Seelora Sahu1, Suman Arora2, Hemant Bhagat3, Amlan Swain1
1Senior Resident; 2Additional Professor; 3Associate Professor
Department of Anesthesiology & Intensive Care, Postgraduate Institute of Medical Education and Research, Kairon Block, Sector 12, Chandigarh, 160012, (India)
Correspondence: Seelora Sahu, Senior Resident (DM, Neuroanesthesia), Department of Anesthesiology & Intensive Care, Postgraduate Institute of Medical Education and Research, Kairon Block, Sector 12, Chandigarh, 160012, (India); E-mail: seelora@gmail.com
ABSTRACT
Alteration of cardiac electrical activity is usually due to primary cardiac pathology, but can also be secondary to non-cardiac causes, e.g. electrolyte disturbances, hypothermia, esophageal disorders, poisoning, drugs as well as some intracranial events like ischemic stroke, cerebral hemorrhage, subarachnoid hemorrhage, space occupying lesions etc. We present a case of a young male undergoing craniotomy and excision of intracranial epidermoid presenting with an intraoperative event consisting of multiple episodes of junctional rhythm.
Key words: Junctional rhythm; Arrhythmia; Bradycardia; Intracranial neoplasm
Citation: Sahu S, Arora S, Bhagat H, Swain A. Junctional rhythm during neurosurgical procedure. Anaesth Pain & Intensive Care 2015;19(4):517-520
INTRODUCTION
Abnormalities of the electrocardiographic (ECG) traces are extremely useful in diagnosing heart disease, but they have also been known to occur in a variety of states in which the primary pathology is extra-cardiac.1 Electrocardiographic changes have been reported in electrolyte disorders, acute pulmonary embolism, central nervous system pathology, esophageal disorders,1 hypothermia,2 drugs, poisoning, electrical injury etc.3 Electrocardiographic changes have been reported in a wide range of neurologic disorders including infections like meningitis,4 demyelinating diseases like Guillian-Barre syndrome, trauma, epilepsy,5 cerebrovascular diseases, tumors etc.
Here we present a case of a young male patient with multiple episodes of bradycardia and junctional rhythm on ECG while undergoing craniotomy and excision of an intracranial epidermoid tumor.
CASE REPORT
A 21 year old male patient presented to the neurosurgery OPD with complaints of gradually progressive hearing loss on the right side, slurring of speech and right sided facial weakness since the last eighteen months. He also had complaints of weakness in the right upper and lower limbs since one year with history of choking while eating food. On clinical and radiological examination he was found to have right cerebello-pontine angle epidermoid cyst (Figure 1) and was planned for craniotomy and excision.
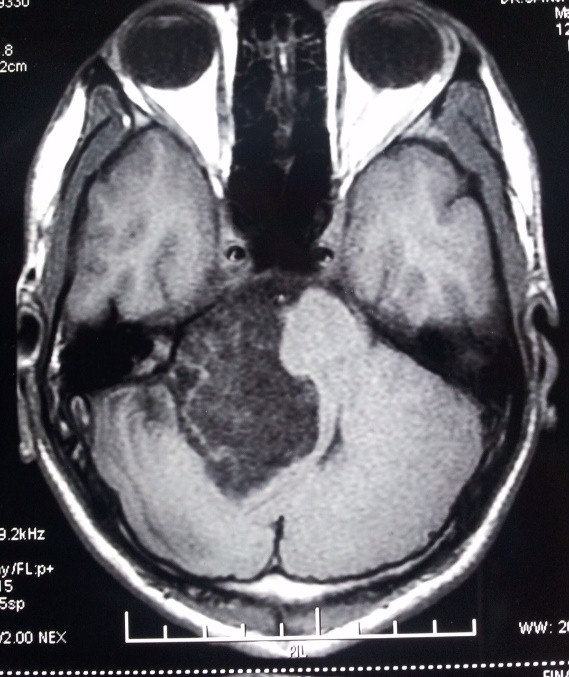 Figure 1: MRI showing the tumor in the right CP angle
Figure 1: MRI showing the tumor in the right CP angle
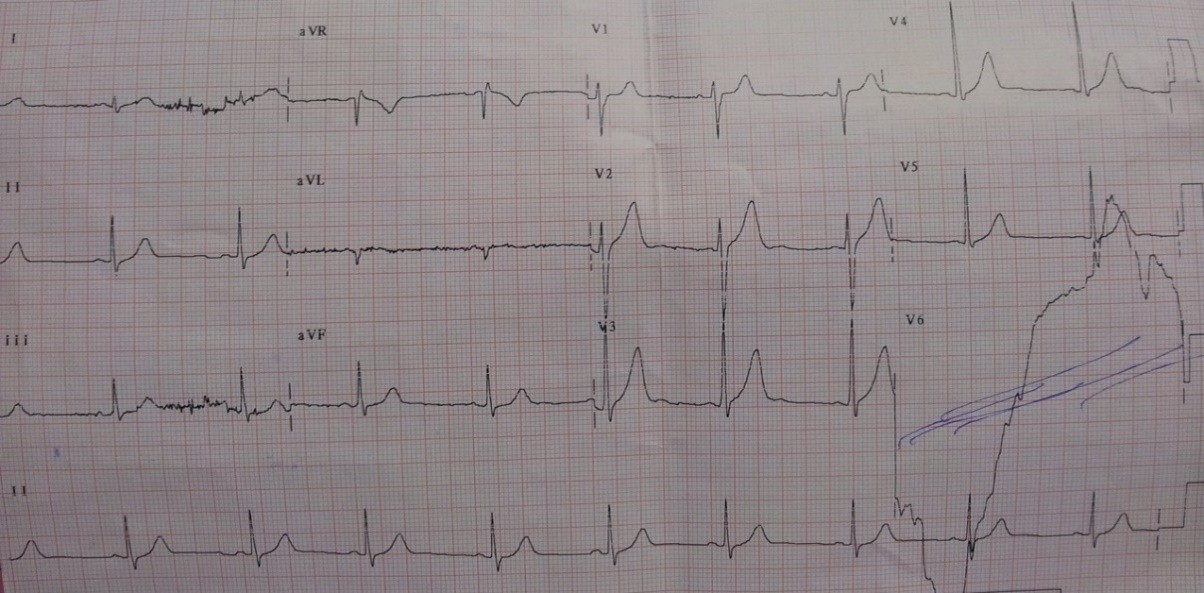
During the preoperative assessment, the patient gave no history of any systemic comorbidities such as hypertension, diabetes mellitus, bronchial asthma etc. He gave no history of palpitation, syncope, or chest pain and had a good exercise tolerance (> 4 METS). Preoperative ECG was normal (Figure 2) with a heart rate of 60 beats per minute.
The neurological examination revealed lower motor type lesion of facial nerve on the right side (VII cranial nerve), sensorineural hearing loss in the right ear (VIII cranial nerve), upward arching of right palatial arch on vocalising “aah” (IX and X cranial nerves) and mild deviation of the tongue to left side (XII cranial nerve). On assessment of airway, the modified Mallampatti grade was I with no obvious craniofacial abnormality. The patient was classified as an ASA grade I patient and was advised routine premedication in the form of tablet Ranitidine 150 mg in night and on the morning of surgery with sips of water, two hours prior to surgery.
On the day of surgery, his clinical examination revealed a heart rate 48-50 bpm and blood pressure 110/58 mmHg. In the operating room, the intravenous access was established and routine monitoring (e.g. non-invasive blood pressure monitoring, 5 lead electrocardiograph, and pulse oximetry) was established. Induction of anesthesia was done with propofol 2 mg/kg IV and intubation was facilitated with inj. vecuronium bromide 0.1 mg/kg. Inj morphine 0.1 mg/kg was used for intraoperatively analgesia. Anesthesia was maintained with propofol infusion, 66% nitrous oxide in oxygen, and intermittent boluses of vecuronium. Ventilation was maintained to achieve the end-tidal carbon dioxide (EtCO2) at 32-35 mmHg. Invasive blood pressure (IBP) monitoring was established by cannulating the left radial artery. TOF and BIS monitoring was instituted to monitor depth of anesthesia.
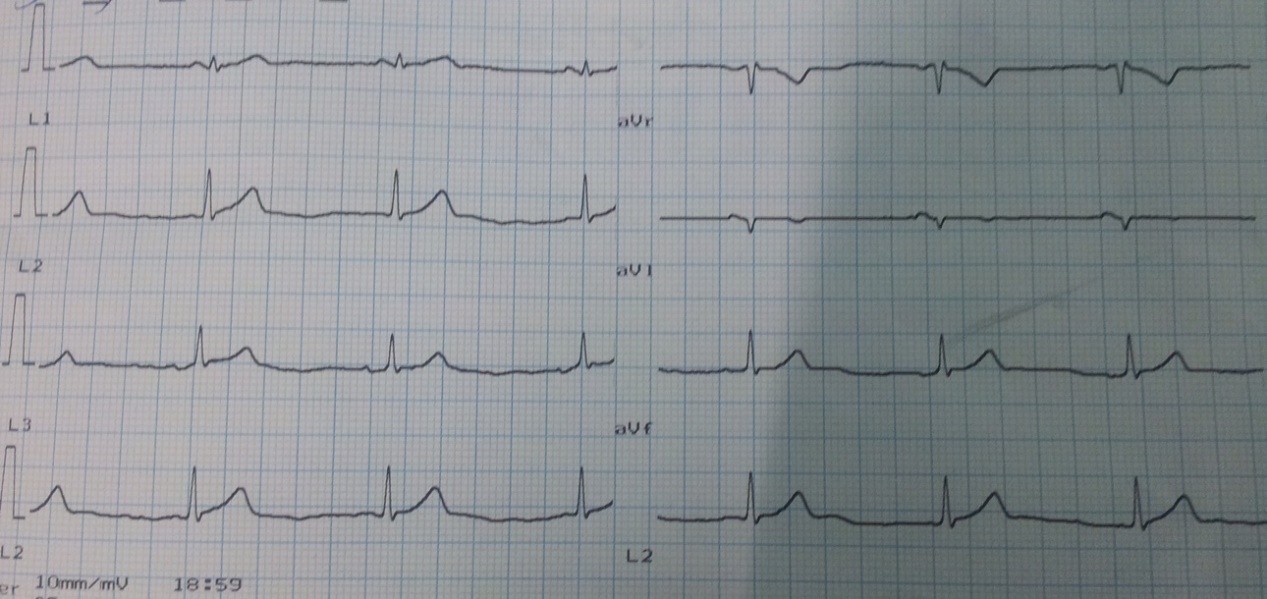
After five minutes of intubation, before positioning the patient for the surgery, a junctional rhythm in lead II and lead V was noted. The heart rate dropped to 48-49 bpm with each episode, consisting of 10-12 beats of abnormal rhythm. 2-4 episodes were observed per minute throughout the surgery but reverted to normal spontaneously at variable intervals.
There was no evidence of raised intracranial pressure as observed by the neurosurgeon.
Intraoperative blood gas analysis revealed normal acid base and electrolyte balance and normothermia was maintained throughout the procedure. Neuromuscular blockade was reversed using inj. neostigmine 50 µg/kg and glycopyrrolate 10 µg/kg on return of spontaneous respiration, at the end of surgery. The patient was left intubated in view of prolonged surgery close to the brain stem. He was shifted to the neurosurgical ICU and was extubated the next morning according to the ICU extubation protocol. Post extubation, the patient was stable with a heart rate at 58-66 bpm, regular rhythm and normal blood pressure. There were no further episodes of any ECG abnormalities and the further hospital stay was uneventful. The serum electrolytes were normal in the preoperative and postoperative period.
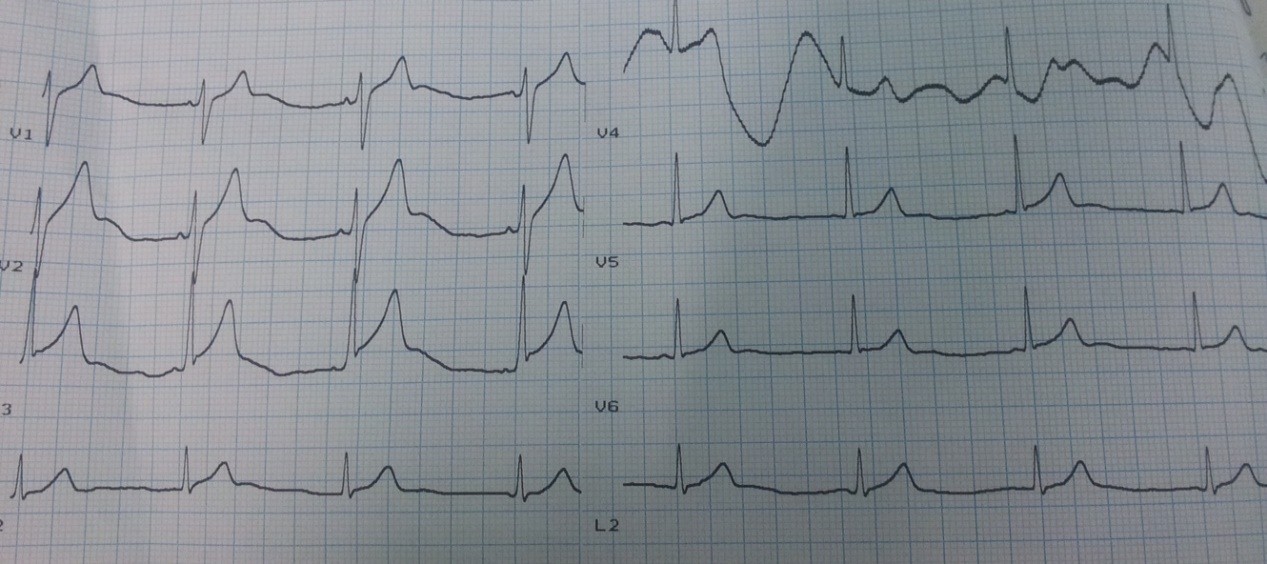
Postoperative 12 lead ECG was normal except for mild ST elevation in lead V2 and V3 (Figures 3 and 4). An echocardiographic evaluation done on the postoperative day was found to be normal.
DISCUSSION
Dysrhythmias represent an important cause of perioperative complications because during this period there are several clinical situations that may trigger changes in cardiac rhythm.1 Dysrhythmias have been were observed in up to 70.2% of patients undergoing general anesthesia as observed in a multicenter study with involving 17,201 patients.2 Electrocardiographic changes have been reported in electrolyte disorders, acute pulmonary embolism, central nervous system pathology, esophageal disorders, hypothermia, drugs, poisoning, electrical injury, anesthesia, surgery etc.3-5 It is of grave importance to recognize that the changes in ECG are because of intracranial pathology rather than a cardiac etiology as it has a significant bearing on the further management of the patient.
ECG abnormalities, which might alter management include atrial flutter or fibrillation, LVH or RVH, first, second or third-degree heart block, myocardial infarction, ST segment abnormalities, prolonged QT segment, premature atrial complexes or premature ventricular complexes, tall peaked T waves, Wolf-Parkinson-White syndrome and small QRS voltage.6
A less common finding is junctional rhythm disturbances. The causes of intraoperative junctional rhythm include surgical stress response, vagal hypertonicity, hypothermia, endotracheal tube cuff pressure or venous air embolism.7
In our patient, an adequate depth of anesthesia was maintained during intubation and surgery. The persistence of the abnormal rhythm throughout the surgery makes intubation response an unlikely cause of junctional rhythm in this patient. The patient was normothermic throughout the procedure, normovolemia was maintained and there was no evidence suggestive of any venous air embolism. High endotracheal tube cuff pressure was also ruled out. The perioperative electrolyte measurements were within normal limits and there was no history or clinical evidence suggestive of infection of any kind. Vagal hypertonicity could be the cause of junctional rhythm in our patient.
The mechanism by which the lesions of the nervous system influence the electrocardiogram though a matter of concern, could be most likely the direct effect of the autonomic nervous system on the electrophysiological behavior of the heart. [1]Multiple neurological disorders such as epilepsy, brain tumors or stroke, show this relationship.7
Tall P waves, extrasystole and prolongation of QTc interval have been associated with sympathetic stimulation, whereas sinus arrhythmia with a fixed or wandering pacemaker and nodal rhythm have been attributed to vagal stimulation in various intracranial pathologies.8 The main electrocardiographic abnormality noted with neurological diseases was nonspecific ST-T changes followed by prolonged QT interval and bundle branch block. The most common arrhythmia noted was sinus bradycardia, atrioventricular block and junctional rhythm.9
In patients with cerebral tumors without any known organic heart disease or any evidence of raised intracranial pressure, lesions of limbic structures do exert cardioarrhythmogenic effects and may provide an explanation for ECG abnormalities in patients with cerebral tumors.10 However, in our patient, the tumor was extralimbic in location.
Hakan Ay et al concluded that since troponin-T (a more specific marker of myocardial injury) did not increase after stroke, the CK-MB elevations in stroke patients are likely to be non-cardiac in origin.11 In view of these observations, the measurement of troponin-T or CK-MB was not considered necessary in our patient.
In conclusion, while managing neurosurgical cases, the presence of ECG abnormalities including junctional rhythm must be considered a possibility. In such a setting a cardiology opinion and going through a battery of tests for diagnosing the cause of ECG changes may cause a delay thus resulting in an adverse outcome.
REFERENCES
- Thompson A, Balser JR. Perioperative cardiac arrhythmias. Br J Anaesth 2004; 93:86-94.
- Atlee JL. Perioperative cardiac dysrhythmias: Diagnosis and management. Anesthesiology 1997; 86:1397-424.
- Samuels MA. Electrocardiographic manifestations of neurologic disease. Semin Neurol. 1984; 4:453-458.
- Bertrand CA, Steiner NV, Jameson AG, Lopez M. Disturbances of cardiac rhythm during anesthesia and surgery. JAMA 1971; 216:1615-1617.
- Roizen MF. The usefulness of the preoperative electrocardiogram. J Clin Monit 1993; 9:101-103.
- Agrawal S, Srivastava V. Bezold-Jarisch reflex as a cause of haemodynamic alterations during surgery in prone position. Anaesth, Pain & Intensive Care 2010; 14:115-117.
- Samuel MA. The brain-heart connection. Circulation. 2007; 116:77-84. [PubMed] [Free full text]
- Hersch C. Electrocardiographic changes in subarachnoid hemorrhage, meningitis and intracranial space-occupying lesions. Brain Heart J 1964; 26:785-793. [PubMed] [Free full text]
- Póvoa R, Cavichio L, Ana Lúcia de Almeida, Viotti D, Ferreira C, Galvão L, Pimenta J. Electrocardiographic abnormalities in neurological diseases. Arq Bras Cardiol 2003; 80:355-358.
- Koepp M, Kern a, Schmidt D. Electrocardiographic changes in patients with brain tumors. Arch Neurol 1995; 52:152-155.
[PubMed]
- Hakan Ay, Arsava EM, Sarıbaş O. Creatine kinase-MB elevation after stroke is not cardiac in origin; comparison with troponin T levels. Stroke 2002; 33:286-289. [PubMed] [Free full text]