Anil Agarwal1, Chetna Shamshery2, Susheel PrakashAmbesh1, Anuj Jain3
1Professor; 2Senior Resident; 3Senior Resident
Department of Anesthesiology, Sanjay Gandhi Post Graduate Institute of Medical Sciences (SGPGI), Rae Bareli Road, Lucknow, Uttar Pradesh 226014 (India)
Correspondence:Dr Chetna Shamshery, M-139, Aashiana Colony, Kanpur Road, Lucknow, Uttar Pradesh(India); Cell: +918004904611; E-mail: drchetna@rediffmail.com
ABSTRACT
Introduction:Low back pain (LBP) has a point prevalence of 11.9 ± 2% worldwide. Nucleoplasty is a minimally invasive procedure, combining disc removal and thermal coagulation using radiofrequency waves in the nucleus pulposus. The purpose of this preliminary study was toevaluate the efficacy of nucleoplasty in patients with low back pain and radiculopathy, and to have comparative evaluation of the disc appearance on MRI pre- and post-procedure.
Methodology: We enrolled 20 patients, suffering with low back pain along with radiculopathy undergoing nucleoplasty from June 2010 to June 2012. Inclusion criteria were; patients of either sex, age 18-60 yrs, one or two level herniated disc (contained), failed conservative therapy for six weeks. Exclusion criteria were loss of >50% disc height and severe disc degeneration. Post nucleoplasty patients were called for follow up at 3, 6 and 12 months. Repeat MRI was done after 3 months of nucleoplasty to look for changes in the intervertebral disc. Pain was assessed using the visual analogue scale (VAS) and patient’s satisfaction was evaluated by Macnab’s outcome assessment. Statistical analysis was done with Friedman ANOVA using the package SPSS 21.0 (SPSS Inc.,Chicago, IL). A p-value of < 0.05 was considered significant.
Result: There were 4 drop outs and thus we present results of 16 patients only. In 13 patients single disc decompression was done, whereas in the remaining 3 patients it was done at two levels. Post procedure MRI was evaluated in 8 patients. Following nucleoplasty 81% of patients experienced pain relief and improvement in patient satisfaction. MRI performed 3 months after the procedure revealed appreciable reduction in the disc bulge in 3 out of 8 (37.5%) patients.
Conclusion: Nucleoplasty appears to be a safe and favorable day care minimally invasive procedure in selected patients. Large randomized, controlled studies are required to correlate MRI findings to clinical outcomes.
Key words: Pain;Low back pain;Low Back Pain, Recurrent;Failed Back Surgery Syndrome; Neurologic Manifestations; Radiculopathy;Neuralgia; Lumbar vertebra;Decompression;Treatment outcome
Citation: Agarwal A, Shamshery C, Ambesh SP, Jain A. Evaluation of nucleoplasty in patients of low back pain with radiculopathy: A preliminary report.Anaesth Pain & intensive Care 2015;19(3):292-296
This study was presented as a poster in the ISSPCON conference at Nagpur (India), in February 2013.
INTRODUCTION
Low back pain (LBP) has a point prevalence of 11.9 ± 2% worldwide,1 and if it remains persistent for more than 3 months, it is called chronic LBP. A systematic approach to the management of LBP has been advised by the American Pain Society.2The interventional therapiesfor LBP includemany minimally invasive procedures (MIP), e.g.disc decompression, nucleotomy and nucleoplasty etc. The purpose of all interventions is to relieve the pressure on the nerve roots, either by managing the bone or the disc pressing the nerve root. The MIP of the disc remove a part of the nucleus pulposus, hence reducing the intradiscal pressures and allowing the intact annulus to regain its normal position.3 Nucleoplasty is a MIP introduced in the year 2000. Procedure combines disc removal and thermal coagulation with radiofrequency in the nucleus pulposus, which causes a molecular dissociation process converting tissue into gas. In the present study we evaluated the efficacy of nucleoplasty in patients suffering from low back pain with radiculopathy and its association with changes in the MRI following the procedure.4,5
METHODOLOGY
In the present study we enrolled 20 patients undergoing nucleoplasty, who reported with low back pain with radiculopathy, due to disc disease leading to nerve root compression (16) or patients with spinal stenosis but unwilling for spinal surgery(4 patients), from June 2010 to June 2012.We obtained formal approval from the institute’s ethical committee and the informed consent of every patient.The patients of either sex, age 18-60 yrs, who failed conservative therapy for six weeks,were enrolled. The conservative therapy offered to the patients was tab pregabalin 150mg at night +tab amitripty line10mg at night + tab tramadol thrice a day.Exclusion criterion were loss of disc height by>50%and/or severe disc degeneration.
Following written informed consent patients were wheeled into the operating room, infusion of normal saline was started and inj. cefazoline 2 g was administered. Standard monitors for blood pressure, heart rate and oxygen saturation were connected. Patients were placed in prone position on the operating table, with a pillow under the abdomen to decrease the lumbar lordosis and the back was painted with10% povidone-iodine(Betadine®) solution and draped. Targeted disc was visualise dantero-posteriorly by fluoroscopy, the end plates were overlapped using cephalo-caudal tilt of the fluoroscope and oblique angulation was done so as to bring the superior articular process of the inferior vertebral body in the middle of the intervertebral disc.
The puncture site was taken in front of the superior articular process in the middle of the disc.Skin was infiltrated using local anesthetic and the Perc-DC SpineWand™(Arthrocare, Sunnyvale, CA, USA)was introduced in the disc in the nucleus pulposus in gun barrel view. Six channels were created by rotating the SpineWand™ by 60º after entering the disc, taking 10 sec each during forward and backward movements at 2,4, 6, 8, 10 and 12’o clock positions setting the coablation machine at 2mA. The patients were observed for six hours post-procedure in the postoperative room and then were discharged. They were advised to take tab ciprofloxacin 500mg twice a day for 5 days, tab etoricoxib 90mg at night for 3 days, tab tramadol 37.5 mg/paracetamol 325 mg as required, tab pregabalin 150mg and tab amitripty line 10mg at bed time. They were recommended rest for 1 week, minimal daily routine activities at home, and to avoid forward bending or lifting heavy weight. They were asked to revisit the pain clinic after 2weeks for review, and inform us as and if there was any aggravation of the pain.
All the procedures were done under local anesthesia.If at any moment patient reported of nerve root irritation, the position of the SpineWand™ was changed. Following the procedure follow-up was advised at 3, 6 and 12 months. A repeat MRI was done after 3 months of nucleoplasty in all patients who had done it prior to procedure as well, to look for changes in the intervertebral disc. On each follow up visit pain was assessed using the visual analogue scale (VAS) of 0-10. At 1 year follow up visit patient’s satisfaction was assessed based on Modified MacNab’s Criteria 5 for outcome assessment (Box 1).
Box 1: Modified MacNab’s Criteria
Statistical analysis was done with Friedman ANOVA using the package SPSS 21.0 (SPSS Inc.,Chicago, IL). A p-value of < 0.05 was considered significant.
RESULTS
A total of 20 adult patients were enrolled during the study period. There were 4 dropouts as 3 did not turn up for follow up and in one patient the procedure was abandoned due to nerve irritation. The remaining 16 patients had mean height of 165 ± 15 cm, weight 45-75 kg and a M:F ratio 5:3.
In 13 patients nucleoplasty was done at one level and in 3 patients it was done at two levels based upon MRI findings and clinical history.
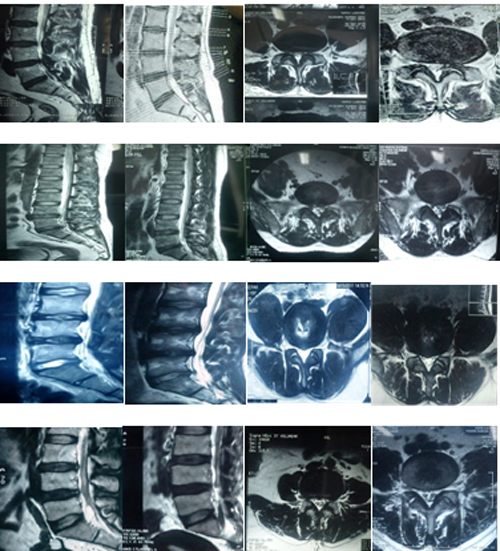
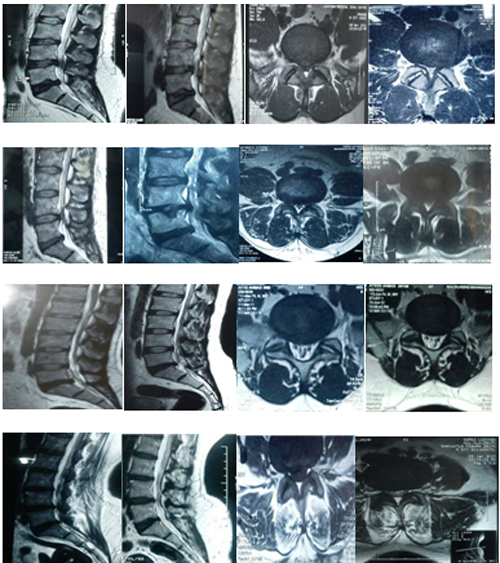
Figure 1: MRI pictures of 8 patients demonstrating pre and post procedure disc
PRE POST PRE POST
Significant reduction in pain was observed immediately following nucleoplasty and it persisted till the end of the study period i.e. up to one year post-procedure.Pre-procedure median VAS was 8, reduced to 6 immediately after the procedure, and it was 2.5 after one year (p<0.05). It shows that the reduction was statistically significant at 12 month interval.
Pre- and post-procedure MRI evaluation was done in 8 patients. In 3 out of these 8 patients morphologically appreciable reduction in disc size was observed after 3 months (Figure1).
No complications were noted in any patient.
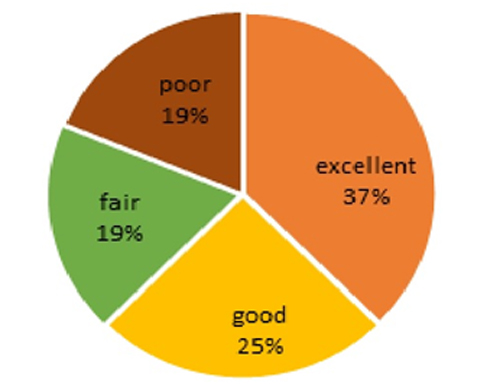
Figure 2: Patient satisfaction as assessed by MacNab’s grade at 1 year following neucleoplasty
Patient satisfaction following nucleoplasty at 1 year was reported as excellent (37%), good (25%), fair (19%) and poor (19%) respectively (Figure2).
DISCUSSION
Following nucleoplasty 81% of patients experienced pain relief along with improvement in patient satisfaction (excellent to fair) till the end of the study period i.e. 1 year. MRI performed 3 months after the procedure revealed appreciable reduction in the disc bulge in 37.5% of patients. 4 (25%)patients out of sixteen did not have any pain relief, nor did they have any improvement in patient satisfaction. 3 out of these had spinal canal stenosis.
Nucleoplasty is a percutaneous disc decompression using radiofrequency energy. Bipolar radiofrequency coagulation denatures proteoglycan and changes the tissue inside nucleus pulposus to liquid or gaseous state, which is absorbed and removed at the target site.6Chen et al proved in a cadaveric specimen that the decompression using Coblation® technique decreased the pressure in the disc.3 The advantage of the Coblation® technique used in nucleoplasty is that it does precise and targeted removal of nucleus pulposus with minimal thermal injury to the surrounding tissues.7
There exists a level II-3 evidence for mechanical lumbar percutaneous disc decompression with nucleoplasty in treatment of leg pain.8Our patients also had significant pain relief in the radicular component following the procedure. 12 out of 16 patients experienced subjective relief of >50%.Patient selection criterion for the procedure constitutes an important factor to ensure optimum benefit of nucleoplasty. Our study included 4 patients of spinal stenosis. Out of these 4 patients one had excellent relief, one had fair relief and 2 had poor relief.
Out of the 8 patients in which post procedure MRI done at 3 months after the procedure, morphologic reduction in disc size was appreciable in 3 patients, contrary to the prior studies which did not show obvious changes at early post-operative MRI.9Out of these three patients two patients had excellent outcome on modified Macnab outcome assessment whereas, but the third one had only fair relief in the symptoms. Animal model in 2012 showed a reduction of 16% of nucleus pulposus following nucleoplasty.10 Human studies have yet to be done to show the reduction in the volume of nucleus pulposus. Some earlier studies regarding relief in the clinical symptoms have been done before and reported good efficacy and regression of an intevertebral disc following cervical nucleoplasty.11,12 We observed that following nucleoplasty majority of patients experience pain relief along with improvement in patient satisfaction till 1 year after the procedure.
LIMITATIONS
Major limitation of the present study isa very small number of cases included, along with the absence of the control group. MRI studies were not complete in all of the patients.
CONCLUSION
Based upon our observations, we conclude that nucleoplasty, appears to be safe and effective modality in treating discogenic disease with radicular symptoms. However,larger randomized control trials are needed to prove its efficacy and safety.Changes in the disc morphology following nucleoplasty based on MRI or other diagnostic modalities need also to be studied at a larger scale.
Conflict of interest: None declared by the authors
REFERENCES
- Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F,A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012 Jun;64(6):2028-37. [PubMed] doi: 10.1002/art.34347.
- Liz Horsley. ACP Guidelines for the Diagnosis and Treatment of Low Back Pain. Am Fam Physician 2008;77(11):1607-10. [PubMed][Free full text]
- Chen YC, Lee SH, Chen D. Intradiscal pressure study of percutaneous disc decompression with nucleoplasty in human cadavers. Spine2003;28:661–5. [PubMed]
- Raj P. Interventional pain management image guided procedures. 2nd Edition. Philadelphia, Saunders Elsevier, 2008, pp 548-49
- Raj P. Interventional pain management image guided procedures. 2ndEdition. Philadelphia, Saunders Elsevier, 2008, pp 344-45
- Bonaldi G, Baruzzi F, Facchinetti A, Fachinetti P, Lunghi S. Plasma radio-frequency-based diskectomy for treatment of cervical herniated nucleus pulposus: feasibility, safety, and preliminary clinical results. Am J Neuroradiol 2006;27(10):2104–11. [PubMed][Free full text]
- Boswell MV, Trescot AM, Datta S, Schultz DM, Hansen HC, Abdi S, etal. Interventional techniques: evidence-based practice guidelines in the management of chronic spinal pain. Pain Physician2007;10:7–111. [PubMed][Free full text]
- Manchikanti L, Derby R, Benyamin RM, Helm S, Hirsch JA. A systematic review of mechanical lumbar disc decompression with nucleoplasty. Pain Physician 2009;12(3):561-72. [PubMed][Free full text]
- Calisaneller T, Ozdemir O, Karadeli E, Altinors N. Six months post-operative clinical and 24 hour post-operative MRI examinations after nucleoplasty with radiofrequency energy. Acta Neurochir (Wien) 2007;149(5):495–500. [PubMed]
- Kasch R, Mensel B, Schmidt F, Ruetten S, Barz T, Froehlich S, etal.Disc volume reduction with percutaneous nucleoplasty in an animal model.PLoS One.2012;7(11):e50211. [PubMed][Free full text] doi: 10.1371/journal.pone.0050211.
- Masala S, Massari F, Fabiano S, Ursone A, Fiori R, Pastore F,et al. Nucleoplasty in the treatment of lumbar diskogenic back pain: one year follow-up. Cardiovasc Intervent Radiol 2007;30(3):426–32. [PubMed]
- Sim SE, Eun, Ko S, Kim DK, Kim HK, Kim YC, et al. The results of cervical nucleoplasty in patients with cervical disorder: A retrospective clinical study of 22 patients. KJP 2011 Mar;24(1):36-43. [PubMed][Free full text] doi: 10.3344/kjp.2011.24.1.36.