Sedef Gulcin Ural¹, Dilek Yazicioglu2, Hasan Sahin3, Ugur Altinisik3, Tugba Dogu3, Hatice Betul Altinisik3, Mustafa Ozmen4, Basak Sahin5.
1Department of Anesthesiology and Reanimation, Osmaniye State Hospital, Osmaniye (Turkey)
2Department of Anesthesiology and Reanimation, Dışkapı Yıldırım Beyazıt Training and Research Hospital, Ankara (Turkey)
3Department of Anesthesiology and Reanimation, Faculty of Medicine, Canakkale Onsekiz Mart University, Canakkale (Turkey)
4Department of Anesthesiology and Reanimation, Van Training and Research Hospital, Van (Turkey)
5Department of Psychiatry, Faculty of Medicine, Canakkale Onsekiz Mart University, Canakkale (Turkey)
Correspondence: Hasan SAHIN, MD, Department of Anesthesiology and Reanimation, Faculty of Medicine, Canakkale Onsekiz Mart University, Kepez, Canakkale, (Turkey); Phone:+90 5057647997; Fax: +90 286 263 59 56; E-mail: drhasan@comu.edu.tr
ABSTRACT:
Objective: Patients undergoing surgery, experience acute physiological distress in the preoperative period. Smoking addiction is a complex behavior in which environment and genetic effects play a part. In this study our aim was to compare the impact of cigarette smoking cessation verses continued smoking on preoperative HAM-A scores and anesthetic requirement
Methodology: After approval by the Ethic Committee, informed consent was obtained from patients, 18- 65 years old, American Society of Anesthesiologists (ASA) physical status I-II, 120 patients scheduled for elective laparoscopic cholecystectomy were included in this prospective randomized, double-blind study. Groups were defined as Group N (n:60, patients who continued smoking in the preoperative period) and Group NS (n:60, who stopped smoking 48 hours before the operation).Only the first patient on the list were included… All patients received intravenous midazolam 0.05-0.1 mg/kg as premedication. In the preoperative period HAM-A scores were recorded while the preoperative examination was performed in the outpatient clinic and after premedication. In addition, we monitored patients with Bispectral Index Monitor (BIS) and anesthetic requirements were recorded during surgical procedure.
Results: HAM-A scores in the outpatient clinic and after receiving premedication were statistically significantly higher in Group N. Additional fentanyl requirement was also significantly higher in Group N.
Conclusion: We conclude that to stop smoking 48 hours before surgery reduced anxiety as measured by HAM-A scores and anesthetic requirement and increased patient comfort.
Key words: Cigarette; Smoking; Preoperative anxiety; Anesthetic requirement; Anesthesia; Fentanyl
Citation: Ural SG, Yazicioglu D, Sahin H, Altinisik U, Dogu T, Altinisik HB, Ozmen M, Sahin B. Effects of preoperative smoking cessation on HAM-A sedation scores and intraoperative consumption of anesthetic and fentanyl. Anaesth, Pain & Intensive Care 2017;21(1):52-58
Received: 5 Dec 2016; Reviewed:1 Dec 2016; 14 Jan 2017; Corrected:16 Dec 2016, 17 Jan 2017; Accepted:8 Mar 2017
INTRODUCTION:
Patients undergoing surgery, experience acute physiological distress in the preoperative period1. There can be many reasons for anxiety in the preoperative period. Besides being away from home and family/relatives, concerns about interruption of daily activities, complications that can occur during and after surgery, insufficient information about anesthesia and surgery, concerns about not waking up at the end of surgery and feeling pain during and after surgery.2 It is reported that the incidence of anxiety among adult patients is between 11% and 80%.3 Anxiety can manifest as aggressive reaction4 and controlling and managing postoperative pain becomes more difficult in these patients.4,5 In addition to these, requirement for high anesthetic doses in the intraoperative period3 and the frequency of postoperative patient controlled analgesia (PCA) demands may increase.
Smoking addiction is a complex behavior in which environment and genetic effects play a part.7 Psychological elements and habits also play a role. The main component in addiction is nicotine in cigarette. Through specific nicotinic acetylcholine receptors, nicotine stimulates dopamine release which is thought to be responsible for acute rewarding effects of nicotine8. It has been showed that smoking has chronic anxiety effect.
The aim of our study was comparison of preoperative HAM-A anxiety scores and anesthetic requirement of chronic smoker patients who stopped smoking 48 hours before the operation with patients who continued smoking.
METHODOLOGY:
After obtaining the ethical committee approval and consent from patients, the study recruited 120, 18- 65 years old, ASA I- II patients undergoing laparoscopic cholecystectomy under general anesthesia. Exclusion criteria were as follows:anxiety disorders, physical/ psychological trauma in the recent year, use of sedative/ antidepressant/ antiepileptic drugs in the recent year, cooperation problems, difficulty in understanding, hearing impairment, history of malignancy, need to stay at the hospital more than one day in the preoperative period and having preoperative pain. After evaluating the patients before the operation, information about the surgery was provided to the patients. Patients were randomized into two groups. Group N (n = 60) patients who continued smoking in the preoperative period and Group NS (n = 60) who stopped smoking 48 hours before the operation. Only the first cases of operation list.
At the time of preoperative examination, demographic data (gender, age, body mass index, education level) of the patients, history of any previous operation, systemic disease, duration of smoking and number of cigarette consumption (year and number of cigarettes per day), and stress scores were recorded. The stress scores were assessed by the Hamilton Anxiety Rating Scale (HAM-A).
Twenty minutes after intravenous midazolam premedication (0.05-0.1 mg/kg), patients were evaluated with HAM-A scale. After standard monitoring, basal heart rate, systolic arterial pressure (SAP), diastolic arterial pressure (DAP) and mean arterial pressure (MAP) were recorded. All patients received propofol 2-3 mg/kg, fentanyl 1 µg/kg, vecuronium 0.1 mg/kg for anesthesia induction. After intubation, anesthesia was maintained with oxygen-nitrous oxide and sevoflurane. Depth of anesthesia was monitored by bispectral Index and titrated to maintain BIS between 40 and 60. Even when BIS value was between 40 and 60, if there was more than 20% increase in mean arterial pressure and/or heart rate compared with basal values fentanyl 50 µg was given to the patients.
Primary outcome measure of the study was the outpatient clinic-operation day anxiety level of the patients assessed with HAM-A scale. Secondary outcome measure was fentanyl consumption (in addition to the dose administered at induction).
Statistical analysis: SPSS for Windows 17.0 package program was used for data analysis. Kolmogorov Smirnov test was used to check whether continuous numerical distribution was close to normal. Descriptive statistics, was shown as mean ± standard deviation or median (minimum – maximum) for continuous variables, and number of cases and (%) for categorical variables.
The mean difference between two groups was analyzed with Student’s t test, and of the difference in terms of median values was analyzed with Mann Whitney U test. Categorical variables were assessed with Pearson’s chi-square test (χ2). The statistical difference between outpatient clinic scores and operation day HAM-A scores between the groups was compared using the Wilcoxon signed-rank test. Spearman’ correlation test was used to examine whether there was a significant relationship between age, education level, body mass index, cigarette pack year, total fentanyl consumption and operation day HAM-A and change in Hamilton anxiety scale scores.
Multivariate linear regression analysis was used to search whether there was a statistically significant difference between groups in terms of operating day HAM-A scores the outpatient clinic scores, after adjusting for other confounding factors. All variables determined as p > 0.15 after univariate statistical analysis were included in multivariate linear regression models as candidate factors. Regression coefficient for each variable, 95% confidence interval and t statistics were calculated. Because the data related to HAM-A scores were not normally distributed, logarithmic transformation was done in regression analysis. p < 0.05 was accepted as statistically significant.
RESULTS:
There was no statistically significant difference between Group N (those who continued smoking) and Group NS (those who stopped smoking 48 hours before the operation) in terms of mean age (41.6 ± 13.1, 42.1 ± 11) and gender distribution (p = 0.84, p = 0.855). There was no statistically significant difference between groups in terms of history of previous surgery and education levels (p = 0.271, p = 0.912). Between groups and Group NS statistically significant difference was not observed in terms of mean BMI (body mass index) (23.3 ± 2.6, 23.6 ± 2.9) and distribution of BMI levels (p = 0.618, p = 0.350). Median smoking pack year levels were statistically similar between groups (Group N and Group NS (p = 0.205). The median fentanyl consumption was significantly higher in Group NS than Group N (p < 0.001).
Table 1: Demographic and clinical characteristics of the cases according to the groups
| Group N
(n = 60) |
Group NS
(n = 60) |
p-value | |
| Age (year) | 41.6 ± 13.1 | 42.1 ± 11.0 | 0.845† |
| Sex | 0.855‡ | ||
| Male | 29 (48.3%) | 30 (50.0%) | |
| Female | 31 (51.7%) | 30 (50.0%) | |
| History of the previous operation | 36 (60.0%) | 30 (50.0%) | 0.271‡ |
| Primary School | 0.912‡ | ||
| Primary School | 13 (21.7%) | 13 (21.7%) | |
| Secondary School | 4 (6.7%) | 6 (10.0%) | |
| High School | 27 (45.0%) | 27 (45.0%) | |
| University | 16 (26.7%) | 14 (23.3%) | |
| Body Mass Index (kg/m2) | 23.3 ± 2.6 | 23.6 ± 2.9 | 0.618† |
| Body Mass Index | 0.350‡ | ||
| < 25 kg/m2 | 39 (65.0%) | 34 (56.7%) | |
| ≥25 kg/m2 | 21 (35.0%) | 26 (43.3%) | |
| Cigarette (pack year) | 6.0 (0.5-37) | 7.6 (0.5-43.7) | 0.205 |
| Total fentanyl consumption | 100 (50-150) | 50 (0-100) | < 0.001 |
†Student’s t test, ‡ Pearson’s Chi- Square test, ¶ Mann Whitney U test
Both outpatient clinic and operation day median HAM-A scores were statistically higher in Group N(continued smoking) than Group NS (stopped smoking 48 hours before the operation) (p < 0.001, p < 0.001).
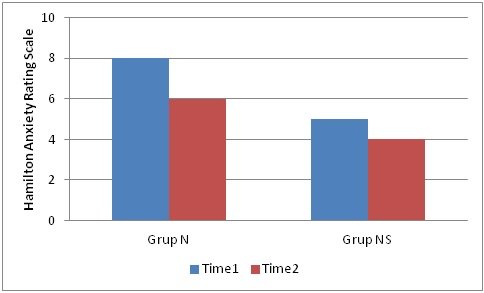
In Group N (continued smoking), when compared with outpatient clinic values, there was statistically significant decrease in median HAM-A score (p < 0.001). Also in Group NS, when compared with outpatient clinic values, there was statistically significant decrease in median HAM-A score (p < 0.001). The HAM-A score decreased more in Group N than Group NS and this difference was statistically significant (p < 0.001) (Figure 1).
Figure 1: The HAM-A score decreased more in Group N than Group NS, and was statistically significant (p < 0.001)
There was no statistically significant correlation between age, body mass index, cigarette pack year and change in operation day HAM-A score (p > 0.05). With an increase in total fentanyl consumption, operation day HAM-A score decreased (p = -0.339, p < 0.001).
Table 2: Outpatient clinic and operation day Hamilton anxiety scores according to the groups
| Outpatient clinic | Operation day | p-value† | Change | |
| Group N | 8 (4-10) | 6 (3-7) | < 0.001 | -2 (-4 – 0) |
| Group NS | 5 (4-8) | 4 (3-6) | < 0.001 | -1 (-2 – 0) |
| p-value ‡ | < 0.001 | < 0.001 | < 0.001 |
† Comparisons in groups, between Outpatient clinic and operation day, Wilcoxon Sign test, ‡ comparisons between groups in terms of anxiety levels in Outpatient clinic and operation day and changes in operation day anxiety score with regard to Outpatient clinic levels, Mann Whitney U test
With the increase in education levels, operation day HAM-A score decreased and this was statistically significant (p = -0.219, p = 0,016). With the increase in total fentanyl consumption, operation day HAM-A score increased (p = 0.518, p < 0.001).
Table 3: Correlation coefficients and momentousness levels between age, education levels, body mass index, cigarette pack year, total fentanyl consumption and change in operation day HAM-A and Hamilton anxiety score
| Parameter | Postop HAM-A | Δ HAM-A | |
| Age | Correlation coefficient | -0.129 | 0.109 |
| p-value † | 0.161 | 0.235 | |
| Education level | Correlation coefficient | -0.219 | 0.117 |
| p-value † | 0.016 | 0.205 | |
| Body mass index | Correlation coefficient | 0.007 | 0.087 |
| p-value † | 0.940 | 0.342 | |
| Cigarette pack year | Correlation coefficient | -0.030 | 0.164 |
| p-value † | 0.742 | 0.074 | |
| Total fentanyl consumption | Correlation coefficient | 0.518 | -0.339 |
| p-value † | < 0.001 | < 0.001 |
† Spearman’s correlation test
There was no statistically significant difference between males and females in terms of both operation day median HAM-A score and degree of change in HAM-A score (p = 0.137, p = 0.254).
Table 4: Operation day HAM-A score and amount of change in Hamilton anxiety score according to sex, history of operation and body mass index
| Parameter | Operation day HAM-A | p-value†¶ | Δ HAM-A | p-value ‡¶ |
| Sex | 0.137 | 0.254 | ||
| Male | 4 (4-7) | -2 (-4 – 0) | ||
| Female | 5 (3-7) | -2 (-4 – 0) | ||
| History of previous operation | 0.059 | 0.406 | ||
| No | 4 (3-6) | -2 (-4 – 0) | ||
| Yes | 5 (4-7) | -2 (-4 – 0) | ||
| Body mass index | 0.956 | 0.155 | ||
| < 25 kg/m2 | 5 (3-7) | -2 (-4 – 0) | ||
| ≥25 kg/m2 | 5 (3-7) | -2 (-2 – 0) |
† Comparisons between groups in terms of operation day HAM-A levels, ‡ comparisons between groups in terms of amount of changes in operation day HAM-A level with regard to outpatient clinic level, ¶Mann Whitney U test
A group of patients who had a history of previous operation and the group which did not have, there was no statistically significant difference in terms of both median HAM-A score and amount of change in HAM-A score (p = 0.059, p = 0.406).
Table 5: After adjusting for other risk factors, determining the determinative factor(s) in estimating the change in operation day HAM-A level
| Regression
Coefficient |
95% Confidence Interval | t-value | p-value | ||
| Lower limit | Upper limit | ||||
| Group N | 0.005 | -0.057 | 0.066 | -0.146 | 0.884 |
| Female factor | -0.006 | -0.059 | 0.046 | -0.234 | 0.815 |
| History of previous operation | 0.012 | -0.037 | 0.061 | 0.483 | 0.630 |
| Education level | -0.010 | -0.035 | 0.016 | -0.753 | 0.453 |
| Total fentanyl consumption | 0.001 | -0.0001 | 0.002 | 1.872 | 0.064 |
| Operation day HAM-A | 0.091 | 0.066 | 0.115 | 7.369 | < 0.001 |
According to body mass index levels, statistically significant difference was not observed in both median operation day HAM-A score and amount of change in HAM-A score (p = 0.956, p = 0.155).
Table 6: After adjusting for other possible risk factors, determining the determinative factor(s) in predicting the amount of change in operation day HAM-A level compared with outpatient clinic level
| Regression
Coefficient |
95% Confidence Interval | t-value | p-value | ||
| Lower limit | Upper limit | ||||
| Group N | -0.218 | -0.343 | -0.093 | 3.457 | < 0.001 |
| Cigarette pack year | 0.002 | -0.004 | 0.008 | 0.593 | 0.554 |
| Total fentanyl consumption | -0.001 | -0.003 | 0.001 | -0.651 | 0.516 |
Joint effects of all possible factors which were effective or thought to be effective on operation day HAM-A score in univariate statistical analysis were searched with multivariate linear regression analysis. All variables determined as p < 0.15 in univariate statistical analysis were included in multivariate linear regression models as possible risk factors. Because the data related to HAM-A score not normally distributed, logarithmic transformation was done in regression analysis. After adjusting for other possible confounding factors, the difference between groups in terms of operation day HAM-A score disappeared (B = 0.005, 95% CI:-0.057 – 0.066, p = 0.884). It was observed that statistically significant effects of education level and total fentanyl consumption also disappeared (p = 0.453, p = 0.064). Independently of other risk factors, only outpatient clinic HAM-A score was effective. Operation day HAM-A score was as high as outpatient clinic HAM-A score (B = 0.091, 95% CI:0.066 – 0.115, p < 0.001).
Joint effects of all possible factors which were effective or thought to be effective on change in operation day HAM-A score compared with outpatient clinic score in univariate statistical analysis were searched with multivariate linear regression analysis. All variables determined as p < 0.15 in univariate statistical analysis were included in multivariate linear regression models as possible risk factors. Because the data related to delta HAM-A score were not normally distributed, logarithmic transformation was done in regression analysis. After adjusting for other possible risk factors, there was still more decrease in HAM-A score in Group N than Group NS and this was statistically significant (B = -0.218, 95% CI:-0.343 – -0.093, p < 0.001). It was observed that statistically significant effects of total fentanyl consumption disappeared (p = 0.516).After adjusting for other possible risk factors, cigarette pack year also had no statistically significant effect on change in HAM-A score (p = 0.554).
DISCUSSION:
In this study we observed that HAM-A score was lower in patients who stopped smoking 48 hours before the operation. Also in this group of patients, intraoperative fentanyl requirement was lower.
Surgical operation, thought of receiving anesthesia and fear of staying in hospital are the factors that stimulate preoperative anxiety.9 It has been shown that preoperative anxiety levels increase with the duration of operation.10,11 In addition, hunger and thirst accompanying this waiting period also increases anxiety.12 All patients participating in our study, were hospitalized one night before the operation and preoperative starvation period was limited to twelve hours. Study population consisted of patients who were first on the surgical list. Patients rested in the premedication room and anxiety score of the patients were evaluated there.
Chronic cigarette consumption upregulates nicotinic receptor. Distribution half-life of nicotine is between 15 and 20 min, and half-life in blood is two hours13. Those addicted to cigarette confirm that cigarette calm them when under stress, and helps concentration but there is little scientific evidence available for this In our study, we observed that HAM-A scores were higher in patients who continued smoking.
Moerman et al. reported that patients who don’t have previous anesthesia experience request more information and they are more anxious.14 However it is also reported that characteristics of previous anesthesia experience (positive or negative) can effect preoperative anxiety.14 A study including more than 500 patients reported that age of the patient, type of the surgical procedure and previous anesthesia experience were not related to preoperative anxiety. In our study all patients underwent similar surgical procedure, and it was observed that age, and previous anesthesia experience did not affect preoperative anxiety. Çuvaş et al. stated that having systemic disease, ASA classification and history of previous operation are did not affect anxiety levels.15 In Duman et al.’s study, no correlation was found between VAS scores when compared with preoperative anxiety values in patients who requested more information.16 There results are similar to our study.
Studies report that female patients are more anxious than male patients in the preoperative period.14,16 Studies involving breast surgery and minor surgery with lower expectation can be the reason of this.17 In our study we did not find a relationship between preoperative anxiety and gender.
While some studies report that anxiety increases with the increase in education level, others show that education level does not affect anxiety.18,19 In our study education levels of the patients was similar in both groups.
It has also been reported that if patients stop smoking preoperatively they have lower basal anxiety levels than active smokers.14 But in these studies there was no factor that stimulated stress. Warner et al. showed that preoperative nicotine replacement therapy does not affect anxiety level of smokers in perioperative abstinence status and withdrawal symptoms do not cause a serious clinical problem in perioperative period.20 In Billert et al.’s study it has been reported that preoperative withdrawal does not affect anxiety levels.21 In our study there was no significant difference between group N and group NS in terms of smoking and amount of cigarette consumption. Total opioid consumption and HAM-A anxiety score were lower in the group where there patients stopped smoking. We think smoking cessation decrease patients’ anxiety scores and reduce intraoperative analgesic requirement as a result of it.
HAM-A scale is one of the first scales which was developed to measure the severity of anxiety and is still in common use in clinical practice and by researchers. This scale consist of 14 items. Each items includes a series of symptoms and measures. It includes both psychological anxiety (agitation, psychological stress) and somatic anxiety (physical stress related to anxiety). Despite common use, this scale is criticized because it cannot discriminate between anxiolytic and antidepressant effects and somatic side effects. Despite all, reliability of HAM-A score has been acceptable.22 It has been observed that State Trait Anxiety Inventoryn (STAI), which is one of the anxiety scales in common use, is not explanatory enough in differential diagnosis of anxiety and depressive disorders.23
A relation between operating time and anxiety level has been shown. In a recent study it has been shown that presence of anxiety in the afternoon is a predictor for preoperative anxiety24. We only included patients who were first on the surgical list. Badner et al., concluded that anxiety the night before the operation continued in preoperative period.25 In order that the conditions related to the operating time did not affect our results, we chose patients who were first on the operation list and measured anxiety in the morning.
CONCLUSION:
In conclusion we observed that stopping smoking 48 hours before operation decreased patients’ anxiety in terms of HAM-A scores. We also observed that intraoperative fentanyl requirement was lower in patients who stopped smoking 48 hours before the surgery.
Conflicts of interest: No potential conflicts of interest were disclosed.
Author’s contribution:
SGU & DY: conceiving and designing the study, performing experiment, data collection, writing the manuscript
DY: critical revision of the article and obtaining funding
HS & TD: analyzing and interpreting the data, collecting the data
HBA: statistical analysis
UA: analyzing and interpreting the data, critical revision of the article
MO: data collection
BS: critical revision of the article
REFERENCES:
- Mathews A, Ridgeway V. Personality and surgical recovery: a review. Br J Clin Psychol. 1981 Nov;20(Pt 4):243-60. doi:10.1111/j.2044-8260.1981.tb00525.x [PubMed]
- Egan, KJ, Ready LB, Nessly M, Greer BE. Self-administration of midazolam for postoperative anxiety:a double blinded study. Pain. 1992;49(1):3-8. doi:10.1016/0304-3959(92)90180-J [PubMed]
- Maranets I, Kain ZN. Preoperative anxiety and intraoperative anesthetic requirements. Anesth Analg, 1999;89(6):1346. doi:10.1213/00000539-199912000-00003. [PubMed]
- Anderson KO, Masur FT 3rd. Psychological preparation for invasive medical and dental procedures. Journal of Behavioral Medicine. 1983;6(1):1-40. [PubMed]
- Thomas V, Heath M, Rose D, Flory P. Psychological characteristics and the effectiveness of patient-controlled analgesia. Br J Anaesth. 1995 Mar;74(3):271-6.doi:10.1093/bja/74.3.271. [PubMed]
- Wells JK, Howard GS, Nowlin WF, Vargas MJ. Pre-surgical anxiety and postsurgical pain and adjustment: Effects of a stress inoculation procedure. J Consult Clin Psych. 1986;54(6):831. [Free full text]
- Batra V, Patkar AA, Berrettini WH, Weinstein SP, Leone FT. The genetic determinants of smoking. CHEST Journal. 2003;123(5):1730-1739. doi:10.1378/chest.123.5.1730. [PubMed]
- Watkins SS, Koob GF, Markou A. Neural mechanisms underlying nicotine addiction: acute positive reinforcement and withdrawal. Nicotine Tob Res. 2000 Feb;2(1):19-37. doi:10.1080/14622200050011277. [PubMed]
- Ramsay MAE. A survey of preoperative fear. Anaesthesia. 1972;27(4):396-402. [PubMed] [Free full text]
- Kindler CH, Harms C, Amsler F, Ihde-Scholl T, Scheidegger D. The visual analog scale allows effective measurement of preoperative anxiety and detection of patients’ anesthetic concerns. Anesth Analg. 2000 Mar;90(3):706-12. doi:10.1097/00000539-200003000-00036. [PubMed]
- Soni JC, Thomas DA. Comparison of anxiety before induction of anaesthesia in the anaesthetic room or operating theatre. Anaesthesia 1989;44(8):651-655. doi:10.1111/j.1365-2044.1989.tb13586.x [PubMed] [Free full text]
- Ayoğlu H, Uçan B, Taşçılar Ö, Atik L, Kaptan YM Turan IÖ. Preoperatif Oral Karbonhidrat Solüsyonu Kullanılmasının Hasta Anksiyetesi ve Konforu Üzerine Etkileri. JTAICS/Türk Anestezi ve Reanimasyon Dergisi. 2009;37(6).
- Jarvis MJ. Why people smoke. BMJ 2004;328(7434):277-279. [PubMed] [Free full text]
- Moerman N, van Dam FS, Muller MJ, Oosting H. The Amsterdam preoperative anxiety and information scale (APAIS). Anesth Analg 1996;82(3):445-451. [PubMed]
- Cuvaş Ö, Aslanargun P, Aslan E, Yücel F, Dikmen B, Ceyhan A. Sigara İçiminin Preoperatif Anksiyete Üzerine Etkisi. JTAICS/Türk Anestezi ve Reanimasyon Dergisi. 2010;38(5).
- Duman A, Öğün CÖ, Şahin TK, Sarkılar G, Ökesli S. Preoperatif korku ve endişeyi etkileyen faktörlerin değerlendirilmesi. SÜ Tıp Fak Derg. 2003;19:21-26. [PubMed] [Free full text]
- Grabow L, Buse R. Preoperative anxiety–anxiety about the operation, anxiety about anesthesia, anxiety about pain? Psychother Psychosom Med Psychol. 1990 Jul;40(7):255-63. [PubMed]
- Domar AD, Everett LL, Keller MG. Preoperative Anxiety: Is It a Predictable Entity?. Anesthesia Analgesia. 1989;69(6):763-767. [PubMed]
- Mackenzie JW. Daycase anaesthesia and anxiety A study of anxiety profiles amongst patients attending a Day Bed Unit. Anaesthesia. 1989;44(5):437-440. [PubMed] [Free full text]
- Warner DO, Patten CA, Ames SC, Offord KP, Schroeder DR. Effect of nicotine replacement therapy on stress and smoking behavior in surgical patients. Anesthesiology. 2005;102(6):1138-1146. [PubMed] [Free full text]
- Billert H, Gaca M, Adamski D, Miluska J, Breborowicz G. [Significance of smoking and cigarette abstinence regarding anxiety in gynecologic patients in a perioperative period]. Przegl Lek. 2006;63(10):870-7. [PubMed]
- Caumo W, Schmidt AP, Schneider CN, Bergmann J, Iwamoto CW, Bandeira D, et al. Risk factors for preoperative anxiety in adults. Acta Anaesthesiol Scand 2001;45(3):298-307. doi:10.1034/j.1399-6576.2001.045003298.x [PubMed]
- Kennedy BL, Schwab JJ, Morris RL, Beldia G. Assessment of state and trait anxiety in subjects with anxiety and depressive disorders. Psychiatr Q. 2001 Fall;72(3):263-76. [PubMed]
- Lichtor JL, Johanson CE, Mhoon D, Faure EA, Hassan SZ, Roizen MF. Preoperative Anxiety Does Anxiety Level the Afternoon Before Surgery Predict Anxiety Level Just Before Surgery? Anesthesiology. 1987 Oct;67(4):595-9. [PubMed] [Free full text]
- Badner NH, Nielson WR, Munk S, Kwiatkowska C, Gelb AW. Preoperative anxiety: detection and contributing factors. Canadian Journal of Anaesthesia. 1990;37(4):444-447. [PubMed]

