Gurpreet Singh, MD1, Haramritpal Kaur, MD1, Shobha Aggarwal, MD2,
Gagandeep Sharda, MD3, Amandeep Singh, MS4,
Aditi Jha, MBBS5, Hiteshi Aggarwal, MBBS5
1Associate Professor; 2Professor & Head; 3Ex-postgraduate resident; 5 Postgraduate resident
Department of Anesthesiology, Guru Gobind Singh Medical College & Hospital (GGSMCH), Sadiq Road, Faridkot, Punjab 151203, (India)
4Associate Professor, Department of General Surgery, Guru Gobind Singh Medical College & Hospital (GGSMCH), Sadiq Road, Faridkot, Punjab 151203, (India)
Correspondence: Dr Haramritpal Kaur, Department of Anesthesiology, Guru Gobind Singh Medical College & Hospital (GGSMCH), Sadiq Road, Faridkot, Punjab 151203, (India); E-mail: amritk_dr@yahoo.co.in
ABSTRACT
Background: The stress response to laryngoscopy and endotracheal intubation is a commonly encountered physiological phenomenon. Though the response can be transient and harmless in normotensive healthy patients, but it may prove hazardous amongst patient with underlying cardiac disease, or hypertensive disease and its sequelae. Present study was planned to evaluate the efficacy of IV dexmedetomidine infusion and IV lignocaine in attenuating the hemodynamic responses during laryngoscopy and intubation.
Methodology: On approval from hospital ethical committee, 120 ASA grade I and II, normotensive patients in the age group of 18-60 years, planned for elective surgery under general anesthesia were enrolled in the study. Patients were divided into 3 equal groups of 40 each; Group A (Lignocaine group) received lignocaine 1.5 mg/kg IV 2 min before induction, Group B (dexmedetomidine group ) received dexmedetomidine 1 µ/kg IV infusion with syringe pump 10 min before induction, and Group C (control group) received normal saline before induction. Heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), oxygen saturation of arterial blood (SpO2) and electrocardiogram (ECG) were monitored at induction, intubation and post intubation at one minute interval till 10th minute.
Results: A better control of stress response was observed in patients receiving dexmedetomidine infusion. More decrease in HR was noted in Group B as compared to Group A (9.28 % vs. 13.40%) respectively. The decrease in MAP was also more in Group B as compared to group receiving lignocaine (5.49 % vs. 10.72%) respectively.
Conclusion: Dexmedetomidine 1 μg/kg IV is more effective in blunting stress response to laryngoscopy and endotracheal intubation as compared to lignocaine 1.5 mg/kg IV.
Key words: Dexmedetomidine; Hemodynamic response; Lignocaine; Laryngoscopy; Intubation.
Citations: Singh G, Kaur H, Aggarwal S, Sharda G, Singh A, Jha A, Aggarwal H. Intravenous dexmedetomidine vs. lignocaine in attenuating the hemodynamic responses during laryngoscopy and endotracheal intubation: a randomized double blind study. Anaesth Pain & Intensive Care 2017;21(2):181-186
Received: 31 Dec 2016, Reviewed: 26 Feb 2017, Corrected: 8 Jun 2017, Accepted: 10 Jun 2017
INTRODUCTION
Securing airway remains the most important aspect of safe anesthetic procedure. Though endotracheal tube is the perfect gold standard airway device, its placement is known to evoke stress response, predominantly in the form of tachycardia and systemic hypertension, exposing the susceptible patient to undue risk. These effects are transient in normotensive healthy patients but are more marked in patients with underlying hypertensive disease. [1] Increased sympathetic activity in patients with essential hypertension may lead to serious complications during laryngoscopy and intubation, [2] due to sympatho-adrenal stimulation which may result in a sudden rise in blood pressure, may cause left ventricular failure, arrhythmias, myocardial ischemia, intracranial hemorrhage and sudden increase in intracranial pressure.
Numerous techniques have been incorporated in current safe anesthesia practice to attenuate these adverse effects with variable success rate, including deep levels of general anesthesia prior to endotracheal intubation, using topical anesthesia of upper respiratory tract,[3] administration of intravenous local anesthetic agents (e.g., lignocaine),[4-7] beta blocking agents (esmolol, metoprolol),[8-10] vasodilators (sodium nitroglycerine),[11] calcium channel blockers (nifedipine, nicardipine),[12,13] narcotic analgesics (fentanyl, remifentanil and alfentanil), [14-18] and some other agents including oral gabapentin,[19] pregabalin and clonidine [20] etc.
As none of the above mentioned approaches have proved to be entirely satisfactory, the search for an ideal agent continues. Dexmedetomidine is a relatively new alpha-2 adrenergic agonist. Alpha- 2 adrenergic agonists have been widely used as adjuncts in the preoperative period for their analgesic, sedative/hypnotic, anxiolytic and sympatholytic properties.[7,21-27] Dexmedetomidine has been used and found to be more effective to attenuate the stress response to laryngoscopy when compared with agents like esmolol, fentanyl, and clonidine.[9,10,17,18,20] Lignocaine is an effective, safe and long established agent used to blunt the hemodynamic response to tracheal intubation.
This study was planned to compare the efficacy of IV dexmedetomidine infusion and IV lignocaine in attenuating this hemodynamic responses to laryngoscopy and intubation. We hypothesized that dexmedetomidine would blunt the hemodynamic response to tracheal intubation safely and equally or even more effectively than lignocaine.
METHODOLOGY
After ethical committee approval, the present study was conducted in a randomized double blinded manner in the department of anesthesiology, in our tertiary care hospital over a period of one year -October 2014 till September 2015. ASA grade I and II, normotensive patients of either sex between age group of 18-60 years, planned to undergo elective surgery under general anesthesia, were enrolled in the study. Patients were randomized into three equal groups of 40 patients each using sealed envelope technique (Figure 1). Blinding was done using coded syringes.
Group A (lignocaine group) patients were administered 20 ml normal saline (NS) as an infusion through syringe pump at a rate of 120 ml / hour, 10 min before induction followed by lignocaine 1.5 mg/kg in 10 ml NS over one minute, 2 min before induction.
Group B (dextmedetomidine group) patients were administered dextmedetomidine 1 µ/kg in 20 ml NS through syringe pump at a rate of 120 ml/h, 10 min before induction and 10 ml of NS IV over one minute, 2 min before induction.
Group C (control group), patients were administered 20 ml NS infusion through syringe pump at a rate of 120 ml/h, 10 min before induction and 10 ml of NS IV over one minute, 2 min before induction.
Patients with history of hypertension, renal disease, ischemic heart disease, AV blocks, endocrine diseases, seizure disorders, patients on sympatholytic drugs, with a history of anaphylaxis and allergy to the study drugs, with anticipated difficult airway (modified Mallampati grade ≥ 3), pregnant patients and patients requiring throat packing during surgery were excluded from the study.
After establishing IV line in preoperative area, all patients were premedicated with inj midazolam 1 mg IV, 30 min prior to shifting to operating room.
In the operating room, all patients were preloaded with 500 ml of normal saline. After a stabilizing time of 5 min, a baseline readings of heart rate (HR) per min, systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), oxygen saturation of arterial blood (SpO2) and electrocardiogram (ECG) rhythm were recorded (T0). Patients were monitored at one minute intervals till ten minutes after intubation. Infusion of solution in 20 ml syringe was started using syringe pump @120 ml/hr. At the end of 8th minute (T8) of starting the infusion, the second solution in 10 ml syringe was injected over one minute. The patient was preoxygenated with 100% oxygen during this period. Induction was done with propofol (1%), 2 mg/kg and intubated using suxamethonium 1.5 mg/kg by the senior anesthesiologist present. Laryngoscopy and intubation times was recorded. Cormack-Lehane grade of the laryngoscopic view was noted. Anesthesia was maintained with isoflurane in nitrous oxide (60%), oxygen (40%) and vecuronium bromide 0.08 mg/kg. Patient was put on intermittent positive pressure ventilation using a closed circuit. Anesthesia was reversed with neostigmine 0.05 mg/kg and glycopyrrolate 0.01 mg/kg at the end of surgery.
The study parameters, e.g. HR, SBP, DBP, and MAP were observed at;
T0- base line after entering the operating room
T10 –at the end of infusion with syringe pump i.e. 10 min
Ti –at the time of intubation
T1i to T10i – after 1 min of intubation till 10 min
Statistical analysis: Sample size was calculated based on results of study done by Sulaiman S et al[22] using fall in mean HR per min following dexmedetomidine drug therapy. This required 25 patients in each group for results to be significant (with effect size was calculated as 0.76, α = 0.05 and power of study 95%). Sample size was taken to be 40 to cover any dropouts during study. The data collected was entered into an MS Excel spreadsheet and then converted into SPSS version 16 for further analysis. Chi square tests and ANOVA were used for statistical analysis. P value < 0.05 was taken to be significant and p-value < 0.0001 as highly significant.
RESULTS
All the three groups were comparable in terms of age, gender, weight distribution, time taken to laryngoscopy and intubation, Mallampati grade and Cormack-Lehane grade. (Table 1).
Table 1: Demographic and airway parameters. *P value > 0.05 – not significant
| Parameter | Group C
(n = 40) |
Group A
(n = 40) |
Group B
(n = 40) |
P value
A&B |
| Age in years (Mean ± SD) | 35.90 ± 13.50 | 42.15 ± 13.14 | 36.05 ± 11.39 | 0.091* |
| Weight (kg) (Mean ± SD) | 57.25 ± 12.56 | 60.23 ± 10.68 | 60.25 ± 12.84 | 1.000* |
| Time for laryngoscopy and intubation (sec) | 38.50 ± 2.25 | 39.13 ± 2.16 | 38.68 ± 2.75 | 0.680* |
| Sex (Male/ Female) | 14 / 26 | 15 / 25 | 11 / 29 | 0.469* |
| Mallampati grade (I/II) | 20/20 | 20/20 | 22/18 | 0.654* |
| Cormack-Lehane grade (I/II) | 23/17 | 24/16 | 22/18 | 0.651* |
The mean age varied from 35.90 ± 13.50 to 42.15 ± 13.14 years in three groups and the overall range was from 18-60 years. The patients comprised of 40 males and 80 females. The mean weight varied from 57.25 ± 12.56 kg to 60.25 ± 12.84 kg (Table 1). Changes in HR, MAP SBP, and DBP in all the three groups at different time interval are shown in Figures 1-4.
Figure 1: Changes in HR at different time intervals in all three groups
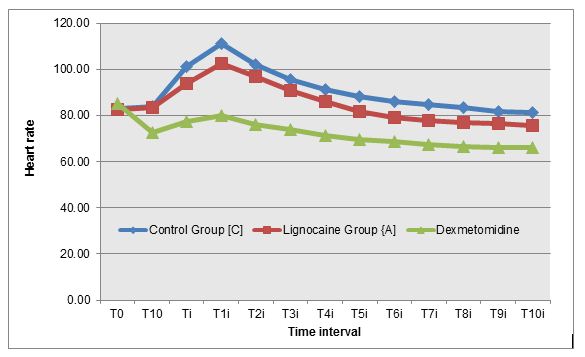
Figure 2: Changes in MAP at different time intervals in all three groups
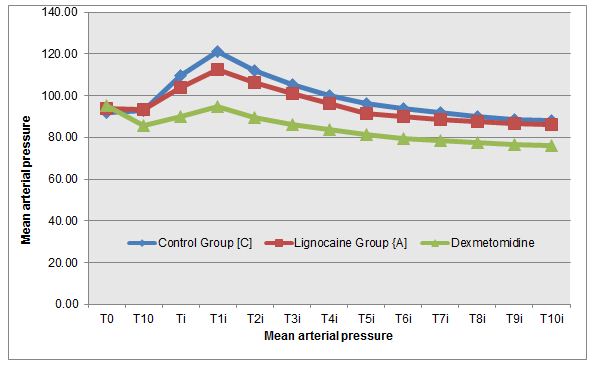
Figure 3: Changes in DBP at different time intervals in all three groups
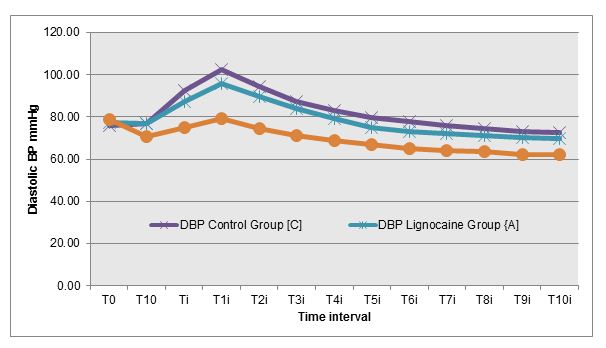
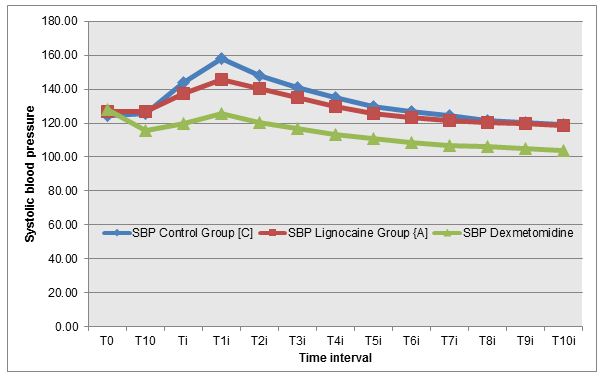
Figure 4: Changes in SBP at different time intervals in all three groups
DISCUSSION
Stress response due to laryngoscopy and intubation is a potentially hazardous side effect of anesthesia technique. Sudden hypertension and increased heart rate results in increased load on the heart and disturbs oxygen demand supply ratio. It may presents as rate & rhythm abnormalities, intracranial hemorrhage, end organ dysfunction of kidney and brain especially so in compromised patient i.e. hypertensive, diabetic patients, patients with coronary artery disease, renal disease and cerebrovascular disease to name a few.
Intravenous lignocaine prevent cardiovascular response to endotracheal intubation by increasing depth of anesthesia, peripheral vasodilatation and direct cardiac depression. Lignocaine has been used to blunt pressor response to intubation [4,5] because of its short duration, antiarrhythmic effects and its effects on synaptic transmission.
Dexmedetomodine, an alpha-2 adrenergic agonist, increases the hemodynamic stability by altering the stress induced sympathoadrenal responses to intubation [17,23] without affecting intraoperative cardiovascular stability. [24] It decreases intraoperative anesthetic requirement and has significant opioid and anesthetic agent sparing properties.
Present study was planned to compare these two agents along with control group in regards to their efficacy to attenuate cardiovascular response to endotracheal intubation.
Abou Madi et al [4] studied cardiovascular responses to laryngoscopy and tracheal intubation following small (0.75 mg/kg 1%) and large (1.5 mg/kg 2%) intravenous dose of lidocaine. They found that smaller dose prevents only the rise in SBP but larger dose provides borderline protection against any hypertension and tachycardia. We used 1.5 mg/kg 2% lignocaine and found that at time of laryngoscopy and intubation (Ti), both lignocaine group and control group recorded a statistically significant increase in mean heart rate by 13.40% and 21.87% respectively from baseline value (T0) (p value –0.000). Although lignocaine recorded a statistically significant maximum increase in mean heart rate from the baseline but it was both lower in magnitude (24.03% vs. 33.78 %) as well as persisted for a shorter duration as compared to control group (4 min vs. 6 min) (Figure 1). Lignocaine group and control group recorded a statistically significant increase in mean MAP by 10.72% and 18.96%respectively from baseline value (T0) (P value – 0.000) at time of laryngoscopy and intubation (Ti). Though lignocaine recorded a statistically significant maximum increase in mean MAP from the baseline but it was both lower in magnitude (10.72% vs 18.96%) and persisted for a shorter duration as compared to control group (4 min vs. 5 min)( Figure 2). Similar trends were seen in SBP and DBP also (Figures 3&4).
Feng et al [6] compared three drugs, lidocaine (2 mg/kg), fentanyl (3 µg/kg) and esmolol (2 mg/kg) for hemodynamic responses to laryngoscopy and tracheal intubation. After intubation, the incidence of tachycardia was 15% in esmolol group, 85% in control group, 75% in lidocaine group and 55% in fentanyl group. They concluded that lidocaine had no effect to blunt adverse hemodynamic response to laryngoscopy and intubation. In present study, although lignocaine doesn’t completely provide any protection against tachycardia but still statistically significant maximum increase in mean heart rate from the baseline was both lower in magnitude (24.03% vs. 33.78 %) and persisted for a shorter duration in lignocaine group as compared to control group (4 min vs. 6 min) (Figure 1).
Kalakeri et al [25] used dexmedetomidine (1µg/kg) to attenuate cardiovascular stress response to endotracheal intubation in patients undergoing cardiac surgery and found that there was statistically significant decrease in HR, SBP, DBP and MAP compared to basal value after drug infusion and before induction. SBP, DBP and MAP remained lower than the baseline value even after the intubation. The incidence of bradycardia requiring active intervention was 4.34%. In present study significant decrease in SBP, DBP, MAP and HR was seen in dexmedetomidine group (Figures 1-4). At the time of intubation (Ti) dexmedetomidine group recorded a statistically highly significant decrease in mean heart rate by 9.28% from the baseline value (T0) (p value – 0.000). Maximum fall in mean MAP was 19.80% at 10 min after intubation (T10i) which was statistically highly significant (P value- 0.000). In present study no patient required active treatment for bradycardia. High incidence of treatment requiring bradycardia in their study could be due to inclusion of hypertensive patients on metoprolol 25 mg in their study.
Pipanmekaporn T et al [26] studied the effects of dexmedetomidine on hemodynamic changes to double lumen endotracheal intubation (DLT) and found that during and after DLT intubation the mean SBP, DBP and MAP in the control group were significantly higher than those of the dexmedetomidine group. In present study dexmedetomidine group recorded no incidence of increase in mean SBP, DBP, and MAP from the baseline throughout the study and remained below the baseline value through the entire time intervals after intubation (Figures 2-4). Maximum fall in mean MAP was 19.80% at 10 min after intubation (T10i) which was statistically highly significant (p < 0.001) but not significant clinically (fall < 25%).
In a recent study, Sebastian et al[27] compared two different doses of dexmedetomidine (0.5 µg/kg and 0.75 µg/kg) and found that a dose of 0.75 µg/kg was better in attenuating stress response to intubation.
Gulabani et al [7] used and compared lignocaine (1.5 mg/kg) with two different doses of dexmedetomidine (0.5 µg/kg and 1 µg/kg). They concluded that dexmedetomidine 1 μg/kg adequately attenuates the hemodynamic response to laryngoscopy and endotracheal intubation when compared with dexmedetomidine 0.5 μg/kg and lignocaine 1.5 mg/kg. These results are in accordance with results of the present study.
On intergroup comparison of lignocaine and dexmedetomidine, we could find a significantly better control of HR (with lignocaine showing 13.40% increase in HR and dexmedetomidine showing 9.28 % decrease in HR at the time of intubation) and MAP (with lignocaine showing 10.72% increase in MAP and dexmedetomidine showing 5.49 % decrease in MAP at the time of intubation).
No untoward side effects were observed during the entire course of study in all the groups. Number of patients having tachycardia are 37 in group C (control group), 22 in group A (lignocaine group) and bradycardia was experienced by 4 patients in group B (dexmedetomidine group); however, no patient required active treatment for the same.
Thus, dexmedetomidine provided better protection against untoward hemodynamic side effects of intubation and laryngoscopy as compared to lignocaine. Lignocaine also blunts the response as compared to control but not as effectively as dexmedetomidine.
LIMITATIONS
This study has some inherent limitations. We terminated the study at 10 min post intubation but the effects of study drugs, particularly that of dexmedetomidine, can persist for long and can have important clinical implications. Future studies with extended monitoring and supplement measurements of catecholamine levels can be planned to further evaluate.
CONCLUSION
Based upon the results of our study, we conclude that intravenous dexmedetomidine is better than lignocaine in attenuating the hemodynamic response to direct laryngoscopy and endotracheal intubation. Intravenous dexmedetomidine infusion in doses used (1 µg/kg) is safe and effective alternative to lignocaine (1.5 mg/kg) in blunting this stress response.
Conflict of interest: Nil declared
Authors contribution: GS, HK, SA, GS: Concepts, Design, Literature search, Data acquisition, Statistical analysis, Manuscript preparation/editing
AS, AJ, HA: Literature search, Data acquisition, Data analysis, Statistical analysis, Manuscript preparation, Manuscript review
REFERENCES
- Low JH, Harvay JT, Pyrs Roberts C, Dagnino J. Studies of anesthesia in relation to hypertension. Br J Anaesth 1986;58:471-477. [PubMed]
- Phillipp T, Distler A, Cordes U. Sympathetic nervous system and blood pressure control in essential hypertension. Br J Anaesth 1978;45:671.
- Hamill JR, Bedford RF, Weaver DC, Colohan AR. Lidocaine before endotracheal intubation: intravenous or laryngotracheal? Anesthesiology 1981;55:578. [PubMed] [Free full text]
- Abou-Madi MN, Keszler H, Yocoub JM. Cardiovascular reactions to laryngoscopy and tracheal intubation following small and large intravenous dose of lidocaine.CandAnaesthSoc J 1977;24:9-12. [PubMed]
- Lev R, Rosen P Prophylactic lidocaine use preintubation: a review. J Emerg Med. 1994; 12(4):499-506. [PubMed]
- Feng CK,Chan KH, Liu KN, Or CH, Lee TY. A comparison of lidocaine, fentanyl, and esmolol for attenuation of cardiovascular response to laryngoscopy and tracheal intubation. Acta Anaesthesiol Scand 1996;34(2):61-67. [PubMed]
- Gulabani M, Gurha P, Dass P, Kulshreshtha N. Comparative analysis of efficacy of lignocaine 1.5 mg/kg and two different doses of dexmedetomidine (0.5 μg/kg and 1 μg/kg) in attenuating the hemodynamic pressure response to laryngoscopy and intubation. Anesth Essays Res.2015 ;9(1):5-14. doi: 10.4103/0259-1162.150167. [PubMed] [Free full text]
- Coleman AJ, Jordan C. Cardiovascular responses to anesthesia: influence of beta adrenoreceptor blockade with metoprolol. Anaesthesia 1980;35:972-978. [Free full text]
- Reddy SV, Balaji D, Ahmed SN. Dexmedetomidine versus esmolol to attenuate the hemodynamic response to laryngoscopy and tracheal intubation: A randomized double-blind clinical study.Int J Appl Basic Med Res. 2014 ; 4(2): 95–100. doi: 10.4103/2229-516X.136788. [PubMed] [Free full text]
- Yavascaoglu B, Kaya FN, Baykara, Bozkurt M, Korkmaz S.. A comparison of esmolol and dexmedetomidine for attenuation of intraocular pressure and haemodynamic responses to laryngoscopy and tracheal intubation. Eur J Anaesthesiol. 2008;25:517-9. doi: 10.1017/S0265021508003529. [PubMed]
- Fassoulaki A, Kaniaris P. Intranasal administration of nitroglycerine attenuates pressor response to laryngoscopy and intubation of trachea. Br J Anaesth 1983;55:49-52. [PubMed]
- Mikawa K, Obara H, Kusunoki M. Effect of nicardipine on cardiovascular response to tracheal intubation. Br J Anaesth 1990;64:240-242. [PubMed]
- Puri GD, Batra YK. Effect of nifedipine on cardiovascular response to laryngoscopy and intubation. Br J Anaesth 1988;60(5):579-581. [PubMed]
- Kautto UM. Attenuation of circulatory response to laryngoscopy and intubation by fentanyl. Acta Anaesthesiol Scand 1982;26(3):217-221. [PubMed]
- Black TE, Kay B, Healy TE. Reduction of haemodynamic response to laryngoscopy and intubation.A comparison of alfentanil with fentanyl. Anaesthesia 1984;39(9):883-887. [PubMed] [Free full text]
- Salihoglu Z, Demiroluk S, Demirkiran. Comparison of effects of remifentanil, alfentanil and fentanyl on cardiovascular responses to tracheal intubation in morbidly obese patients. Eur J Anaesthesiol 2002;19:125-128.
- Scheinin B, Lindgren L, Randell T, Scheinin H, Schenin M. Dexmedetomidine attenuates sympatoadrenal response to tracheal intubation and reduces the need for thiopentone and postoperative fentanyl. Br J Anaesth 1992; 68:126-131. [PubMed]
- Suparto, Flores OC, Angela CA, Layusa A randomized controlled trial on the effectiveness of dexmedetomedine versus fentanyl in attenuating the sympathetic response in laryngoscopy and endotracheal intubation. MajKdot Indon. 2010;3(60)
- Fassoulaki A, Melemeni A, Paraskeva A, Petropoulos G. Gabapentin attenuates the pressor response to direct aryngoscopy and tracheal intubation Br J Anaesth 2006;96(6):769–773. [Free full text]
- Agarwal S, Gupta K, Singh VP, Sharma D, Pandey MN. Comparative evaluation of dexmedetomidine with clonidine as premedication for attenuation of hemodynamic responses during laryngoscopy and endotracheal intubation under general anesthesia. Int J Res Med Sci 2016;4:4026- 32. [Free full text]
- Sulaiman S, Karthekeyan RB, Vakamudi M, Sundar AS, Ravullapalli H, Gandham R. The effects of dexmedetomidine on attenuation of stress response to endotracheal intubation in patients undergoing elective off-pump coronary artery bypass grafting. Ann Card Anaesth 2012;15:39-43. doi: 10.4103/0971-9784.91480. [PubMed] [Free full text]
- Jaakola ML, Ali-Melkkila T, Kanto J, Kallio A, Scheinin H, Schenin M. Dexmedetomidine reduces intraocular pressure , intubation responses, and anaesthetic requirements in patients undergoing ophthalmic surgery.Br J Anaesth 1992; 68:570-575. [PubMed]
- Keniya VM, Ladi S, Naphade R. Dexmedetomidine attenuates sympathoadrenal response to tracheal intubation and reduces perioperative anaesthetic requirement. Ind J Anaes 2011; 55(4):352–357. doi: 10.4103/0019-5049.84846. [PubMed] [Free full text]
- Kalakeri S, Suresh C. Dexmeditomidine as an adjunct to anaesthetic induction to attenuate hemodynamic response to endotracheal intubation in patients undergoing CABG Int J Curr Res Aca Rev 2015;3(4):101-117. [Free full text]
- Pipanmekaporn T, Punjasawadwong Y, Charuluxananan S, Lapisatepun W, Bunburaphong P.The effect of prophylactic dexmedetomidine on hemodynamic disturbances to double-lumen endotracheal intubation: a prospective, randomized, double-blind, and placebo-controlled trial . Anesthesiol Res Pract. 2013; 2013: 236089. doi: 10.1155/2013/236089. [PubMed] [Free full text]
- Sebastian B,Talikoti AT, Krishnamurthy D. Attenuation of haemodynamic responses to laryngoscopy and endotracheal intubation with intravenous dexmedetomidine: A comparison between two doses Indian J Anaesth. 2017 Jan;61(1):48-54. doi: 10.4103/0019-5049.198404. [PubMed]

