Gauhar Afshan, FCPS*, Khalid Bashir, MCPS, FCPS**
*Professor & Chair, Department of Anaesthesiology, Aga Khan University, Karachi (Pakistan)
**Professor & Head, Department of Anesthesiology, Postgraduate Medical Institute & Ameeruddin Medical College, Lahore (Pakistan)
Correspondence: Dr. Gauhar Afshan, Professor, Department of Anesthesiology, Aga Khan University, Karachi (Pakistan); E-mail: gauhar.afshan@aku.edu
SUMMARY
This review attempts to address the current pharmacological treatment strategies in children. Irrespective of the type of cancer ‘Pain’ is among the three most frequently reported symptoms and in 40% of children it is under treated. Cancer pain is a complex pain and various mechanisms are responsible for it. Self-reporting or behavioral observational scales are commonly used methods for pain assessment. In current practice, the two-step approach is considered an effective strategy for the pharmacological treatment of pain in children with cancer. For mild pain, paracetomol and ibuprofen are considered as first options in children older than 3 months. For moderate to severe pain, opioid analgesics should be considered and morphine is the drug of choice. It is strongly recommended that analgesics should be administered on a regular basis rather than on an “as required basis” via the most effective, simplest and least painful route. Authors highly recommend the most recent WHO guidelines for two-step strategy using common analgesics regimen in children for cancer pain.
Key words: Cancer pain; Children; Pain assessment; Paracetamol; Morphine; WHO pain guidelines
Citation: Afshan G, Bashir K. Cancer pain in children: a two-step strategy. Anaesth Pain & Intensive Care 2014;18(1):106-110
INTRODUCTION
Pain relief in children has always been neglected due to the fact that children’s pain is often not recognized and it is difficult to assess. However, in the past two decades, it has now been globally recognized as a public health problem of major concern at all three levels of health care: tertiary, secondary and primary.
Cancer is a significant cause of persistent pain in children. Its treatment is often complex and requires holistic approach. This review attempts to address the current treatment strategies in children suffering from pain due to cancer itself and the treatment required for cancer. The prevalence, pathophysiology and preventive as well as management strategies are discussed.
PREVALENCE
Cancer in children is less common as compare with adults. In children, cancers usually occur suddenly, without any early symptoms and have a high rate of cure. The most common (about one-third) cancer in children is leukemia. The other common cancers are brain tumors e.g. gliomas and medullo-blastoma. The less common cancers are neuroblastomas, Wilm’s tumors and sarcomas while lymphomas are rare tumors in children.1
Irrespective of the type of cancer, cancer pain is among the three most frequently reported symptoms i.e. physical fatigue 86%, reduced mobility 76% and pain at 73%. Despite the availability of several guidelines for cancer pain management, (WHO & Agency for Health Care Policy & Research) under treatment, rather inadequate treatment is well documented and is up to 40%.2
CAUSES OF CANCER PAIN
Cancer pain in children shares many etiological factors that are present in adult patients. When cancer is diagnosed at early stages, then children usually experience pain due to diagnostic and therapeutic procedures and treatment. However, at an advanced stage children can’t access chemotherapy or radiotherapy, therefore the pain is usually due to the progression of cancer itself.
Cancer pain is a complex pain and various pathophysiological mechanisms are responsible for it. The acute cancer pain is caused by direct invasion of body tissues by the tumor causing pain due to pressure, distension, inflammation, obstruction and nervous tissue compression. Metastatic spinal cord compression may be a cause of acute back pain and metastatic brain tumor can cause severe headaches.
Chronic pain can either be caused by the tumor growth itself and can cause diffuse bone and joint pain or neuropathic pain. It may also be related to various cancer-related procedures e.g. amputation or chemotherapy.3
PAIN ASSESSMENT TOOLS
Assessment and continual reassessment of cancer pain is an essential component of cancer pain management in children. An assessment of pain intensity and character in children is very difficult as compared to adults. It is usually performed by the following two methods;3
- Self-reporting
- Use of behavioral observational scales (for those who are unable to perform self-reporting)
Self-reporting depends upon the cognitive ability of the child to understand that pain severity to be measured along a continuum. Children between 3 to 8 years of age are capable of quantifying their pain by using visual analog pain scales (a series of faces showing the severity of pain. In older children between 8 to 11 years of age) visual analog scale that rates the intensity of pain on a horizontal or numeric scale (0 to 10) is used.4 Adolescents can rate their pain using a numerical rating scale. In addition other components of pain can also be assessed e.g. description of pain, radiation and other related features.5
In children, who are unable to talk, pain reporting is usually dependent on their parents, who know their child’s behavioral response to pain. Some observational tools are also used to assess pain in this group. These tools are based upon scoring facial expressions, ability to be consoled, the level of interaction, limb and trunk motor responses, and verbal responses.6,7 These are following:
- Revised Face, Legs, Activity, Cry, Consolability (r-FLACC) tool
- Non-Communicating Children’s Pain Checklist – Postoperative Version (NCCPC-PV)
- Pediatric Pain Profile
Observational assessment may underestimate pain severity compared to self-reporting and it is interesting to note that no tool can be recommended over another (does it mean that no reliable, authentic tool could be devised up till now?).
PAIN MANAGEMENT STRATEGIES
Pain management goals should be realistically determined as unrealistic goals may result in disappointment in children or parents. Complete pain relief is not always possible; however, improvement in the quality of life is possible in the majority of children. The main goal of pain management in children is to reduce, control, and prevent pain. Adequate pain control help improving the quality of life, e.g. mobility/ambulation, emotion and self-care in children with cancer.
BASIC PRINCIPLES OF PHARMACOLOGICAL TREATMENT
Although pharmacological treatment should be tailored to the individual child according to the results of assessment and reassessment, the correct use of pain relieving drugs should be based on the following key principles;
• Using a two-step strategy
• Dosing at regular intervals
• Using the appropriate route of administration
• Adapting treatment to the individual child
The last three principles, mentioned in the list above, were introduced by WHO in 1986 as “three-step ladder of pain relief” as ‘by the clock’, ‘by the mouth’ and ‘by the individual’. This three-step ladder has been abandoned now for children in favor of a two-step approach. Currently, it is recommended to use the analgesic treatment in two steps according to the child’s level of pain severity.8
Two-Step Strategy:
The two-step strategy considers the use of low doses of strong opioid for the moderate pain in contrast to the three-step conventional ladder that recommends the use of codeine or tramadol (weak opioid) for the treatment of moderate pain. The risks associated with strong opioids in a low dose are acceptable when compared with the unrelieved pain associated with the codeine and tramadol in children.9
In current practice, the two-step approach is considered an effective strategy for the pharmacological management of pain in children with cancer. There are a limited number of pain medicines available that can be safely used in children with a two-step approach. This approach consists of a different category of analgesics to be used according to the pain severity.
The First Step: for mild pain:
Paracetomol and ibuprofen should be considered as first options in children older than 3 months and who can take medicine orally. Paracetomol is the only option for the child who is below three months of age. No other non-steroidal anti-inflammatory drug (NSAID) has been recommended as an alternative to ibuprofen considering efficacy and safety in children. Both, paracetomol and ibuprofen have adverse effects reported in children. Ibuprofen has a potential for renal and gastrointestinal toxicity and bleeding while paracetomol is associated with hepatotoxicity in case of acute overdose.
The Second Step: Moderate to Severe Pain:
Administration of an opioid should be considered in children assessed to have moderate to severe pain. Morphine is the drug of choice for this step. However, other strong opioids should be considered as an alternative to morphine, when it is either not available or causes intolerable side effects. Routine rotation of opioids is not recommended and according to recent evidence, it is only considered in the presence of inadequate pain relief with intolerable side effects.
Dosing at regular intervals:
This is one of the key principles in treating persistent cancer pain in children. It is strongly recommended that analgesics should be administered on a regular basis rather than on an ‘as required basis’ in persistent pain in children. There are very few conditions in cancer pain, where the pain episodes are truly intermittent and predictable; perhaps in these conditions ‘as required basis’ may be considered.
Generally, children suffer from persistent pain in cancer. Therefore, they should receive analgesics at regular intervals. In addition to this regular dosing ‘rescue doses’ for intermittent and breakthrough pain should always be planned.10
Using the appropriate route of administration:
In children, analgesics should be administered by the most effective, simplest and least painful route. The oral route is the most convenient and the least expensive route of administration; however, when the oral route is not possible/effective then alternative routes e.g. intravenous, subcutaneous, rectal or transdermal routes should be considered. The decision is based on clinical judgment of a physician about effectiveness of the route and the child’s preference. The intramuscular route is painful and should be avoided whenever possible.
The rectal route has an unpredictable bioavailability even for common analgesics which limit its applicability in clinical practice.9
Adapting treatment to the individual child:
The pharmacological treatment should be tailored according to the individual child’s needs of pain control. Opioid analgesics should be given in titrating manner according to the individual requirement and preset targets in the sick child. Therefore, the dose should be adapted in steps until the correct dosage has been found, based on the child’s pain control. There is no specific or maximum dose of opioids that can be predicted in any individual case. The correct dose should be determined in collaboration with the patient to achieve the best possible pain relief with less tolerable side effects. The most recent WHO guidelines recommend commonly used step one and step two analgesic regimens (Table 1-4).
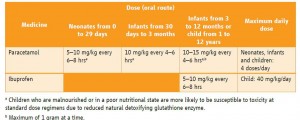
Table 1: Non-opioid analgesics for the relief of pain in neonates, infants and children
(Source: WHO guidelines on the pharmacological treatment of persisting pain in children with medical illnesses 2012)
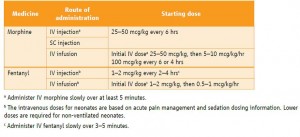
Table 2: Starting dosages for opioid analgesics for opioid-naive neonates
(Source: WHO guidelines on the pharmacological treatment of persisting pain in children with medical illnesses 2012).
Table 3: Starting dosages for opioid analgesics in opioid-naive infants (1 month – 1 year)
(Source: WHO guidelines on the pharmacological treatment of persisting pain in children with medical illnesses 2012)
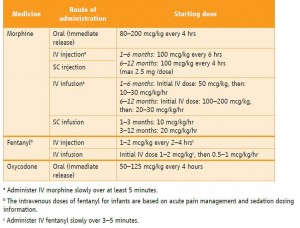
Table 4: Starting dosages for opioid analgesics in opioid-naive children (1–12 years)
(Source: WHO guidelines on the pharmacological treatment of persisting pain in children with medical illnesses 2012)
CONCLUSION
Cancer pain is very much treatable in children but success requires a holistic approach. It is strongly recommended that analgesics in children suffering from cancer pain should be managed using two -steps approach rather the conventional three step ladder. Paracetomol and ibuprofen are analgesics of choice in the first step for mild pain while morphine is recommended as the first-line strong opioid for moderate to severe pain.
The attention should be directed to pain management plans that improve the quality of life in children with cancer. Even when the most practical guidelines and sophisticated techniques are being utilized; the most effective therapeutic modality remains an empathic and caring physician.
REFERENCES
- National Cancer Institute – Comprehensive Cancer Information 2013. Available on www.cancer.gov (Accessed on 14 March 2014).
- Jalmsell L, Kreicbergs U , Onelöv E, Steineck G, Henter JI. Symptoms affecting children with malignancies during the last month of life. : A Nationwide Follow-up. Pediatrics 2006;117(4):1314-1320 [Free Full Text] doi: 10.1542/peds.2005-1479
- Classification of cancer pain in children. WHO guidelines on the Pharmacological Treatment of Persisting Pain in Children with Medical Illnesses. 2012. Available at www.ncbi.nlm.nih.gov/books/NBK138356. (Accessed on 14 March 2014)
- Berde CB, Sethna NF. Analgesics for the treatment of pain in children. N Engl J Med 2002;347(14):1094-103 [PubMed] [Free Full Text]
- Tomlinson D, von Baeyer CL, Stinson JN, Sung L. A systematic review of faces scales for the self-report of pain intensity in children. Pediatrics 2010; 126:e1168-98. doi: 10.1542/peds.2010-1609. Epub 2010 Oct 4. [PubMed] [Free Full Text]
- Breau LM, McGrath PJ, Camfield CS, Finley GA. Psychometric properties of the non-communicating children’s pain checklist-revised. Pain 2002; 99(1-2):349-57. [PubMed]
- Malviya S, Voepel-Lewis T, Burke C, Merkel S, Tait AR. The revised FLACC observational pain tool: improved reliability and validity for pain assessment in children with cognitive impairment. Paediatr Anaesth 2006; 16(3):258-65. [PubMed]
- Cancer pain relief with a guide to opioid availability, 2nd ed. Geneva, World Health Organization, 1996.
- Okkola KT, Hamunen K, Maunuksela EL. Clinical pharmacokinetics and pharmacodynamics opioid analgesics in infants and children. Clin Pharmacokinet. 1995 May;28(5):385-404. [PubMed]
- Guideline for the use of chronic opioid therapy in chronic noncancer pain: evidence review. Glenview, IL, The American Pain Society in Conjunction with The American Academy of Pain Medicine, 2009. Available on http://www.ampainsoc.org/pub/pdf/Opioid_Final_Evidence_Report.pdf, (Accessed 9 September 2011).