Saad Ur Rehman1, Muhammad Zafar Khan2, Yaasir Ijaz Ahmed2, Abdul Rehman3
1Fellow;2Consultant; 3Resident
Department of Anesthesiology and Pain Medicine, Shaukat Khanum Memorial Cancer Hospital & Research Centre, Lahore, (Pakistan).
Correspondence: Dr. Saad Ur Rehman, MD, FCPS, Fellow, Department of Anesthesiology and Pain Medicine, Shaukat Khanum Memorial Cancer Hospital & Research Centre, Johar Town, Lahore 54000, (Pakistan); Work Phone: +92-42-5905000 ext. 5113; Cell: +92-343-4545963; Email: saad_rehman@yahoo.com
ABSTRACT
Objectives: Treatment of cancer pain presents a challenging problem. Up to 90% of cancer patients can be treated with conventional pharmacological therapy. The remaining 10% of patients require additional interventions for management of their pain. Intrathecal chemical neurolysis(ICN) is a beneficial intervention in management of cancer pain. The primary objective of this study was to study the effects of pain relief of ICN on the Visual Analogue Score (VAS) of patients with metastatic cancer disease on palliative therapy.
Methodology: This retrospective case series was performed at Shaukat Khanum Memorial Cancer Hospital & Research Centre, Lahore (Pakistan). We reviewed the medical records of thirty nine patients who underwent ICN at our institute.The mean VAS before procedure was 7.8.
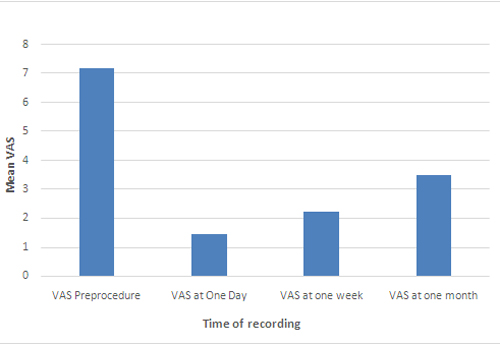
Results: After ICN, mean pain scores fell to 1.44 at first day, 2.23 at first week and 3.5 at first month. Mean opioid analgesic free period was 23.5 days.
Conclusion: We conclude that ICN is a beneficial procedure for selected patients with intractable refractory pain.
Key words: Cancer pain; Pain intervention; Intrathecal chemical neurolysis
Citation: Rehman SU, Khan MZ, Ahmed YI, Rehman A. Intrathecal chemical neurolysis for intractable cancer pain: a retrospective audit of 39 patients at a specialized cancer centre. Anaesth Pain & intensive Care 2015;19(3):287-291
INTRODUCTION
Pain is one of the most common sequelsof cancer.1Up to 40% of patients suffer from pain and the incidence and severity increases with advanced stages of cancer.1-3 Not only is it feared by patients but it is a burden on health care costs and resources.In spite of the advances in pain management up to 46% of patients on palliative treatment have inadequate pain control at death.1,4The World Health Organization (WHO) 3-tiered ladder for management of pain control remains the guideline for managing cancer pain; however, 10-14% of patients suffer from significant pain even when these guidelines are applied. For relief of pain in such patients, a fourth step to the WHO analgesic ladder has been added which includes advanced interventional approaches 1,5. There are a variety of interventional techniques, which can be grossly divided into Neuraxial blocks & Neurolytic blocks. As the names imply nerve fibers are blocked in the former and destroyed in the latter interventions.
Intrathecal Chemical Neurolysis (ICN) is an important intervention in treatment of cancer pain1,2,6. It is useful in patients with terminal cancer pain and pain refractory to pain medication. Some of the major advantages of ICN include fewer follow-ups as compared to regional analgesic techniques using continuous neuraxial drug delivery and greater cost-effectiveness for patients.2 However like other interventional techniques it comes with its share of complications.6
On local literature search, studies are limited to case reports and role of regional interventions.7,8 We present a case series of thirty nine patients with metastatic cancer who underwent ICN for management of their pain and discuss the results noted.
Our hypothesis was that ICN would decrease the VAS of patient’s pain as compared to before procedure. The primary objective of this study was to study the effects of pain relief of ICN on the VAS of patients with metastatic cancer disease on palliative therapy.
METHODOLOGY
This retrospective study was conducted in the Department of Anesthesiology & Pain Medicine, Shaukat Khanum Memorial Cancer Hospital Lahore and is presented as a case series.All patients with metastatic cancer disease on palliative chemotherapy,who underwent ICN procedures fulfilling inclusion and exclusion criteria were studied. Patients with incomplete medical records and patients lost to follow up were exluded.
Data collection: The medical records ofall patients who underwent ICN at our institute between November 2008 and February 2011 were reviewed.All patients had metastatic disease with poor prognosis. The details of primary malignancy and demographics were noted. Patients were considered for ICN when they had pain in the lumbosacral nerve route distribution with failure to pharmacological therapy i.e. oral morphine more than 10 mg per day. The mean score on the Visual Analogue Score (VAS) with use of opioid therapy was 7.8 out of 10.
The details of pain, site, radiation, associated symptoms and analgesic drugs were documented on a form along with details of procedure, the dermatomes blocked and any complications.
Procedure: All procedures were performed in the operating room by the same anesthesia consultant. After taking informed consent patients were shifted to the operating room. Basic monitors including pulse-oxymetery, E.C.G and non-invasive blood pressure were applied and intravenous access was established. The distribution of pain was co-related with a dermatome chart and the nerve roots to be blocked were determined. Patients were placed in lateral spinal position with painful side up. After aseptic measures a 25 G Quincke cutting spinal needle was introduced till subarachnoid space was reached and there was free flow of CSF. At this point patients were rolled anteriorly 45 degree so that the dorsal root was at the highest point and strapped so that they would remain in this position. A tuberculin syringe containing absolute alcohol was injected in 0.1 ml increments to a total of 0.4-0.7 ml. Patients were kept in that position for 15 min, and kept for monitoring after procedure. They were discharged on the same day after assessment by anesthetist. When bilateral procedure was required, the more painful side was treated first and the other side two weeks later. Those patients who were pain free after the first procedure for at least two weeks were offered a repeat ICN procedure. 16 (41%) patients underwent repeat procedures and a total of sixty seven ICN procedures were performed.
Follow up data after procedures were extracted from patient visit notes on first post procedure day, one week and one month. The degree of pain relief was recorded with VAS by the anesthesia resident who had assessed the patient pain earlier, at first post procedure day, one week and one month.
RESULTS
A total of forty one patients with metastatic disease refractory to pain medication received 68 procedures during the study period. Two patients wereexcluded as medical records were incomplete. The data of thirty nine patients were studied. Demographic data of the patients are given in Table 1.
Table 1: Patient Demographic Data (n=39)
|
Parameter |
Value |
| Males |
16 (41.02) |
| Females |
23 (58.9) |
| Age (Mean ± SD) |
46.8 ± 3.14 |
|
Primary tumor site |
|
| Breast |
14 (35.9) |
| Bone |
5 (12.8) |
| Gynecological |
4 (10.3) |
| Rectum and Anal Canal |
3 (7.7) |
| Lung |
4 (10.3) |
| Lymphoma |
2 (5.1) |
| Pancreas, Prostate, Bladder, Kidney, Larynx, Vascular, Primary unknown |
1 each (2.6) |
| Total |
39 (100) |
Involved dermatomes are shown in Table 2.
Table 2: Involved dermatomes
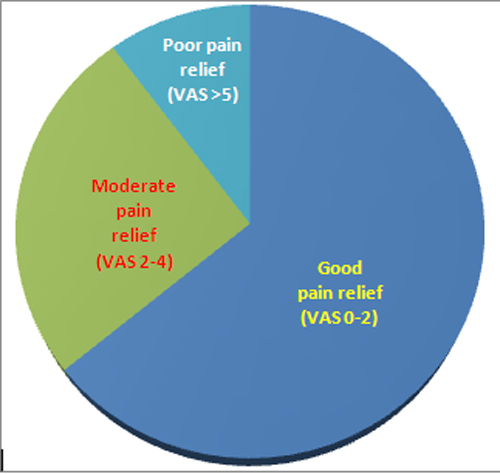
25 (64%)patients had significant pain relief (VAS 0-2/10) after the procedure, while 10 (25.6%) patients had moderate pain relief (VAS 2-4/10) and 4 (10.2%) had no pain relief after the procedure. Mean VAS scores were 1.44/10 on first day, 2.23/10 at one week and 3.5/10 at one month follow up (Figure 1 & 2).
Figure 1: Visual Analog Scores (VAS) pre- and post-procedure
Figure 2: Quality of pain relief immediately after procedure
The mean analgesic free period was 25.8 days. Patients were started on rescue analgesic oral morphine when their VAS was more than 3 and dose was titrated to effect.
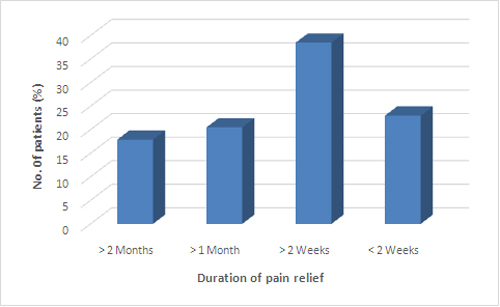
The duration of significant pain relief was more than two months in 17.9% (7 patients), more than one month in 20.5% (8 patients), more than 2 weeks in 38.4% (15 patients) and less than 2 weeks in 23% (9 patients) (Figure 3).
Figure 3: Duration of pain relief
Complications observed were numbness in 20 (51.2%), temporary weakness in 17 (43.5%), urinary and fecal incontinence in 6 (15.3%) and paralysis in 1 (2.5%) patient. None of the patients developed post dural puncture headache or meningitis. Results are summarized in Table 3.
Table 3: Complications
|
Complications |
N (%) |
| Numbness |
20 (51.2) |
| Paresthesias |
14 (35.8) |
| Dysesthesia |
9 (23.09) |
| Temporary weakness |
17 (43.5) |
| Paralysis |
1 (2.5) |
| Urinary, fecal incontinence |
6 (15.3) |
| Meningitis |
0 (0) |
| Post dural puncture headache |
0 (0) |
| Treatment failure |
4 (10.2) |
DISCUSSION
Intrathecal Alcohol injection for relief of intractable pain was first described by Dogliotti in 1931.10This procedure provides pain relief by destroying the posterior sensory root axons while protecting the motor roots. The injection of alcohol in the dorsal root causes demyelination and degeneration of the nerve fibers which results in pain relief11. Other agents like phenol-glycerol have been used for ICN with similar results.12,13The efficacy of ICN in relief of cancer pain is documented however it has not gained as much popularity after the advent of Implantable drug delivery systems.1,11,14 Nevertheless it is a beneficial intervention in advanced, progressive and irreversible illness.1,11
ICN is inexpensive and easy to perform for anesthetists and the procedure is well tolerated by patients. They do not require admission to hospital after the procedure and it can be performed as a day case. Follow ups are minimal and patients can be followed up by phone or by weekly appointments. These benefits make ICN effective and practical.
The complications associated with ICN include short duration of effect, Post Dural puncture headache (PDPH), meningitis, weakness of limbs and rectal/bladder dysfunction1,7,11,15. There are two reasons for the short duration of action. As the tumor progresses it involves more and more nerve fibers which increases the pain. Secondly the axons destroyed by alcohol undergo regeneration leading to pain recurrence. Post Duralpuncture headache and meningitis are potential complications whenever the Dura is punctured. Weakness of limbs and urine/fecal incontinence is due to spread of alcohol to anterior motor nerve roots. These are frequent and unavoidable.
Our patients had similar percentage of complications as observed in previous studies however we did not observe any PDPH or meningitis.Duration of pain relief and recurrence remains a problem. The mean pain relief after procedures is not expected to be more than 2-3 months, almost all of our patients required opioids after 2 months of procedure. However this procedure is easy to perform and can be repeated if required.Forty one percent of our patients underwent repeat procedures after they developed recurrence. Four patients had no effect from this procedure. We are not aware of the cause of that, it could be due to migration of needle or erroneous spread of alcohol. Weakness of limbs and urinary, fecal incontinence is an inevitable problem and incidence rates are same as previous studies.2,11,12 Patients should be informed and counseled about these problems before hand. Permanent neurological injury and death is also a serious concern when injecting neurolytic agents into subarachnoid space12and we advocate that this procedure be limited to patients with intractable pain and end stage disease.
The most important factor in the decision of choice of ICN is life expectancy. It should be limited to patients with advanced cancer with poor prognosis and short life span. Some authors advocate it for patients with life expectancy less than one year. The potential benefits should be weighed against the expected complications while making the decision. The patient and family should be counseled about the limitations and benefits of the procedure and involved in the decision making process.
CONCLUSION
ICN can be a beneficial procedure for pain relief of patients with expected short life span with intractable pain refractory to pain medications. Although it is associated with complications, we believe it is an important adjuvant to the interventions for cancer pain.
REFERENCES
- Christo P, Mazloomdoost D. Interventional pain treatments for cancer pain. Ann N Y Acad Sci. 2008;1138(1):299-328. [PubMed]doi: 10.1196/annals.1414.034.
- Tay W, Ho K. The role of interventional therapies in cancer pain management. Ann Acad Med Singapore. 2009;38(11):989-997. [PubMed][Free full text]
- Goudas L, Bloch R, Gialeli-Goudas M, Lau J, Carr D. The epidemiology of cancer pain. Cancer Invest. 2005;23(2):182-190. [PubMed]
- Hui D, Elsayem A, De la Cruz M, Berger A, Zhukovsky DS, Palla S. Availability and integration of palliative care at US cancer centers. JAMA. 2010;303(11):1054.[PubMed][Free full text]
- Azevedo São Leão Ferreira K, Kimura M, Jacobsen Teixeira M. The WHO analgesic ladder for cancer pain control, twenty years of use. How much pain relief does one get from using it?Support Care Cancer. 2006;14(11):1086-1093. [PubMed][Free full text]
- Kongsgaard U, Bjørgo S, Hauser M. Neurolytic blocks for cancer pain–still a useful therapeutic strategy. Tidsskr Nor Laegeforen. 2004;124(4):481-483. [PubMed][Free full text]
- Iqbal M, Khan M, Faruqui Z. Contralateral limb weakness after intrathecal chemical neurolysis for cancer pain. Anaesth Pain & Intensive Care. 2010;14(2):109-111. [Free full text]
- Anjum Q. Role of neuromodulation in the treatment of opioid poorly responsive cancer pain. JCPSP. 2002;12(3):189-194.
- Ferreira-Valente MA, Pais-Ribeiro JL, Jensen MP. Validity of four pain intensity rating scales. Pain 2011;152(10):2399-404 [PubMed]
- Dogliotti A. Traitement des syndromes douloureux de la périphérie par l’alcoolisation sub-arachnoidienne des racines postérieures à leur émergence de la moelle épinière Press Med 1931;29:1249–1252.
- Koyyalagunta D, Burton A. The role of chemical neurolysis in cancer pain. Curr Pain Headache Rep. 2010;14(4):261-267. [PubMed]doi: 10.1007/s11916-010-0123-9.
- Candido K, Philip C, Ghaly R, Knezevic N. Transforaminal 5% phenol neurolysis for the treatment of intractable cancer pain. AnesthAnalg. 2010;110(1):216-219. [PubMed]
- Watanabe A, Yamakage M. Intrathecal neurolytic block in a patient with refractory cancer pain. J Anesth. 2011;25(4):603-605. [PubMed]
- Perez M, Pulley S. Intrathecal analgesia in cancer pain. Techniques in Regional Anesthesia and Pain Management. 2010;14(1):10-18. [Online] DOI:http://dx.doi.org/10.1053/j.trap.2009.12.004
- McGarvey M, Ferrante F, Patel R, Maljian J, Stecker M. Irreversible spinal cord injury as a complication of subarachnoid ethanol neurolysis. Neurology. 2000;54(7):1522-1524.[PubMed]