Tanzeela Firdous, MBBS, FCPS1, Maqsood Ahmed Siddiqui, MCPS, FCPS, MSc (Pain Medicine)2, Safia Maqsood Siddiqui, MBBS, FCPS3
1Consultant Anesthesiologist, Shaukat Khanum Memorial Hospital & Research Centre, Lahore (Pakistan)
2Consultant Anesthesiologist & Pain Physician, Department of Anesthesiology, Surgical Intensive Care & Pain management Centre, Peoples University of Medical & Health Sciences Hospital Nawabshah, Shaheed Benazirabad (Pakistan)
3Associate Professor, Department of Gynaecology and Obstetrics, Peoples University of Medical & Health Sciences Hospital Nawabshah, Shaheed Benazirabad (Pakistan)
Correspondence: Dr. Maqsood Ahmed Siddiqui, Banglow No: D-2, Old Doctors Colony near Hamid Ali Club, Court Road Nawabshah, Shaheed Benazirabad (Pakistan); Cell: 03337027717, 03003212517; E-mail:drmaqsood70@yahoo.com
ABSTRACT
Objective: Post dural puncture headache (PDPH) is one of major complications of spinal anesthesia. There are two approaches to administer spinal anesthesia i.e. median and paramedian. We conducted this study to compare the frequency of PDPH after spinal anesthesia for cesarean section with median versus paramedian approach using 25 gauge pencil point needle.
Methodology: This randomized controlled trial was conducted at Departments of Anesthesiology, Surgical Intensive Care & Pain Management Centre as well as Gynecology & Obstetrics, Peoples University of Medical & Health Sciences, Nawabshah, Benazirabad (Pakistan). One hundred and twenty females underwent elective cesarean section under spinal anesthesia were enrolled. After informed written consent, the parturients were randomly divided into two equal groups by lottery method; Group A patients received spinal block with median approach and Group B patients received it with paramedian approach. All spinal blocks were performed with 25 gauge pencil point needle. The patients were asked about the presence or absence of headache through Visual Analogue Scale (VAS) in the next 72 hours.
Results: In median approach (Group A), 3 patients (5%) had PDPH; whereas in paramedian approach (Group B) only 1 patient (1.6%) had PDPH. All the patients were of younger age and low parity. They developed PDPH within 24 -48 hours which was of mild to moderate in degree on VAS and relieved by rest, plenty of fluids and simple analgesics containing caffeine in mild case. While strong analgesics and muscle relaxants were added in cases of moderate PDPH. PDPH was relieved within 2-3 days in all cases without any complication. The difference was statistically insignificant (p-value=0.30).
Conclusion: Paramedian approach is better than median approach in terms of reduction in the frequency of PDPH, though the results were statistically insignificant.
Key words: Median; Parmedian; Post dural puncture headache; Anesthesia, Spinal; Cesarean Section; Pencil-point spinal needleAnesthesia, Spinal, Cesarean Section, Post-Dural Puncture Headache
Citation: Firdous T, Siddiqui MA, Siddiqui SM. Frequency of post dural puncture headache in patients undergoing elective cesarean section under spinal anesthesia with median versus paramedian approach. Anaesth Pain & Intensive Care 2016;20(2):165-170
Received: 13 January 2016; Reviewed: 16 February, 30 March 2016; Corrected: 5 April 2016; Accepted: 10 June 2016
INTRODUCTION
Spinal anesthesia is a form of central neuraxial blockade employed for various surgical procedures of lower abdominal, inguinal, urogenital, rectal and lower limb surgeries. Spinal anesthesia is easy to perform and has rapid and intense onset. Spinal anesthesia is related with decreased incidence of venous thrombosis and pulmonary embolism, reduced bleeding and transfusions requirements and is safe for various procedures of upper abdomen in patients with lung diseases if managed properly but still there is a risk of complications. Some other benefits include earlier return of bowel function following surgery, early mobilization and decreased patient discomfort and hospital stay. When used for cesarean section, spinal anesthesia allows a mother to remain awake and experience the birth of her child, early breast feeding and prevents the incidents of gastric contents aspiration and failed endotracheal intubation.1,2,3,4
Post dural puncture headache (PDPH) is one of the widespread complications of spinal anesthesia and occurs in 32% of patients carrying a considerable morbidity. Also the associated symptoms last for several days, at times severe enough to impair patient’s quality of life.5 Different modalities have been tried to decrease the element of post dural puncture headache. However, despite taking best preventive measures, post dural puncture headache may still occur.6 The reason of post dural puncture headache following spinal anesthesia varies with characteristics of individual patients, the type of spinal needle and the technique or approach used.7 The two approaches used to administer local anesthetics in spinal anesthesia are the median and the paramedian.8 The median approach involves passage of the needle through supraspinous, interspinous ligaments and ligamentum flavum, while the paramedian approach avoids supra and interspinous ligaments and hits ligamentum flavum directly after passing through para spinal muscles.9
The frequency of PDPH is directly linked to the diameter of needle that is used to pierce the dura mater. Even though needle punctures with relatively smaller diameter employed for subarachnoid block decrease the risk of post dural puncture headache, these needles are challenging to use and carry a lesser success rate with reference to the spinal anesthesia.10
A number of studies show that paramedian approach was better than median approach in terms of post dural puncture headache (4% vs. 28%). The difference between both approaches was highly significant (p-value=0.05).9 However different results were present showing that with median approach 9.3% patients developed post dural puncture headache while with paramedian approach, 10.7% patients developed post dural puncture headache, showing that there was no statistically significant difference in post dural puncture headache among the two approaches (p=0.875)11 Completely opposite results showed that post dural puncture headache was rather more common in paramedian than median approach (9.8% vs. 9.4%) though the results were statistically insignificant (p value > 0.05).12
The rationale of this study was to compare the frequency of PDPH with median and paramedian approach in elective cesarean section using 25 gauge pencil point needle for spinal anesthesia. The literature reported above had different results which created ambiguity whether the use of paramedian approach was better than median approach and limited research was available on this subject with 25 gauge pencil point needle. The study was conducted with a hope to bring change in clinical practice of using better approach (median or paramedian) to reduce PDPH associated morbidity and intervention.
We aimed to compare the frequency of post dural puncture headache in patients undergoing elective cesarean section under spinal anesthesia with median versus paramedian approach, using 25 gauge pencil point needle.
METHODOLOGY
This randomized controlled trial was conducted at Department of Anesthesiology, Surgical Intensive Care & Pain Management Centre as well as Department of Gynaecology & Obstetrics Peoples University of Medical & Health Sciences, Nawabshah, Shaheed Benazirabad, for six months from 01-12-2013 to 30-05-2014. Following parameters were used for sample size calculation with WHO sample size calculator.
Level of significance (α) =1%; Power of the test (1-β) =80%; Anticipated PDPH with Median approach= 28%; Anticipated PDPH with Paramedian approach= 4%
The minimum sample size turned out to be 60 patients in each group; 120 patients in total by non-probability, purposive sampling technique.
Pregnant females of age 20–40 years undergoing elective cesarean section under spinal anesthesia with ASA status I & II. Females suffering from cluster headache, tension headache, temporal arteritis, chronic pain syndrome, a history of migraine or any chronic headache preoperatively or on the morning of surgery.
Bleeding diathesis, deranged clotting profile, pre-existing neurological disorder or cardiac problem (abnormal ECG) and hypertension (BP > 140/90 mmHg).
Patients with history of allergy to any medications used in this study or contraindication for spinal anesthesia or with abnormality of vertebral column.
Data collection procedure: One hundred and twenty patients who presented in the Department of Gynaecology & Obstetrics fulfilling the criteria were counselled and explained the details of the study. Written informed consent, detailed history and assessment of each patient was done. Patients were randomly allocated into two equal groups;
Group A (median approach) and
Group B (paramedian approach).
Each group comprised of 60 patients.
Before commencing the block, facilities for resuscitation and back up of general anesthesia was confirmed. Monitors (ECG, NIBP, and SpO2) were attached and IV access secured. The back was cleaned using antibacterial solution. After appropriately preloading with 15 ml/kg Lactated Ringer’s solution, all blocks were performed in the sitting posture. Observing aseptic measures, the skin was infiltrated with 1% lignocaine solution at the appropriate lumbar space. Hyperbaric bupivacaine (0.75%) 1.6ml was injected intrathecally, as a local anesthetic agent by using 25 gauge pencil point needle. Immediately after spinal anesthesia, the patient was positioned in the supine position and a >15° wedge was placed under the right hip to avoid supine hypotension. Hypotension was treated with rapid administration of intravenous fluids and injection phenylephrine 50-100 µg (0.5–1 mcg/kg). All the patients were given spinal anesthesia. Details were recorded regarding age, approach used and post dural puncture headache and visual analogue scale score over 72 post–operative hours. All the data was entered into the attached proforma.
Post dural puncture headache was described as patient’s complaint of feeling bilateral throbbing headache experienced within 6-72 hours of administration of spinal anaesthesia, which improves on lying down. Criteria included history of spinal anaesthesia, duration, frontal or occipital pain, aggravated by standing or movement and relieved on lying down.
The Visual Analogue Scale used as tool to assess the severity of pain. The following diagram was printed on an A4 sheet ensuring that the lines are exactly 10 cm in length. The print out was then folded at the dotted line. Patient was asked to mark the line according to his/ her pain by moving from no pain to worst pain without showing the numbered side. After that the VAS score was measured by unfolding the numbered side and recording the corresponding score.
PDPH was measured in terms of analogue scale
Pain score: Mild 1-3, moderate 3-6, severe 6-9, unbearable 10
Statistical analysis: All the collected data was entered into SPSS version 16. Quantitative variables i.e. age and VAS score were presented by mean ±SD. Qualitative variable i.e. post dural puncture headache was presented as frequency and percentage. Chi-square test was applied for comparison of post dural puncture headache in both groups. A p value of ≤0.05 was taken as statistically significant.
RESULTS
In our study, total 120 female patients, who met the inclusion criteria without falling into any of the exclusion criteria, were included. They were randomly allocated to one of the two groups (Group A & Group B of 60 patients each) by draw (lottery) method. None of the patients were dropped out or lost from the study at any stage.
Patients in both groups were similar regarding age distribution. In Group A, (median approach), there were 54 patients (90%) in age group 20-30 years & 06 patients (10%) in age group 31-36 years. In Group B, (paramedian approach), there were 49 patients (81.7%) in age group 20-30 years & 11 patients (18.3%) in age group 31-36 years. Statistically there was insignificant difference between the age of the patients among the two study groups i.e. p-value=0.302 (Figure 1)
The mean age of the total patients were noted as 26.92 ± 4.02 years with minimum age of 20 and maximum age of 36 years. In Group A, mean age of patients were noted as 26.82 ± 4.52 years with 20 & 36 years minimum and maximum ages respectively. In Group B, the mean age of the patients were noted as 26.77 ± 4.13 years with 20 & 36 years minimum and maximum ages respectively.
Out of total 120 patients, included in the study, 4 patients presented with PDPH. The overall frequency of PDPH in all patients under study was 3.33%. In Group A (Median group), 3 patients (out of 60) developed PDPH. Frequency of PDPH in Group A was 0.05 (5%). In this group 1st patient was of 20 years old, primipara,, developed PDPH within 24 hours that was of moderate degree, 2nd patient was 24 years old P2+0, developed PDPH of moderate degree after 24 hours and 3rd patient was 27 years old, P3+0 developed PDPH after 24 hours which was of mild degree.
In Group B (Paramedian group), only 1 patient (out of 60) developed PDPH. Frequency of PDPH in Group B was 0.0167 (1.67%). She was 25 years old, para 2+0, developed PDPH after 24 hours, which was moderate in degree.
In mild case, patient was treated by rest, plenty of fluids and simple analgesics containing caffeine. In moderate cases, patients were treated by bed rest, plenty of fluids, strong analgesics, and caffeine and muscle relaxants. Caffeine was given in the form of tablets, tea and coffee. In all patients, PDPH was relieved within 2-3 days without any complication.
PDPH was absent in 116 (96.67%) patients in which 57 (95%) patients belonged to Group A and 59 (98.33%) patients belonged to Group B. Statistically there was insignificant difference between the study groups i.e. p-value=0.30 (Table 1; Figure 2).The mean VAS of the total patients were noted as 2.54 ± 1.187 with minimum score of 1 and maximum score of 06 (Table 2).
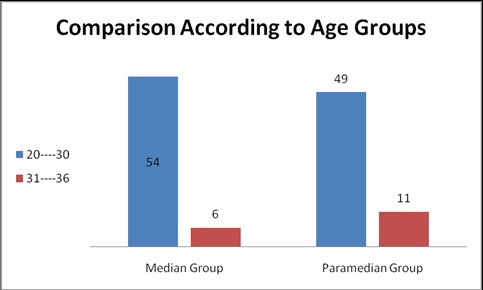
Figure 1: Comparison According to Ages (Group A Vs. Group B)
Table 1: Comparison of PDPH between study groups
| PDPH | Group | Total | |
| Group A | Group B | ||
| Present | 3(5%) | 1(1.67%) | 4(3.33%) |
| Absent | 57(95%) | 59(98.33%) | 116(96.67%) |
| Total | 60(100%) | 60(100%) | 120(100%) |
Chi-square= 1.034; p -value= 0.30 (insignificant)
p -value= 0.24(insignificant)/Fischer exact test
Group A= Median Group; Group B=Paramedian Group
Figure 2: PDPH in Group A vs. Group B
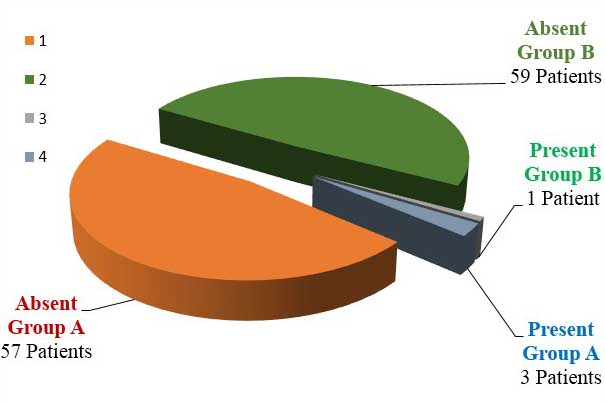
Table 2: Descriptive statistics of VAS of the patients
| VAS | Total | 120 |
| Mean | 2.54 | |
| SD | 1.187 | |
| Minimum | 01 | |
| Maximum | 06 |
VAS = Visual analogue score
DISCUSSION
The results of our study showed that frequency of PDPH was less with the use of paramedian approach as compared to median approach, using 25 gauge pencil point needle in patients undergoing elective cesarean section under spinal anesthesia; but unfortunately the difference in the frequency of PDPH between the two groups was statistically insignificant. Group A patients had received spinal anesthesia with median approach while Group B patients received spinal anesthesia with paramedian approach. In Group A, 3 (out of 60) patients developed PDPH and the frequency of PDPH was 0.05 (5%). In Group B, 1 (out of 60) patients presented with PDPH and the frequency of PDPH was 0.0167 (1.67%). Though apparently there was reduction in the incidence of PDPH with the use of paramedian approach, the difference in the frequency of PDPH between the two groups was statistically insignificant i.e. p-value=0.30.
Some studies do favor our results whereas some do not.
Haider et al. on 50 patients undergoing different elective surgeries under spinal anesthesia found a statistically significant difference in the incidence of PDPH with median and paramedian approaches. They concluded that the paramedian approach using the Quincke level needle reduces the incidence of PDPH significantly.9
Mosaffa et al. concluded that there is no difference in PDPH incidence with median versus paramedian approaches, and therefore recommend the paramedian approach, especially for older patients with degenerative changes in the spine and intervertebral spaces, and those who cannot assume the proper position for the median approach; the easier positioning would result in less pain for the patient and a higher success rate for spinal anesthesia.11
Sadeghi et al. conducted a randomized double blind clinical trial of 125 patients scheduled for elective cesarean section who received spinal anesthesia with median or paramedian approach. Headache was evaluated for three days following surgery. The incidence of headache was 9.8% in paramedian group versus 9.4% in median group (p>0.05). The authors concluded that the use of paramedian approach in pregnant women who have difficulty in positioning is acceptable and without increasing risk of headache and hemodynamic changes.12
Janick et al. on 250 patients undergoing transurethral prostate surgery under spinal thesia reported a significantly higher rate of PDPH with the paramedian approach than with the median approach in relatively older patients, while no significant difference was observed in younger patients.13
Li JY et al. compared the technical difficulty and the incidence of post dural puncture headache (PDPH) between two approaches of spinal anesthesia i.e. median and paramedian approaches. Cesarean section was performed in 700 women under spinal thesia with either median or paramedian approach. It revealed that median approach was associated with a significantly greater success rate in the first attempt (231 of 350 patients) than paramedian approach. (205 of 350 patients) (p<0.05). The incidences of PDPH between median and paramedian approaches after single dural puncture is 4.33% (10 of 231 patients) and 0.97% (2 of 205 patients), respectively. They concluded that paramedian approach might significantly reduce the incidence of PDPH but it would need a more skillful hand to increase the successful rate.14
Muranaka et al.“ compared midline approach with paramedian approach for combined spinal-epidural thesia(CSEA) by needle through needle technique.70 patients undergoing elective gynecological surgery received CSEA with a 27 G Whitacre spinal needle, which protrudes 12 mm beyond the tip of the Tuohy needle. They concluded that the choice of midline or paramedian approach for CSEA did not affect the success rate of the subarachnoid puncture, but paramedian approach required longer protrusion length of the spinal needle than midline approach. To raise the success rate of subarachnoid puncture by paramedian approach, they recommended a long protruded spinal needle to raise the success rate by paramedian approach.15
Kumar and Mehta reported three cases in which patients with Ankylosing Spondylitis were successfully administered spinal thesia using a paramedian approach after failed attempts with a median approach.119 Nevertheless, Schelew et al., suggest that both; midline and paramedian methods may be attempted with success.16
Sivrikaya et al. study described that spinal anesthesia was successfully administered by the median approach in the lateral position on the first attempt, but preceded by two failed attempts by the median approach in the sitting position.17
Morgan et al. described that the median approach involves passage of needle through the supraspinal and interspinal ligaments and the ligamentum flavum, but the paramedian approach avoids the supra and interspinal ligaments and approaches the ligamentum flavum directly after passing through the para spinal muscles.18
Zhurda, Ahmed, & Ahsan-ul-Haq, in their studies concluded that paramedian approach would be an easier method of spinal anesthesia especially for older patients, who had sclerosed ligaments and degenerative changes in the spine and intervertebral spaces.19,20
Since female gender & pregnancy are already well known risk factors for PDPH, we specifically conducted our study only on obstetric (pregnant) female patients undergoing cesarean section under spinal anesthesia to exclude any confounding element between the two study groups.
In our study, we used 25-guage pencil-point (Whitacre) needles, not Quincke needles, because pencil-point needles are known to cause less PDPH than Quincke needles. Moreover, this is the type of needle are now routinely available for performing spinal anesthesia in our institute. Hence, our thetist have become used to handle these needles, without causing many complications. Another reason for conducting this study with 25-guage pencil-point needle is that only limited research was available on this topic particularly with 25 gauge pencil point needle. That is why, we used 25-guage pencil point needle to perform spinal anesthesia in all patients of both study groups.
The main limitation of our study is a smaller sample size due to which we couldn’t get statistically significant results. In fact, the results of our study have merely increased the need for conducting more studies with larger sample size to establish whether median or paramedian approach is better in reducing PDPH.
CONCLUSION
It is concluded through results of this study that paramedian approach is apparently better than median approach in terms of reducing frequency of PDPH in patients undergoing elective cesarean section under spinal anesthesia, though the results were clinically insignificant.
It is, therefore, recommended that more clinical trials with larger sample size are conducted so as to get statistically significant results to establish whether median or paramedian approach is better in reducing PDPH in patients undergoing cesarean section under spinal anesthesia.
Conflict of interest: Nil
REFERENCES
- Morgan Jr GE, Mikhail MS, Murray MJ. Clinical Anesthesiology. New York: McGraw-Hill Medical; 2013.
- Luck JF, Fettes PD, Wildsmith JA. Spinal anaesthesia for elective surgery: a comparison of hyperbaric solutions of racemic bupivacaine, levobupivacaine, and ropivacaine. Br J Anaesth 2008; 101:705-710. doi: 10.1093/bja/aen250. [PubMed] [Free full text]
- Brull R, MacFarlane AJR, Chan VWS. Spinal, epidural, and caudal anesthesia. In: Miller RD, ed. Miller’s Anesthesia. 8th ed. Philadelphia, (PA): Elsevier Saunders; 2015:chap 56.
- Kettner SC, Marhofer P Willschke H. Does regional anaesthesia really improve outcome? Br J Anaesth. 2011 Dec;107 Suppl 1:i90-5. doi: 10.1093/bja/aer340.doi: 10.1093/bja/aer340. [PubMed] [Free full text]
- Ali ZH. Effect of pre and post nursing intervention on the occurrence of tension headache among surgical patients undergoing spinal anesthesia. J Anesth Clin Res 2012;3:7-11.[Free full text]
- Hamzei A, Basiri-Moghadam M, Pasban-Noghabi S. Effect of dexamethasone on incidence of headache after spinal anesthesia in cesarean section. A single blind randomized controlled trial. Saudi Med J. 2012 Sep;33(9):948-53. [PubMed]
- Bezov D, Ashina S, Lipton R. Post-dural puncture headache: Part II–prevention, management, and prognosis. Headache. 2010 Oct;50(9):1482-98. doi: 10.1111/j.1526-4610.2010.01758.x. [PubMed]
- Ankorn C, Casey WF. Spinal Anaesthesia – a practical guide. Update in Anaesthesia. 2000; 12: 21-34 [Free full text]
- Haider S, Butt KJ, Aziz M, Qasim M. Post Dural Puncture Headache-A Comparison Of Midline And Paramedian Approaches. Biomedica. 2005;21:90–2.
- Ghaleb A. Postdural puncture headache. Anesthesiol Res Pract. 2010;2010. pii: 102967. doi: 10.1155/2010/102967. [PubMed] [Free full text]
- Mosaffa F, Karimi K, Madadi F, Hasan KS, Besheli LD, Eajazi A. post dural puncture headache: a comparison between median and paramedian approaches in orthopedic patients. Anesth Pain Med. 2011 Fall;1(2):66-9. doi: 10.5812/kowsar.22287523.2159.[PubMed] [Free full text]
- Sadeghi A, Razavi SS, Gachkar L, Ariana P, Ghahremani M. Comparison of the incidence of post spinal headache following median and para median approach in cesarean patients. J Iranian Soc. Anesthesiol Intens Care 2009;31:4-9.
- Janik R, Dick W. Post spinal headache. Its incidence following the median and paramedian techniques. Anesthetist 1992;41:137-41. [PubMed]
- Li JY, Tsai SC, Wang CH, Hui YL, Tan PC. Paramedian Approach Reduce the Incidence of post dural puncture headache. Chinese J. Pain 1995;5:71-76.
- Muranaka K, Mizutani H, Seo K, Yoshida M, Gohara T, Miyawaki H. A comparison between midline and para median approaches for combined spinal-epidural anaesthesia. Masui 2001;50:1085-8. [PubMed]
- Kumar CM, Mehta M. Ankylosing spondylitis: lateral approach to spinal anaesthesia for lower limb surgery. Can J. Anesth 1995;42:73-6. [PubMed]
- Sivrikaya GU, Hanci A, Dobrucali H, Yalcinkaya A. Cesarean section under spinal anaesthesia in a patient with ankylosing spondylitis. Middle East J Anesthesiol 2010;20:865-8. [PubMed]
- Morgan G, Mikhail M, Murray M, Larson Jr M. Anesthesia for orthopedic surgery. In: Morgan GE, Mikhail MS Clinical Anesthesiology 2nd ed. Stamford, Conn: Appleton & Lange 1996; p. 675-7.
- Zhurda T. Kërçi M, Bajraktari M, Muzha D, Kurti B. The advantages of para median approach for spinal anesthesia of elderly patients in urology surgery .Eur J Anaesthesiol 2010;47:130. [Free full text]
- Ahsan-ul-Haq M, Amin S, Javaid S. Paramedian technique of spinal anesthesia in elderly patients for hip fracture surgery. J Coll Physicians Surg Pak. 2005;15(3):160–1 [PubMed]

