José M. Beleña, MD, PhD*, MónicaNúñez, MD**, Alfonso Vidal, MD, PhD***, Carmen Gasco, MD, PhD****, Javier YusteMD***** and Amjad Kahn MD, PhD******
*Staff Anaesthesiologist and Assistant Professor,
Department of Anaesthesiology and Critical Care, Sureste University Hospital, Arganda del Rey, Madrid (Spain)
Anaesthesiology and Resuscitation Unit. Department of Pharmacology, Faculty of Medicine. Complutense University of Madrid (Spain)
**Staff Anaesthesiologist, Department of Anaesthesiology and Critical Care, Ramón y Cajal University Hospital, Madrid (Spain)
***Associate Professor; ****Professor Emeritus,
Anaesthesiology and Resuscitation Unit. Department of Pharmacology, Faculty of Medicine. Complutense University of Madrid (Spain)
*****Consultant Anaesthesiologist; ******Chief Anaesthesiologist).
Department of Anaesthesiology and Intensive Care, Dr. Sulaiman Al-Habib Al Takhassusi Hospital,Riyadh (Saudi Arabia)
Correspondence:José M. Beleña, Department of Anaesthesiology and Critical Care. Sureste University Hospital, C/ Ronda del Sur, 10. 28500 Argandadel Rey, Madrid(Spain); Phone: +34 918394184; Fax: +34 918394378; E-mail:josemariabelena@yahoo.es
ABSTRACT
Background: LMA ProsealTM (LMA-P) and i-gelTM are two of the most used supraglottic airway devices (SADs) with an inbuilt drain channel. We compared these devices regarding efficacy, safety, ease of use and incidence of adverse events.
Methodology: We randomized 140 patients undergoing elective laparoscopic cholecystectomy to have either i-gel or LMA-P. We evaluated speed of insertion, success rates, ease of insertion of the drain tube, leak pressure and tidal volume. We also recorded postoperative oropharyngeal discomfort based on sore throat, dysphagia and dysphonia.
Results: I-gel had a lower leak pressure and achieves a lower tidal volume compared to the LMA-P (28.3 ± 3.3 cmH2O versus 30.9 ± 2.6 cmH2O; p = 0.027), as well as a lower tidal volume provided (562.6 ± 41 ml versus 584.8 ± 44 ml; p = 0.025). Insertion times were lower for i-gel compared with LMA-P (10 ± 1.7 versus 11.7 ± 2 s; p = 0.004). Insertion success rate on first attempt as well as drain tube insertion were comparable between groups. I-gel group complained about a slightly higher sore throat scoring at 2 h postoperatively (p = 0.025).
Conclusions: We found that i-gel had a lower leak pressure and achieves a lower tidal volume compared to the LMA-P in anesthetised patients undergoing laparoscopic cholecystectomy. Although i-gel was quicker to insert than LMA-P, it reported higher sore throat scoring at 2 h postoperatively.
Key words: LMA Proseal;i-gel;Laparoscopic cholecystectomy;Airway, leak pressure
Citation:Beleña JM, Núñez M, Vidal A, Gasco C, Yuste J, Kahn A. Comparison of the i-gelTM and the LMA ProsealTM in anesthetized patients undergoing laparoscopic cholecystectomy: a prospective, randomized clinical trial.Anaesth Pain & Intensive Care 2015;19(2):135-40
INTRODUCTION
The Laryngeal Mask Airway ClassicTM (LMA-C) is the most widely studied supraglottic airway device (SAD) and since it was introduced, several devices have been incorporated in order to improve the SAD´s indications, some of them with gastric access incorporation.
A far as we know, there are seven SADs with a drain tube available in the market at this moment: Laryngeal Tube SuctionTM (LTS or LTS-D if disposable), LMA ProsealTM (LMA-P), LMA SupremeTM (LMA-S), i-gelTM and recently The Guardian CPVTM , the BaskaMaskTMand the AmbuAuraGainTM . LMA-P and i-gel are two of the most commonly used devices with gastric access in clinical anesthesia.
These devices are a reasonable choice when performing anesthesia for procedures accompanied by high peak airway pressure, such as laparoscopy. In addition, the drain channel helps to identify the correct tip position just after insertion.1Over the last ten years, some studies have been performed in order to establish the safety of SADs with gastric access for this purpose. In that sense, a number of studies have been performed with LMA-P2,3 and LMA-S4-7 , but we only found a few articles evaluating i-gel for laparoscopic procedures.5,8,9
We present a prospective and randomised study of 140 patients undergoing elective laparoscopic cholecystectomy, comparing the use of i-gel and LMA-P and evaluating in detail their safety, efficacy and ease of use. We also compared the incidence of adverse events, focused on postoperative rate of sore throat, dysphagia or dysphonia.
Our primary outcomes were to measure leak pressure, speed of insertion and success rates. Our secondary outcome was to evaluate the postoperative oropharyngeal discomfort during the patients´ stay in the Postanesthesia Care Unit (PACU).
METHODOLOGY
Local Research Ethics Committee of the Hospital Universitario del Sureste, Arganda del Rey, Madrid, Spain (Chairperson Dr. F.J. Yuste, registration number: HUSE 2012-3) approved this study on 11 October 2012. Written informed consent was obtained from all participants and recruitment ended on 10 June 2013. We prospectively randomized 140 adult patients scheduled for elective laparoscopic cholecystectomy. Patients were excluded if they presented ASA physical status 4 or higher, BMI ≥ 40 kg m–², severe gastro-esophageal reflux disease or known risk of aspiration.
Patients were randomly assigned using computer generation random numbers to one of the two groups, to be managed with either i-gel or LMA-P as SAD.
Midazolam 0.03 mg/kg and remifentanil 0.1 μg/kg/min intravenously were used as premedication and standard anesthetic monitoring was attached. Airway management was performed by four senior anesthesiologists experienced in the use of SADs .
After preoxygenation, anesthesia was induced with intravenous remifentanil 0.3 μg/kg/min and propofol 2-3 mg/kg. We did not use neuromuscular blocking drugs at this time. After optimum conditions for SAD insertion were achieved (relaxation of the jaw, loss of eyelash reflex and onset of apnea), either i-gel or LMA-P was introduced.
Size chosen was based on manufacturer´s recommendations according to the patient´s weight. All the devices were lubricated and the cuff of LMA-P was completely deflated.
The SADs were inserted with the patient´s head in the “semi-sniffing” position using a digital technique. The cuff of LMA-P was inflated to a pressure of 60 cmH2O using a manometer. After insertion, the device was connected to a closed-circuit breathing system under volume-controlled ventilation (TV of 8 ml/kg, RR of 12 breaths/min, I: E ratio of 1:1.5 and fresh gas flow 3 L/min). Successful placement was defined as a square-wave tracing on the capnography with normal end-tidal CO2 (EtCO2) values. After three failed attempts, insertion was considered a failure and endotracheal intubation (ETI) was performed. The time required for successful insertion was defined as the time from removing the face mask to the first square capnogram. In case of ineffective ventilation [hypoventilation (TV < 6 ml/kg) or hypercarbia(> 45 mmHg)], despite a successful placement, the device was removed and reinserted performing correctives maneuvers. If ventilation continued ineffective after repositioning the SAD, it was considered a ventilation failure and ETI was performed.
A suction gastric tube was introduced via the drain tube (12 FG for i-gel and 16 FG for LMA-P) and ease of insertion was scored (easy to insert, minor difficulty to insertion and difficult to insert). A non-blinded observer who was not involved in the study recorded the number of attempts and time needed for the SAD´s insertion as well as ease of the drain tube´s insertion.
Anesthesia was maintained with 6% desflurane in 50% oxygen and air, remifentanil 0.15-0.5 μg/kg/minand rocuronium 0.6 mg/kg. After obtaining and effective and stable airway, leak pressure (LP) was assessed by closing the circuit and allowing a fresh gas flow of 3 L/min to built airway pressure until an audible leak was heard over the mouth (not permitted to exceed 40 cmH2O) 10 .
Ventilatory variables were recorded before and after the pneumoperitoneum, intra-abdominal pressure was held constant at 13 mm Hg and head-up tilt was limited to 30º. Peritoneal insufflation time and anesthetic time were also recorded.
Maximum expiratory tidal volume was recorded over one minute after pneumoperitoneum was established, based on the expiratory tidal volume showed by the ventilator. This measurement corresponds to the maximum expiratory TV value observed over that minute under pneumoperitoneum condition. During emergence and removal, airway complications (laryngeal stridor, laryngospasm, bronchospasm, regurgitation, aspiration, cough or hypoxia) and the presence of blood on device were recorded. Aspiration of gastric contents was defined as either the presence of bilious secretions or particulate matter in the tracheobronchial tree. All patients were closely followed up during anesthesia period, especially when we detected regurgitation of gastric contents observed at the gastric tube. Patients also were followed up at PACU in order to find a clinically detectable pulmonary aspiration and we performed a chest radiograph to discard the presence of infiltrates when clinical suspicion.
Additionally, all patients were interviewed at 2 hours postoperatively by an assessor blinded to the allocation group, about the presence of sore throat, dysphagia and hoarseness. It was assessed using a VAS (0 = no sore throat, dysphagia or dysphonia, 10 = worst sore throat ever, total dysphagia or dysphonia).
Patients received a standard postoperative analgesic regime of dexketoprofen (50 mg) and paracetamol (1 g) IV, analgesic requirements were comparable between both groups.
Statistical analysis:Published data on leak pressure were used to calculate the necessary sample size. Assuming a mean OLP of 26 cmH2O for the i-gel11 and 25 cmH2O for the LMA-P,12 and assuming a standard deviation of 5 cmH2O for all devices, 66 patients per group were needed to detect a clinically significant difference of 10% between the groups with 90% power (1 – β = 0.90) and a significance level of 0.05 (two tailed). A total of 146 patients were consented to account for a 9% dropout rate.
We analysed the data with SPSS version 17 (SPSS Inc., Chicago, Illinois, USA).
The distribution of data was determined using Kolmogorov-Smirnov analysis. Statistical analysis was performed with paired t test, one way ANOVA for repeated measurements and χ2 test for nominal data. Data are mean (± SD) unless otherwise stated. A p-value less than 0.05 was considered significant.
RESULTS
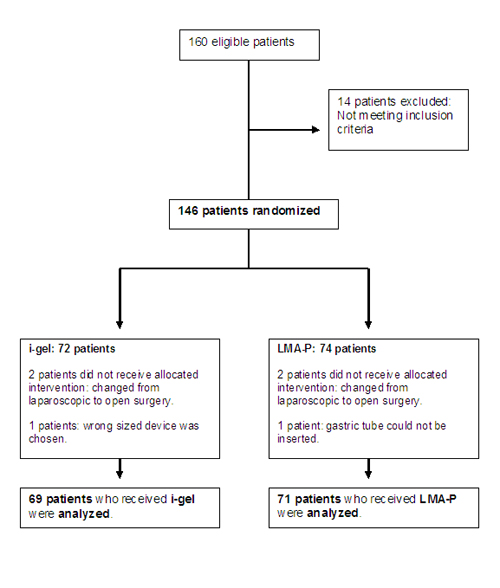
We recruited 146 patients and data were excluded from six randomized patients, four of them after the surgical approach changed from laparoscopy to open surgery, one more patient for a protocol violation (wrong sized i-gel device) and in another patient (LMA-P) gastric tube could not be inserted and had to be intubated for safety reasons. The results of 140 patients (71 LMA-P and 69 i-gel) were finally analyzed (Figure 1).
Figure 1: Patient Flow Diagram.
The groups were comparable for demographic and surgical data (Table 1).
Table 1: Demographic and surgical data
|
Parameter |
LMA-P (n = 71) |
i-gel (n = 69) |
p |
|
Gender (F/M) |
41/30 |
38/31 |
0.45 |
|
Age (yr) |
52 ± 2 |
49 ± 3 |
0.35 |
|
Weight (kg) |
70 ± 2 |
73 ± 3 |
0.54 |
|
Height (cm) |
165 ± 3 |
164 ± 4 |
0.36 |
|
BMI (kg.m-2) |
25 ± 4 |
27 ± 4 |
0.60 |
|
ASA 1/2/3 |
31/30/10 |
25/37/7 |
—– |
|
Surgical time (min) |
75 ± 5 |
70 ± 4 |
0.60 |
|
Peritoneal insufflation time (min) |
55 ± 3 |
53 ± 5 |
0.09 |
|
Duration of anesthesia (min) |
100 ± 7 |
98 ± 8 |
0.53 |
Values are presented as mean ± SD or numbers
The mean leak pressure with i-gel group was significantly lower than in the LMA-P group (28.3 ± 3.3 cmH2O versus 30.9 ± 2.6 cmH2O; p = 0.027). This finding was consistent with a lower tidal volume achieved with i-gel (562.6 ± 41 ml versus 584.8 ± 44 ml; p = 0.025) (Table 2).
Table 2: Safety and efficacy parameters, incidence of complications and postoperative sore throat data
|
Parameters |
i-gel |
LMA-P |
p-value |
|
Safety/Feasibility parameters |
|||
|
Leak pressure (cmH2O) |
28.3 ± 3.3 |
30.9 ± 2.6 |
0.027* |
|
Mean peak airway pressure before carboperitoneum (cmH2O) |
18 ± 3 |
19 ± 4 |
0.75 |
|
Mean peak airway pressure after carboperitoneum (cmH2O) |
25.5 ± 3 |
24.1 ± 3.5 |
0.15 |
|
Mean peak airway pressure after carboperitoneum and reverse Trendelenburg (cmH2O) |
25.3 ± 3 |
25 ± 3.4 |
0.17 |
|
Tidal volume (ml) |
562.6 ± 41 |
584.8 ± 44 |
0.025* |
|
Efficacy parameters |
|||
|
First attempt success rate (%) |
80 |
74 |
0.09 |
|
Time taken for insertion (s) |
10 ± 1.7 |
11.7 ± 2 |
0.004* |
|
Ease for gastric tube insertion: easy/ minor difficulty/difficult/impossible (%) |
78/20/2/0 |
72/23/5/0 |
0.07 |
|
Complications |
|||
|
Cough (%) |
8.5 |
10 |
0.80 |
|
Blood on mask (%) |
4 |
7 |
0.59 |
|
Postoperative Sore Throat At 2h (mean in a 0-10 VAS) |
0.5 ± 0.6 |
0.25 ± 0.5 |
0.025* |
Values are presented as mean ± SD, numbers or percentage. * p< 0.05.
I-gel showed shorter mean time to insertion compared with LMA-P (10 ± 1.7 versus 11.7 ± 2 s), and it proved to be inserted 1.7 s quicker than LMA-P (p = 0.004) (Table 2).
There were no significant differences in success rate on first attempt insertion between groups: 80% for i-gel versus 74% for LMA-P (p = 0.09). No failed insertions were recorded in either group.
Both groups were comparable regarding ease of insertion of the drain tube, 78% of i-gel and 72% of LMA-P were graded as “easy to insert” (p = 0.07).
No differences were found between groups relating intraoperative complications and noepisodes of laryngeal stridor, laryngospasm, bronchospasm, hypoxia, regurgitation or aspiration were seen. Frequency of coughing and visible blood at removal of the device were comparable in both groups (p = 0.804 and p = 0.593, respectively).
There was a higher incidence of postoperative sore throat in i-gel group compared with LMA-P group (p = 0.025). Patients from i-gel group suffered more sore throat (0.25 more points at the VAS scale) than LMA-P group during their stay at the PACU. In addition, VAS values by categories (VAS=0/VAS=1-3/VAS≥4) were: i-gel = 53%/47%/0% and LMA-P = 77%/23%/0%. Four patients reported dysphagia (two in LMA-P and two in i-gel groups) and one patient complained of dysphonia (i-gel) at that time.
DISCUSSION
A significant portion of current literature studying the use of SADs with gastric access in laparoscopy focuses on comparisons between LMA-P, LMA-S and i-gel. Most of the studies compared these SADs for gynaecological laparoscopic procedures and just a few authors compared the use of these devices in patients undergoing laparoscopic cholecystectomy.
Leak pressure test is commonly performed to qualify the airway seal when a SAD is used. Leak pressure is significant to indicate the success of positive pressure ventilation and the degree of airway protection. It is regarded as the most important value when testing how suitable a SAD is for laparoscopy use.3,13
LMA-P recorded a better LP than i-gel, it may have been due to its bigger and inflatable double cuff, the deeper bowl, the proximal wedge shape of the cuff and its corresponding larger surface area in comparison to i-gel. This last device has smaller cuffless bowl made of a thermoplastic elastomer called SEBS (Styrene Ethylene Butadiene Styrene).
The LP values that we found were consistent with a lower tidal volume achieved with i-gel compared to LMA-P.
Our results are similar to Sharma et al., who found that LMA-P achieved higher LP than i-gel for laparoscopic cholecystectomy while the dynamic compliance was higher for i-gel.8 Woo et al reported that LP did not vary significantly between these two groups; however, their work was performed in females undergoing gynecological laparoscopy.9
We found that i-gel was 1.7 sec quicker to insert than LMA-P. Other authors also found a shorter time to insertion for i-gel as compared with LMA-P, although these studies were performed in non-laparoscopic procedures.14-16 However, this little difference found is clinically irrelevant and due to this fact no differences were found by other authors.8,9
The success rate on the first attempt was not significantly different between the groups. Most of the published data did not report differences regarding first-time success rate.8,9,14 Although two studies reported that i-gel was easier to insert, using an insertion of the device scoring.15,16
Ease of insertion of the gastric tube was comparable between i-gel and LMA-P in our study, as showed by the majority of authors. In fact, i-gel has a narrower drain access which only allows the introduction of a smaller sized gastric tube when compared to LMA-P, but it had no clinical significance.
With regard to intraoperative adverse events, no differences were found, in this sense no episodes of laryngospasm, bronchospasm, hypoxia or regurgitation were seen. Only coughing and visible blood at removal of the device were reported and they were comparable in both groups (p = 0.804 and p = 0.593, respectively). Our findings are similar to the results obtained by other authors.8,14,16
Incidence of postoperative discomfort during the first 2 hours after anesthesia, showed significant differences between devices, so that i-gel group experienced higher sore throat at that moment.
Most of the studies did not find differences concerning postoperative sore throat or other complaints among devices during postoperative period.8,9,14,16
We observed a significant statistical difference (p = 0.025) related to sore throat during the first 2 hours in PACU, whereas dysphagia and dysphonia were comparable between groups. Actually, this result is difficult to explain, despite our findings suggest that i-gel may be a more injuring device than LMA-P regarding airway morbidity, there is not enough argument to draw a conclusion.In any case, we have to consider that a mean difference about 0.25 points in VAS is clinically insignificant with respect to the incidence of postoperative sore throat, which has no clinical relevance. Consequently, more studies are needed in order to explain the small differences that we found.
LIMITATIONS
Our study had a number of limitations. Firstly, the observer who measured the insertion times and events was not blinded to the type of device. Postoperative outcome assessors were blinded to the group assignment in order to mitigate that limitation. Secondly, the anesthesiologist who inserted the device, had less experience with i-gel than using LMA-P, due to the late market appearance of i-gel.
CONCLUSION
We conclude in this randomised study, that i-gel had a lower leak pressure and achieves a lower tidal volume compared to the LMA-P in anesthetised patients undergoing laparoscopic cholecystectomy. I-gel was more rapidly placed than LMA-P, although we found not differences in first time success rate and ease of the drain tube´s insertion. Our study showed that i-gel reached a slightly higher sore throat scoring during 2 h-postoperative period.
Disclosure of funding: No funds were received for the study from any of the following organizations: National Institutes of Health (NIH), Spanish Society of Anesthesiology (SSAR), Regional Government of Madrid (RGM), neither from other organization, including departmental or institutional funding.
Conflict of interest: None
Authors’ contribution:JMB: Study conception and design, acquisition of data, analysis and interpretation of data, drafting of manuscript and critical revision.
MN: Study conception and design, acquisition of data, drafting of manuscript and critical revision.
AV: Study conception and design, analysis and interpretation of data, drafting of manuscript and critical revision.
CG: Acquisition of data, drafting of manuscript and critical revision.
JY: Drafting of manuscript and critical revision
AK: Drafting of manuscript and critical revision
REFERENCES
- O’Connor CJ Jr, Stix MS, Valade DR. Glottic insertion of the ProSeal LMA occurs in 6% of cases: a review of 627 patients.Can J Anaesth 2005; 52(2):199-204.[PubMed]
- Seet E, Rajeev S, Firoz TYousaf F, Wong J, Wong DT, et al. Safety and efficacy of laryngeal mask airway Supreme versus laryngeal mask airway Proseal: a randomized controlled trial. Eur J Anaesthesiol 2010; 27:602-7.[PubMed]
- Kini G, Devanna GM, Mukkapati KR, Chaudhuri S, Thomas D. Comparison of I-gel with proseal LMA in adult patients undergoing elective surgical procedures under general anesthesia without paralysis: A prospective randomized study. J Anaesthesiol Clin Pharmacol 2014; 30:183-7.[PubMed][Free Full Text]
- Chauhan G, Nayar P, Seth A et al. Comparison of clinical performance of the I-gel with LMA proseal. J Anaesthesiol Clin Pharmacol 2013;29:56-60.[PubMed][Free Full Text]
- Maltby JR, Beriault MT, Watson NC, Liepert D, Fick GH: LMA-ClassicTM and LMA-ProSealTMare effective alternatives to endotracheal intubation for gynecologic laparoscopy. Can J Anesth 2003; 50:71-7.[PubMed][Free Full Text]
- Natalini G, Lanza G, Rosano A, Dell´Agnolo P, Bernardini A: Standard Laryngeal Mask AirwayTM and LMA-ProSealTM during laparoscopic surgery. J Clin Anesth 2003; 15:428-32.[PubMed]
- Lee AK, Tey JB, Lim Y, Sia AT. Comparison of the single-use LMA Supreme with the reusable Proseal LMA for anaesthesia in gynaecological laparoscopic surgery. Anaesth Intensive Care 2009; 37:815-9.[PubMed]
- Teoh WH, Lee KM, Suhitharan T,Yahaya Z, Teo MM, Sia AT. Comparison of the LMA Supreme vs i-gel in paralysed patients undergoing gynaecological laparoscopic surgery with controlled ventilation. Anaesthesia 2010; 65:1173-9.[PubMed][Free Full Text]
- Yao T, Yang XL, Zhang F Li N, DU HQ, Wang DX, et al. The feasibility of Supreme laryngeal mask airway in gynaecological laparoscopy surgery. Zhonghua Yi XueZaZhi 2010; 90:2048-51.[PubMed]
- Beleña JM, Nuñez M, Anta D, Carnero M, Gracia JL, Ayala JL, et al. Comparison of LMA SupremeTM and LMA ProsealTM with respect to oropharyngeal leak pressure in patients undergoing anaesthesia during laparoscopic cholecystectomy:a randomized controlled trial. Eur J Anaesthesiol 2013; 30:119-23.[PubMed][Free Full Text]
- Sharma B, Sehgal R, Sahai C, Sood J. PLMA vs. I-gel: A Comparative Evaluation of Respiratory Mechanics in Laparoscopic Cholecystectomy. J Anaesthesiol Clin Pharmacol 2010; 26:451-7.[PubMed][Free Full Text]
- Woo JJ, Sang YC, Seong JB, Kyoung HK. Comparison of the Proseal LMA and Intersurgical I-gel during gynaecological laparoscopy. Korean J Anesthesiol 2012; 63:510-14.[PubMed][Free Full Text]
- Keller C, Brimacombe JR, Keller K, Morris R: Comparison of four methods for assessing airway sealing pressure with the laryngeal mask airway in adult patients. Br J Anaesth 1999; 82:286-7. [PubMed]
- Russo SG, Cremer S, Galli T et al. Randomized comparison of the i-gel, the LMA Supreme and the Laryngeal Tube Suction-D using clinical and fibreoptic assessment in elective patients. BMC Anesthesiology 2012; 12:18. [PubMed][Free Full Text]
- Timmermann A, Cremer S, Eich C, Kazmaier S, Bräuer A, Graf BM, et al.: Prospective clinical and fiberoptic evaluation of the Supreme Laryngeal Mask AirwayTM . Anesthesiology 2009; 110:262-5.[PubMed][Free Full Text]
- Das A, Majumdar S, Mukherjee A et al. i-gel™ in Ambulatory Surgery: A Comparison with LMA—ProSeal™ in Paralyzed Anaesthetized Patients. J ClinDiagn Res 2014, 8:80-84.[PubMed][Free Full Text]