Up’ Sign, with the thumb facing the carotid artery (this is the 1st ever description of this sign for this block) (Figures 12 & 13). Since the posterior tubercle of the C4 transverse process is large (Thumb like), it is difficult to introduce the needle and reach the nerve root from the lateral side of the neck. The needle is therefore, introduced from medial side, in the long axis, under direct vision. Once the tip of the needle is in close proximity of the post tubercle or the nerve root, after aspiration, 10-15 ml of LA is injected (Figure 14).
Usi et al26 and Choquet et al27 in their articles suggest that it is possible to block the cervical plexus under ultrasound guidance by injecting LA in the deep cervical space without specifically targeting the nerve roots.
Figure 12: The C4 vertebrae and the “Thumbs Up” Sign. The C4 nerve root can also be easily visualized at this level on the US scan
Figure 13: The structures seen at the C4 level and the creation of the “Thumbs Up” Sign by the post tubercle and the vertebral body of C4
Figure 14: The needle is approached from the medial side to reach the post tubercle of C4 (the thumb). The nerve root can be easily visualized at this level.
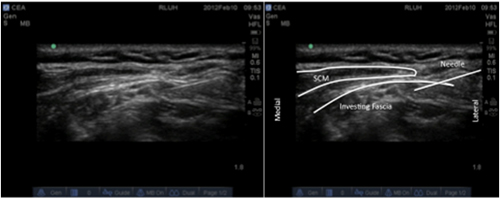
Intermediate Cervical Plexus Block
This approach can also be done under ultrasound guidance. 27 The approach is similar to superficial cervical plexus block but involves deeper injection. An attempt is made to identify the investing fascia of the neck in the interscalene groove and LA deposited under the fascia (Figure 15). A click or “pop” can often be felt when the needle pierces this fascia, 10-15 mls of LA is deposited at this level.
Figure 15: The intermediate approach to the cervical plexus, the investing fascia can be easily identified and LA deposited under the fascia.
COMPLICATIONS OF CERVICAL PLEXUS BLOCKS
Several complications can occur during the conduct of cervical plexus block, more so with deep than superficial cervical plexus blocks. These complications can be minimized by proper knowledge of the physiology of the block and the toxicity of LA.28
Superficial cervical plexus block is associated with the usual general complications that are associated with any nerve block done using LA; intravascular injection into a vein or artery, hematoma, infection and LA toxicity.
Deep cervical plexus block is associated with more serious complications, most important of which is accidental intravascular injection into the vertebral artery. The vertebral artery lies in the vertebral canal, which is only about 0.5 cm below the tip of the transverse process, the landmark where the LA is deposited for the deep cervical plexus block. Since the vertebral artery has direct supply to the brain, injection of a very small amount of LA can cause CNS effects as it is directly delivered to the brain. It is, therefore, important, to maintain constant verbal contact with the patient during injection to help detect early signs of CNS toxicity, such as perioral numbness, disorientation or tinnitus. Aspiration should be done frequently. If injection is performed slowly, and verbal contact with the patient is maintained, progression of toxicity from CNS to cardiac is very unlikely.28
The next dreaded complication of the deep cervical plexus block is subdural injection. If the needle is placed too far, a dural sleeve around the nerve root may be entered. LA injection in this situation can result in a subarachnoid block, which can lead to unconsciousness and hypotension. Endotracheal intubation, respiratory and cardio-vascular support may become necessary in this situation.28
The cervical plexus lie in close proximity to large vessels in the neck and occasionally large haematoma may occur following an accidental puncture of these vessels. If recognised early, local compression should alleviate this problem, if left unrecognised in rare situations this can cause compromise of the airways.28 Airway compromise from cervical plexus block secondary to bilateral recurrent laryngeal nerve palsy affecting the vocal cords, though rare can occur from the LA spread.29
Not a complication but a side effect of the deep cervical plexus block is the phrenic nerve palsy and this should be expected as the nerve originates in the cervical plexus from the 3, 4 and 5th cervical nerve roots. This does not present as much of a problem in healthy individuals but in patients with severe pulmonary disease and those who are dependent of adequate diaphragmatic excursions for adequate respiratory function, this may not be desirable and the block should be avoided.30
SUMMARY
Cervical plexus blocks are simple to learn and the indications for them are expanding as we learn more about the applications of these blocks. Carotid endarterectomy still remains the commonest indication for this block, but in the recent past these blocks have been utilised by the emergency department and the chronic pain physicians. Most people tend to use landmark techniques but with the recent advances, these blocks can be done under ultrasound guidance. In this review we described the anatomy of the cervical plexus, the indications and the various approaches to the cervical plexus using the landmark and under ultrasound guidance. This will provide confidence for people to utilise these blocks more widely in their clinical practice.
REFERENCES
- J. A. Gosling, P. F. Harris, I. Whitmore, and P. L. T. Willan. “Posterior triangle of the neck” in Human Anatomy: Color Atlas and Text, p. 288-89, Elsevier Science, 4th edition, 2002.
- H. Ellis, S.Feldman, W. Harrop Griffiths, “The spinal nerves” in Anatomy for Anaesthetist, p. 146-153, Blackwell Publishing, 8th edition, 2004
- Davies MJ, Silbert BS, Scott DA, Cook RJ, Mooney PH, Blyth C. Superficial and deep cervical plexus block for carotid artery surgery: A prospective study of 1000 blocks. Reg Anesth 1997;22(5):442-6. [PubMed]
- Pandit JJ, Bree S, Dillon P, Elcock D, McLaren ID, Crider B. A comparison of superficial versus combined (superficial and deep) cervical plexus block for carotid endarterectomy: a prospective, randomized study. Anesth Analg 2000;91(4):781-6. [PubMed]
- Stoneham MD, Doyle AR, Knighton JD, Dorje P, Stanley JC. Prospective, randomized comparison of deep or superficial cervical plexus block for carotid endarterectomy surgery. Anesthesiology 1998;89(4):907-12. [PubMed]
- Howell SJ. Carotid endarterectomy. Br J Anaesth 2007;99(1):119-31. [PubMed]
- GALA Trial Collaborative Group, Lewis SC, Warlow CP, Bodenham AR, Colam B, Rothwell PM, et al. General anaesthesia versus local anaesthesia for carotid surgery (GALA): a multicentre, randomised controlled trial. Lancet 2008;372:2132-42. [PubMed] doi: 10.1016/S0140-6736(08)61699-2.
- McCleary AJ, Maritati G, Gough MJ. Carotid endarterectomy; local or general anaesthesia? Eur J Vasc Endovasc Surg 2001;22(1):1-12. [PubMed] DOI: http://dx.doi.org/10.1053/ejvs.2001.1382
- Suresh S, Templeton L. Superficial cervical plexus block for vocal cord surgery in an awake pediatric patient. Anesth Analg 2004;98(6):1656-7. [PubMed]
- Ling KU, Hasan MS, Ha KO, Wang CY. Superficial cervical plexus block combined with auriculotemporal nerve block for drainage of dental abscess in adults with difficult airways. Anaesth Intensive Care 2009;37(1):124-6. [PubMed]
- Halaszynski TM. Ultrasound brachial plexus anesthesia and analgesia for upper extremity surgery: essentials of our current understanding. Curr Opin Anaesthesiol 2011;24:581-91. [PubMed] doi: 10.1097/ACO.0b013e32834aca03.
- Koscielniak-Nielsen ZJ, Frederiksen BS, Rasmussen H, Hesselbjerg L. A comparison of ultrasound-guided supraclavicular and infraclavicular blocks for upper extremity surgery. Acta Anaesthesiol Scand 2009;53(5):620-6. [PubMed] doi: 10.1111/j.1399-6576.2009.01909.x.
- Aunac S, Carlier M, Singelyn F, De Kock M. The analgesic efficacy of bilateral combined superficial and deep cervical plexus block administered before thyroid surgery under general anesthesia. Anesth Analg 2002;95:746-50. [PubMed]
- Lo Gerfo P, Ditkoff BA, Chabot J, Feind C. Thyroid surgery using monitored anesthesia care: an alternative to general anesthesia. Thyroid 1994;4:437-9. [PubMed]
- Kulkarni RS, Braverman LE, Patwardhan NA. Bilateral cervical plexus block for thyroidectomy and parathyroidectomy in healthy and high risk patients. J Endocrinol Invest 1996;19(11):714-8. [PubMed]
- Chauhan S, Baronia AK, Maheshwari A, Pant KC, Kaushik S. Superficial cervical plexus block for internal jugular and subclavian venous cannulation in awake patients. Reg Anesth 1995;20(5):459. [PubMed]
- Herring AA, Stone MB, Frenkel O, Chipman A, Nagdev AD. The ultrasound-guided superficial cervical plexus block for anesthesia and analgesia in emergency care settings. 2012 Sep;30(7):1263-7. [PubMed] doi: 10.1016/j.ajem.2011.06.023
- Goldberg ME, Schwartzman RJ, Domsky R. Deep cervical plexus block for the treatment of cervicogenic headache. Pain Physician 2008;11(6):849–54. [PubMed] [Free full text]
- Telford RJ, Stoneham MD, Correct nomenclature of superficial cervical plexus blocks. Br J Anaesth 2004;92:775-6. [PubMed][Free full text] doi: 10.1093/bja/78.6.775
- Murphy TM. Somatic blockade of head and neck. In: Cousins MJ, Bridenbaugh PO, eds. Neural Blockade in Clinical Anaesthesia and Management of Pain. Philadelphia: Lippincott Company, 1988; 533-58
- Scott DB. Cervical plexus block. In: Scott DB. Techniques of Regional Anaesthesia. Norwalk: Appleton & Lange, 1989; 74-7
- Pandit JJ, Dutta D, Morris JF. Spread of injectate with superficial cervical plexus block in humans: an anatomical study. Br J Anaesth 2003;91(5):733-5. [PubMed][Free full text] doi: 10.1093/bja/aeg250
- Nash L, Nicholson HD, Zhang M. Does the investing layer of the deep cervical fascia exist? Anesthesiology 2005;103(5):962-8. [PubMed]
- Ramachandran SK, Picton P, Shanks A, Dorje P, and Pandit JJ. Comparison of intermediate vs subcutaneous cervical plexus block for carotid endarterectomy. Br J Anaesth 2011;107(2):157-63. [PubMed][Free full text] doi: 10.1093/bja/aer118
- Winnie AP, Ramamurthy S, Durrani Z, Radonjic R. Interscalene cervical plexus block: a single-injection technique. Anesth Analg 1975;54(3):370-5. [PubMed]
- Usui Y, Kobayashi T, Kakinuma H, Watanabe K, Kitajima T, Matsuno K. An anatomical basis for blocking of the deep cervical plexus and cervical sympathetic tract using an ultrasound-guided technique. Anesth Analg 2010;110(3):964–8. [PubMed] doi: 10.1213/ANE.0b013e3181c91ea0.
- Choquet O, Dadure C, Capdevila X. Ultrasound guided deep or intermediate cervical plexus block: the target should be the posterior cervical space. Anesth Analg 2010;111(6):1563-4. [PubMed] doi: 10.1213/ANE.0b013e3181f1d48f.
- Pandit JJ, Satya-Krishna R, Gration P. Superficial or deep cervical plexus block for carotid endarterectomy: a systematic review of complications. Br J Anaesth 2007;99(2):159-69. [PubMed][Free full text] doi: 10.1093/bja/aem160
- Kwok AO, Silbert BS, Allen KJ, Bray PJ, Vidovich J. Bilateral vocal cord palsy during carotid endarterectomy under cervical plexus block. Anesth Analg 2006;102(2):376–7. [PubMed]
- Castresana MR, Masters RD, Castresana EJ, Stefansson S, Shaker IJ, Newman WH. Incidence and clinical significance of hemidiaphragmatic paresis in patients undergoing carotid endarterectomy during cervical plexus block anesthesia. J Neurosurg Anesthesiol 1994;6:21–3. [PubMed]