Sukhminder Jit Singh Bajwa, MD, MBA, FACEE1, Chhavi Sawhney, DNB2, Menaal Khanna, MBBS3
1Professor; 3Resident
Department of Anesthesiology, Gian Sagar Medical College and Hospital, Ram Nagar, Banur, National Highway 64, Jansla, Patiala, Punjab 140506, (India)
2Additional Professor, Department of Anesthesiology, Jai Prakash Narayan Apex Trauma Center (JPNATC), AIIMS, Ring Road, Chaudhary Harsukh Marg, Sarojini Nagar, Raj Nagar, Safdarjung, New Delhi, Delhi 110029, (India)
Correspondence: Prof. Sukhminder Jit Singh Bajwa, House No-27-A, Ratan Nagar, Tripuri, Patiala, Punjab 140506, (India); Phone: +91 9915025828, +91 1752352182; E-mail: sukhminder_bajwa2001@yahoo.com
ABSTRACT
For decades, vitamin K antagonist warfarin has been used for thromboprophylaxis or stroke prevention in atrial fibrillation. Recently, direct thrombin inhibitor – dabigatran and factor Xa inhibitors – rivaroxaban and apixaban, have emerged as alternatives to warfarin. The perioperative management of antithrombotic therapy involves establishing a balance between hemorrhagic risk and thrombotic risk. Routine coagulation assays like prothrombin time and activated partial thromboplastin time provide a crude estimation of their activity. Further, no specific antidotes are available to reverse their effect. These drugs are discontinued before elective surgery and timing is based on the patient’s renal status also. For emergency surgery or bleeding, the management includes the principles of bleeding control; hemodialysis may be effective for dabigatran. Prothrombin complex concentrates are found to be more effective than frozen plasma but more studies are warranted.
Key words: Anticoagulants; Apixaban, Dabigatran; Edoxaban; Rivaroxaban; Warfarin
Citation: Bajwa SJS, Sawhney C, Khanna M. New and old oral anticoagulants in anesthesia practice: a balancing approach. Anaesth Pain & Intensive Care. 2016;20 Suppl 1:S119-S125
Received: 20 August 2016; Reviewed: 12 September 2016; Accepted: 23 September 2016
INTRODUCTION
Vitamin K antagonists (VKA) have been the standard of care for treatment and prophylaxis of thromboembolic complications in patients with mechanical heart valves or atrial fibrillation.1Despite their efficacy, they have many limitations. The problems encountered with warfarin include delayed onset and offset of action, unpredictable pharmacokinetics and pharmacodynamics. It has numerous drug- drug and drug-food interactions and requires frequent laboratory monitoring due to narrow therapeutic and safety index.2 Over the last 5-6 years, new direct oral anticoagulants (NOACs) such as dabigatran etixalate, rivaroxaban, apixaban and edoxaban have been approved for long term anticoagulation. NOACs target key coagulation factor which is highlighted in their names like rivaroxaban, apixaban and edoxaban inhibit factor Xa whereas, dabigatran etixalate inhibits thrombin complex (factor IIa).3 NOACs have many advantages when compared with VKAs, e.g. comparatively short half-lives, predictable pharmacokinetics and pharmacodynamics, so there is no requirement for routine monitoring (Table 1).4 There are many studies to show that NOACs are neither inferior, nor superior to VKAs in preventing stroke or systemic embolization in patients with atrial fibrillation without increasing risk of intracranial bleed or mortality.5–9 NOACs have improved safety and efficacy when compared with LMWH for thromboprophylaxis after major orthopedic surgery.9–13 However, perioperative management of patients taking NOACs is a challenge especially during emergency surgery, trauma, bleeding or drug overdose.
Table 1: Differences between VKA and NOACs
| Parameter | VKA | NOAC |
| Onset of action | Long (days) | Short ( Hours) |
| Duration of action | Long | Short |
| Drug interaction | Yes | Few |
| Food interaction | Yes | No |
| Antidote | Yes | No |
| Renal excretion | No | Yes (dabigatran) |
PHARMACOKINETICS OF NOACs
Dabigatran etixalate
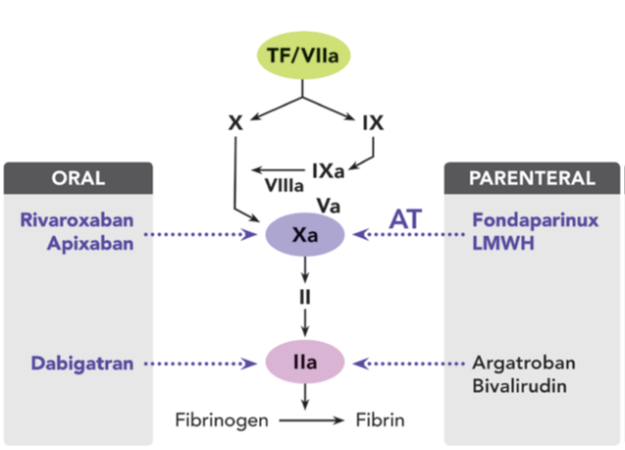
Dabigatran is available as a prodrug, dabigatran etixalate as the drug itself is highly hydrophilic and not orally bioavailable. After oral administration, dabigatran etixalate is rapidly and completely converted to dabigatran by serum esterases.14 Dabigatran is a reversible direct thrombin inhibitor which inhibits both free and fibrin bound thrombin. By inhibiting thrombin, it prevents the conversion of fibrinogen to fibrin and thus, prevents thrombus formation ( Figure 1). It has a bioavailability of 6.5% and a serum half-life of 12-17 hours.15 In contrast to the other NOACs, the low protein binding of dabigatran allows it to be eliminated by hemodialysis.16 In case of moderate hepatic impairment, it can be safely administered without dose adjustment. It is involved in few drug interactions (mainly P-glycoprotein inhibitors), no food interactions and does not require routine coagulation monitoring. The major route of elimination is renal which clears 85% of the drug. Thus, there is accumulation of the drug in the setting of renal insufficiency and this correlates with the degree of renal impairment.
Dosage for thromboprophylaxis after surgery is 110 mg, one to four hours after surgery followed by 220 mg once daily. For stroke prevention after atrial fibrillation, the dose is 150 mg twice daily decreased to 110 mg twice daily in the elderly.
Figure 1: Effect site of anticoagulation agents
Oral Direct Factor Xa Inhibitors
Factor Xa is the rate limiting factor in thrombin generation and amplification. Direct factor Xa inhibitors inhibit free factor Xa, factor Xa in the clots and in prothrombinase complex.
Rivaroxaban and Apixaban
Both rivaroxaban and apixaban selectively and competitively bind with factor Xa and block its interaction with prothrombin (Figure 1).
Both drugs have good bioavailability and high protein binding. About 30% of both the drugs are excreted unchanged by the kidneys. For rivaroxaban, rest of the drug undergoes inactivation in the liver. Thus, two-thirds of rivaroxaban is eliminated by non-renal mechanism and 25% of apixaban is transformed into metabolites in the liver and excreted in feces. CYP3A4 is involved in hepatic clearance of these drugs, so these should be cautiously administered with inducers and inhibitors of CYP3A4.17 Apixaban is one of the substrates for P-glycoprotein so the plasma levels of the drug can increase if co-administered with P-glycoprotein (P-gp) inhibitors. Both rivaroxaban and apixaban cannot be eliminated during hemodialysis.
Table 2: Pharmacokinetics and pharmacodynamics of NOACs
| Variables | Dabigatran | Rivaroxaban | Apixaban |
| Mechanism of action | Thrombin inhibitor | Factor Xa inhibitor | Factor Xa inhibitor |
| Bioavailability | 3-7% | 60-70% without food,100% with food | 60-70% |
| Plasma Protein binding | 35% | 90% | 87% |
| Plasma half life | 12-16 hours | 5-13 hours | 8-15 hours |
| Peak level after ingestion | 1.25-3 hours | 2-4 hours | 3-4 hours |
| Renal clearance | 85% | 30% | 30% |
| Hepatic degradation | 15% | 70% | 70% |
| P-gp transporter interaction | ++ | + | + |
| CYP3A4 interaction | – | + | + |
The recommended dose of rivaroxaban is 20 mg once daily for thrombosis or stroke prevention in patients with AF patients. It is reduced to 15 mg in patients with CrCl < 50 ml/min. It is given as 10 mg once daily within 6-10 hours after surgery for 5 weeks post THR and 2 weeks postTKR.18 Whereas, apixaban is given 2.5 mg twice daily within 12-24 hours of surgery post THR and post TKR. The dose is 5 mg twice daily for patients in AF.2
MONITORING ANTICOAGULATION WITH NOACs
Due to a narrow therapeutic index, frequent monitoring of anticoagulation is required with warfarin. The anticoagulant activity of warfarin is measurement using INR (International normalized ratio). The target is 2.5 (2.0 to 3.0) and 3.0 (2.5-3.5) for treatment in patients with mechanical heart valves.19
Routine monitoring of anticoagulant activity is not required with NOACs, it is required during emergency surgery, trauma, acute bleed or suspected overdose in anticoagulated patients. Monitoring is also required for dose adjustment in patients with renal impairment. NOACs exhibit variable effects on the coagulation assays which are influenced by the type of drug, dose of drug and reagent used. Routine tests like prothrombin time (PT) and activated partial thromboplastin time (aPTT) do not show sensitivity or linearity for NOACs. A normal PT or aPTT does not exclude clinically relevant effect of these drugs.20 Due to the site of action of dabigatran, most of the coagulation parameters will be prolonged except PT. The relationship between dabigatran levels and aPTT is curvilinear so as the drug levels increase, the precision is lost. Thrombin time (TT) might be prolonged even with the clinically insignificant levels of the drug as it is overly sensitive. The most reliable methods available to measure the effects of dabigatran is dilute thrombin time or direct thrombin inhibitor (Hemoclot®) assay which has a linear correlation with the drug concentration and ecarin clotting time assay.21 In ecarin clotting time essay, prothrombin is converted to meizothrombin by the snake venom ecarin and dabigatran inhibits meizothrombin in dose-dependent manner. But, this test is not widely available or frequently used.22 Partial thromboplastin time (PTT) can be used if no other test is available and a normal test would indicate the absence of clinically relevant anticoagulant activity.23
Rivaroxaban and apixaban cannot be measured using routine coagulation assays. Rivaroxaban causes prolongation of PT but the results vary with the reagent used and the sensitivity is decreased at lower drug levels. Anti-factor Xa assay using specific drug calibrators can be used to measure blood concentration of these drugs and are expressed as ng/ml.24
PERIOPERATIVE MANAGEMENT
The perioperative management of patients on oral anticoagulants depends upon patient as well as procedure related risk of bleeding and thrombosis. The discontinuation and restart of therapy depends on the pharmacokinetics and pharmacodynamics of the drug.25 A bleeding tendency is suspected if there is a previous history of bleeding, hepatic or renal impairment or treatment with dual antiplatelet therapy. There are various scoring systems available for assessing the risk for bleeding.26 On the other hand, patients with CHADS2 score (score to assess stroke risk in patients with atrial fibrillation) more than 2 are at an increased risk of thrombosis. It is recommended that the elective procedure should be delayed if there is history of thrombotic event, major hemorrhage in the past three months, the patient is pregnant or less than three months postpartum.27
Warfarin has a half-life of 36 hours so for low and moderate risk procedures, warfarin should be stopped five days prior to surgery.28 According to 2012 ACCP antithrombotic therapy guidelines, warfarin can be continued in the perioperative period for minor procedures with low risk of bleeding like dental procedures (tooth extraction, RCT), skin procedures (skin biopsy) and cataract surgery.28 Bridging therapy with heparin is recommended for patients with high risk of bleeding during withdrawal of VKAs but no recommendations are available for patients with moderate risk of bleeding. Bridging therapy may be reserved for patients with mechanical heart valves and high risk for TE, history of recent stroke, TIA or CHADS2 score of 5 or 6.25 However, recent meta-analyses have revealed that bridging therapy may not provide added benefit and may lead to increased periprocedural bleeding.29
Like warfarin, there are various studies to prove that oral anticoagulants can be safely continued in the perioperative period for minor surgeries like ophthalmologic surgeries.30 Amongst NOACs, the timing of discontinuation of dabigatran is decided by creatinine clearance and the bleeding risk associated with the procedure (Table 2).23,31
Table 2: Creatinine clearance and the bleeding risk
| Creatinine clearance
( ml/min) |
Half-life ( hours) | Time of last dose before surgery | |
| Normal bleeding risk | High bleeding risk | ||
| >80 | 13 | 1 day | 2-4 days |
| 50-80 | 15 | 1 day | 2-4 days |
| 30-50 | 18 | >2 day | >4 days |
| <30 | 27 | 2-5 days | >5 days |
Numerous anesthesia societies have proposed guidelines to improve safety of patients on anticoagulants for neuraxial block or surgery. The European guidelines recommend a gap of two half- lives between discontinuation of drug and neuraxial injection for NOACs: 34 hours for dabigatran, 22-26 hours for rivaroxaban and 26-30 hours for apixaban. It was seen that the plasma drug concentration decrease to about 25% after two half–lives.32 After two half-lives ,the elimination slows down so waiting longer would not decrease the plasma concentration significantly.33 The residual anticoagulant effect seems to facilitate prevention of TE in the immediate postoperative period also. However, these studies were performed in the young subjects and the elderly or the patients with renal impairment and other comorbidities can have longer drug half-lives. The Scandinavian guidelines recommend 18 hours for rivaroxaban but there are no guidelines for dabigatran and apixaban.34,35 The French study group recommended a 24 hour interval for procedures with low risk of bleeding and to restart after 24 hours. They recommend a 5 day interruption for procedures with moderate or high risk of bleeding and to restart according to the risk of bleeding. For patients with high risk of thrombosis, it is recommended to initiate bridging 12 hours after the last dose of NOACs for patients with high risk of thrombosis.36 Catheter placement and removal should be considered when the anticoagulation activity is minimum and the patient should be monitored for signs of hematoma. Rosenchal et al recommended that the anticoagulation should be started 8 hours minus the time taken for peak concentration on the basis that it takes 8 hours for the clot to reach the maximum strength.33
Another simplified approach for temporary withdrawal of NOACs before surgery is given in Table 3.18
Table 3: A simplified approach for temporary withdrawal of NOACs before surgery
| Anticoagulant | Stop before insertion | Check before block | Caution |
| Dabigatran | 3.5-4 days | TT, aPTT | CrCl < 50 ml / min
Age > 75years |
| Rivaroxaban | 2-3 days | Anti Xa, PT | CrCl < 30 ml / min |
| Apixaban | 3-4 days | Anti Xa | CrCl<30 ml / min,
age ≥ 80years and weight ≤ 60 kg |
REVERSAL AND MANAGEMENT OF BLEEDING
Vitamin K1 can lead to activation of existing clotting factors so it can be used for reversal of warfarin. It can be used orally as well as iv.19 The maximum effect of oral Vitamin K1 is seen within18-24 hours as compared to 6-12 hours with intravenous Vitamin K1.37 Oral administration is the preferred route where the procedure can be delayed for 18-24 hours and the risk of bleeding is mild to moderate.38 For surgery where the procedure can be delayed for 6-12 hours only, intravenous Vitamin K1 is given in a dose of 10 mg IV. For rapid reversal of warfarin, the options available are prothrombin complex concentrate and frozen plasma. Prothrombin complex concentrate (PCC) is required for rapid reversal of warfarin in patients with major bleed or urgent surgery within six hours. PCC contains highly purified concentrate of coagulation factors prepared from pooled plasma and has undergone virus reduction.39 However, the efficacy of PCC decreases after 6 hours due to short half-life of factor VII so Vitamin K1 10 mg IV has to be administered concurrently. The recent guidelines by national Advisory Committee recommend the dose to target INR of 1.5 and maximum dose of 3,000 IU (200 ml).39 Frozen plasma is indicated for urgent reversal of warfarin if PCC is unavailable or contraindicated. The target level of coagulation factors required for adequate hemolysis is 30-40% so 10-15 ml/kg of frozen plasma would be required.
Summary of recommendations for reversal of warfarin is given in Table 4.39
Table 4: Summary of recommendations for reversal of warfarin
| Urgency of procedure | Recommendations for reversal of warfarin |
| Emergency ( 0-6 hours) | PCC based on weight and INR
Vitamin K1 slow iv infusion |
| Urgent ( 6-12 hours) | Vitamin K1 slow iv infusion |
| Able to wait 24-36 hours | Vitamin K1 slow iv infusion |
Immediate reversal of NOACs might be required for emergency surgery or in a bleeding patient. If the bleeding is not severe and the surgery can be delayed, stopping the drug and providing supportive treatment is sufficient. In case of moderate bleeding, initial measures are volume resuscitation, identification of the source of bleeding and local hemostasis. FFP or PCC do not have a role in bleeding due to NOACs as there is an ongoing clotting factor inhibition rather than a deficiency of the factors. If anticoagulant overdose is suspected, activated charcoal can be administered within 1-2 hours but it has no role during intraoperative period. Hemodialysis or hemoperfusion can be useful for dabigatran. Tranexamic acid and antifibrinolytics may be used as adjuncts to augment coagulation. The role of FFP’s or factor VIIa has not been studied in human beings. PCCs are available as concentrates of three (II, IX, X) or four (II, VII, IX, X) factors and enhance thrombin generation. The four factor PCCs have activated and inactivated form. 40Small quantities of heparin, antithrombin, protein C and S can also be added to PCCs but the results with PCCs are controversial. The best approach to stop NOAC bleeding would be the administration of antidote.
Thus, the management of bleeding due to anticoagulants would depend upon the severity of bleeding, hemodynamic stability and mortality risk as well as the possible results from the future research.
CURRENT AND FUTURE RESEARCH FOR ANTAGONIST (RE-VERSE AD)™ (NCT02104947)
RE-VERSE AD™ is an ongoing, global Phase III patient study initiated by Boehringer Ingelheim® in 2014 to investigate idarucizumab in emergency settings. Up to 300 patients taking dabigatran, aged 18 years or over are expected to be enrolled from more than 400 centers in 38 countries worldwide. The broad inclusion criteria reflect the types of patients that would require urgent anticoagulant reversal in the real-world emergency setting. These include severely ill or injured patients, (e.g. patients with sepsis, a severe intracranial hemorrhage or a large vessel injury).
Idarucizumab is a humanized antibody fragment, or Fab, designed as a specific reversal agent to dabigatran.41 Idarucizumab binds specifically to dabigatran molecules only, neutralizing their anticoagulant effect without interfering with the coagulation cascade.41
Results from an interim analysis of the Phase III RE-VERSE AD™ patient study demonstrate that 5 gm of idarucizumab immediately reversed the anticoagulant effect of dabigatran (Pradaxa®) in patients requiring urgent anticoagulant reversal. The primary endpoint of the study is the degree of reversal of the anticoagulant effect of dabigatran achieved by 5 gm idarucizumab within 4 hours measured by diluted thrombin time (dTT) and ecarin clotting time (ECT).
Patients received 5 gm of intravenous idarucizumab* administered as two 50 ml bolus infusions, each containing 2.5 gm of idarucizumab, no more than 15 minutes apart.3 Blood was collected and assessed for anticoagulant effect at baseline, after administration of the first vial of idarucizumab*, and then between 10 and 30 minutes and 1, 2, 4, 12 and 24 hours after administration of the second vial.41
The primary endpoint was the maximum degree of reversal of the anticoagulant effect of dabigatran, determined using different laboratory tests (including the coagulations tests diluted thrombin time (dTT) and ecarin clotting time (ECT)) at any point from the end of the first idarucizumab* infusion, up to 4 hours after administration of the second infusion.41
Secondary endpoints include the proportion of patients achieving complete normalization of the dTT or ECT in 4 hours, the reduction in unbound dabigatran concentration, and clinical outcomes as assessed by the treating clinician.
Conflict of interest: No conflict of interest with anyone
Authors’ contribution: SJSB & CS: Concept, Design, Literature search, Data acquisition, Manuscript preparation & review
MK: Design, Literature search, Manuscript preparation & review
REFERENCES
- Untereiner O, Seince P-F, Chterev V, Leblanc I, Berroëta C, Bourel P, et al. Management of Direct Oral Anticoagulants in the Perioperative Setting. J Cardiothorac Vasc Anesth. 2015 Jun;29(3):741–8. [PubMed] [Free full text] doi: 10.1053/j.jvca.2014.12.019.
- Bhanwra S, Ahluwalia K. The new factor Xa inhibitor: Apixaban. J Pharmacol Pharmacother. 2014;5(1):12. [PubMed] [Free full text] doi: 10.4103/0976-500X.124409.
- Breuer G, Weiss DR, Ringwald J. “New” direct oral anticoagulants in the perioperative setting: Curr Opin Anaesthesiol. 2014 Aug;27(4):409–19. [PubMed] [Free full text] doi: 10.1097/ACO.0000000000000100.
- Eikelboom JW, Weitz JI. New Anticoagulants. Circulation. 2010 Apr 6;121(13):1523–32. [PubMed] [Free full text] doi: 10.1161/CIRCULATIONAHA.109.853119.
- Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–992. [PubMed] [Free full text] doi: 10.1056/NEJMoa1107039.
- Ruff CT, Giugliano RP, Braunwald E, Hoffman EB, Deenadayalu N, Ezekowitz MD, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955–962. [PubMed] [Free full text] doi: 10.1016/S0140-6736(13)62343-0.
- Gómez-Outes A, Terleira-Fernández AI, Calvo-Rojas G, Suárez-Gea ML, Vargas-Castrillón E. Dabigatran, Rivaroxaban, or Apixaban versus Warfarin in Patients with Nonvalvular Atrial Fibrillation: A Systematic Review and Meta-Analysis of Subgroups. Thrombosis. 2013;2013:1–18. [PubMed] [Free full text] doi: 10.1155/2013/640723.
- Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–1151. [Free full text] doi: 10.1056/NEJMoa0905561
- Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–891. [PubMed] [Free full text] doi: 10.1056/NEJMoa1009638.
- Werth S, Halbritter K, Beyer-Westendorf J. Efficacy and safety of venous thromboembolism prophylaxis with apixaban in major orthopedic surgery. Ther Clin Risk Manag. 2012 Mar;139. [PubMed] [Free full text] doi: 10.2147/TCRM.S24238.
- Kakkar AK, Brenner B, Dahl OE, Eriksson BI, Mouret P, Muntz J, et al. Extended duration rivaroxaban versus short-term enoxaparin for the prevention of venous thromboembolism after total hip arthroplasty: a double-blind, randomised controlled trial. Lancet Lond Engl. 2008 Jul 5;372(9632):31–9. [PubMed] [Free full text] doi: 10.1016/S0140-6736(08)60880-6.
- Eriksson BI, Borris LC, Friedman RJ, Haas S, Huisman MV, Kakkar AK, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after hip arthroplasty. N Engl J Med. 2008 Jun 26;358(26):2765–75. [PubMed] [Free full text] doi: 10.1056/NEJMoa0800374.
- Lassen MR, Ageno W, Borris LC, Lieberman JR, Rosencher N, Bandel TJ, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty. N Engl J Med. 2008 Jun 26;358(26):2776–86. [PubMed] [Free full text] doi: 10.1056/NEJMoa076016.
http://www.nejm.org/doi/full/10.1056/NEJMoa076016
- Sehgal V, Bajwa SS, Bajaj A. New orally active anticoagulants in critical care and anesthesia practice: The good, the bad and the ugly. Ann Card Anaesth. 2013;16(3):193. [PubMed] [Free full text] doi: 10.4103/0971-9784.114244.
- Stangier J. Clinical pharmacokinetics and pharmacodynamics of the oral direct thrombin inhibitor dabigatran etexilate. Clin Pharmacokinet. 2008;47(5):285–95. [PubMed] [Free full text] doi: 10.2165/00003088-200847050-00001
- Khadzhynov D, Wagner F, Formella S, Wiegert E, Moschetti V, Slowinski T, et al. Effective elimination of dabigatran by haemodialysis. A phase I single-centre study in patients with end-stage renal disease. Thromb Haemost. 2013 Apr;109(4):596–605. [PubMed] [Free full text] doi: 10.1160/TH12-08-0573.
- Levy JH, Key NS, Azran MS. Novel Oral AnticoagulantsImplications in the Perioperative Setting. Anesthesiology. 2010;113(3):726–745. [PubMed] doi: 10.1097/ALN.0b013e3181ebdb15.
- Volk T, Kubulus C. New oral anticoagulants and neuraxial regional anesthesia: Curr Opin Anaesthesiol. 2015 Oct;28(5):605–9. [PubMed] doi: 10.1097/ACO.0000000000000234.
- Ageno W, Gallus AS, Wittkowsky A, Crowther M, Hylek EM, Palareti G, et al. Oral anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012 Feb;141(2 Suppl):e44S–88S. [PubMed] [Free full text] doi: 10.1378/chest.11-2292.
- Cuker A, Siegal DM, Crowther MA, Garcia DA. Laboratory Measurement of the Anticoagulant Activity of the Target-specific Oral Anticoagulant Agents: A Systematic Review. J Am Coll Cardiol. 2014 Sep 16;64(11):1128–39. [PubMed] [Free full text] doi: 10.1016/j.jacc.2014.05.065.
- Stangier J, Feuring M. Using the HEMOCLOT direct thrombin inhibitor assay to determine plasma concentrations of dabigatran. Blood Coagul Fibrinolysis Int J Haemost Thromb. 2012 Mar;23(2):138–43. [Full Text] doi: 10.1097/MBC.0b013e32834f1b0c
- Stangier J, Rathgen K, Stähle H, Gansser D, Roth W. The pharmacokinetics, pharmacodynamics and tolerability of dabigatran etexilate, a new oral direct thrombin inhibitor, in healthy male subjects. Br J Clin Pharmacol. 2007 Sep;64(3):292–303.
[PubMed] [Free full text] doi: 10.1111/j.1365-2125.2007.02899.x
- Levy JH, Faraoni D, Spring JL, Douketis JD, Samama CM. Managing new oral anticoagulants in the perioperative and intensive care unit setting. Anesthesiology. 2013 Jun;118(6):1466–74.
- Lindhoff-Last E, Samama MM, Ortel TL, Weitz JI, Spiro TE. Assays for measuring rivaroxaban: their suitability and limitations. Ther Drug Monit. 2010 Dec;32(6):673–9. [Full Text] doi: 10.1097/FTD.0b013e3181f2f264
- Spyropoulos AC, Al-Badri A, Sherwood MW, Douketis JD. Periprocedural management of patients receiving a vitamin K antagonist or a direct oral anticoagulant requiring an elective procedure or surgery. J Thromb Haemost. 2016 May;14(5):875–85. [Free full text] DOI: 10.1111/jth.13305
- Omran H, Bauersachs R, Rübenacker S, Goss F, Hammerstingl C. The HAS-BLED score predicts bleedings during bridging of chronic oral anticoagulation. Results from the national multicentre BNK Online bRiDging REgistRy (BORDER). Thromb Haemost. 2012 Jul;108(1):65–73. [Free full text] doi: 10.1160/TH11-12-0827
- Benzon HT, Avram MJ, Green D, Bonow RO. New oral anticoagulants and regional anaesthesia. Br J Anaesth. 2013 Dec 1;111(suppl 1):i96–113. [Free full text] doi: 10.1093/bja/aet401
- Douketis JD, Spyropoulos AC, Spencer FA, Mayr M, Jaffer AK, Eckman MH, et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012 Feb;141(2 Suppl):e326S–50S. [PubMed] [Free full text] doi: 10.1378/chest.11-2298
- Douketis JD, Spyropoulos AC, Kaatz S, Becker RC, Caprini JA, Dunn AS, et al. Perioperative Bridging Anticoagulation in Patients with Atrial Fibrillation. N Engl J Med. 2015 Aug 27;373(9):823–33. [PubMed] [Free full text] doi: 10.1056/NEJMoa1501035
- Calenda E, Genevois O, Cardon A, Muraine M. Peribulbar anesthesia in 750 patients treated with oral anticoagulants. Int J Ophthalmol. 2014;7(1):110. [PubMed] [Free full text] doi: 10.3980/j.issn.2222-3959.2014.01.20
- Stangier J, Rathgen K, Stähle H, Mazur D. Influence of renal impairment on the pharmacokinetics and pharmacodynamics of oral dabigatran etexilate: an open-label, parallel-group, single-centre study. Clin Pharmacokinet. 2010 Apr;49(4):259–68. [Free full text] doi: 10.2165/11318170-000000000-00000
- Hylek EM. Therapeutic potential of oral factor Xa inhibitors. N Engl J Med. 2010 Dec 23;363(26):2559–61. [Free full text]
- Rosencher N, Bonnet M-P, Sessler DI. Selected new antithrombotic agents and neuraxial anaesthesia for major orthopaedic surgery: management strategies. Anaesthesia. 2007 Nov;62(11):1154–60. [PubMed] [Free full text] doi: 10.1111/j.1365-2044.2007.05195.x
- Breivik H, Bang U, Jalonen J, Vigfússon G, Alahuhta S, Lagerkranser M. Nordic guidelines for neuraxial blocks in disturbed haemostasis from the Scandinavian Society of Anaesthesiology and Intensive Care Medicine. Acta Anaesthesiol Scand. 2010 Jan;54(1):16–41. [PubMed] [Free full text] doi: 10.1111/j.1399-6576.2009.02089.x.
- Gogarten W, Vandermeulen E, Van Aken H, Kozek S, Llau JV, Samama CM, et al. Regional anaesthesia and antithrombotic agents: recommendations of the European Society of Anaesthesiology. Eur J Anaesthesiol. 2010 Dec;27(12):999–1015. [PubMed] [Free full text] doi: 10.1097/EJA.0b013e32833f6f6f.
- Sié P, Samama CM, Godier A, Rosencher N, Steib A, Llau JV, et al. Surgery and invasive procedures in patients on long-term treatment with direct oral anticoagulants: thrombin or factor-Xa inhibitors. Recommendations of the Working Group on Perioperative Haemostasis and the French Study Group on Thrombosis and Haemostasis. Arch Cardiovasc Dis. 2011 Dec;104(12):669–76. [PubMed] [Free full text] doi: 10.1016/j.acvd.2011.09.001.
- Watson HG, Baglin T, Laidlaw SL, Makris M, Preston FE. A comparison of the efficacy and rate of response to oral and intravenous Vitamin K in reversal of over-anticoagulation with warfarin. Br J Haematol. 2001 Oct;115(1):145–9. [PubMed] [Free full text] DOI: 10.1046/j.1365-2141.2001.03070.x
- Keeling D, Baglin T, Tait C, Watson H, Perry D, Baglin C, et al. Guidelines on oral anticoagulation with warfarin – fourth edition. Br J Haematol. 2011 Aug;154(3):311–24. [PubMed] [Free full text] doi: 10.1111/j.1365-2141.2011.08753.x.
- Curtis R, Schweitzer A, van Vlymen J. Reversal of warfarin anticoagulation for urgent surgical procedures. Can J Anesth Can Anesth. 2015 Jun;62(6):634–49. [PubMed] [Free full text] doi: 10.1007/s12630-015-0366-3.
- von Heymann C, Rosenthal C, Kaufner L, Sander M. Management of direct oral anticoagulants-associated bleeding in the trauma patient: Curr Opin Anaesthesiol. 2016 Apr;29(2):220–8. [PubMed] [Free full text] doi: 10.1097/ACO.0000000000000294.
- Pollack C. V. et al. Design and rationale for RE-VERSE AD: A phase 3 study of idarucizumab, a specific reversal agent for dabigatran. Thromb Haemost. 2015; 28: 114(1). [PubMed] [Free full text] doi: 10.1160/TH15-03-0192.

