Nagesh Jambure, MD, FCA1 and Amarja Sachin Nagre, MD, DM, FCA1
1MGM Medical College / MGM Medical Centre and Research Institute, Aurangabad, Maharashtra, (India)
Correspondence: Dr Nagesh Jambure, Flat 13, 5th Floor, SAI Heritage, Ulkanagari, Aurangabad, Maharashtra, (India); Phone: +9579571122; E-mail: drnagesh83@gmail.com
ABSTRACT
Objective: The aim of study is to evaluate the preoperative sedative effects of intranasal dexmedetomidine as compared to oral midazolam as preanesthetic medication in children undergoing cardiac catheterization for diagnostic and/or therapeutic procedure. We aimed to compare the effects of drug between two groups.
Design: Prospective, randomized, double-blind, controlled study.
Methodology: 61 pediatric patients of either sex between the ages 2-10 years were recruited for cardiac catheterization for diagnostic and/or therapeutic procedural sedation. Patients were randomly divided into two groups; 31 patients (Group D) received intranasal dexmedetomidine 2 μg/kg by mucosal atomiser spray and 30 patients (Group M) received oral midazolam 0.5 mg/kg. Behavior score, sedation score, separation score and vital signs were recorded before shifting the patient to cathlab and at induction of anesthesia. The results were analyzed statistically.
Results: The result in the study shows that, group D patients (2 μg/kg) has statistically significant faster onset of action, separation score, sedation score, behavior score at induction and at 15 and 30 minutes as compared to group M (0.5 mg/kg).
Conclusion: Transnasal dexmedetomidine has faster onset of action, separation score, sedation score, and behavior score than oral midazolam for cardiac cath procedures in pediatric patients.
Keywords: Intranasal; Dexmedetomidine; Midazolam; Pediatric;
Premedication; Preanesthetic Medication
Citation: Jambure N, Nagre AS. Comparison of Intranasal dexmedetomidine and oral midazolam as premedication for cardiac catheterization procedure in pediatric patients. Anaesth Pain & Intensive Care. 2016;20 Suppl 1:S48-S52
Received: 20 June 2016; Reviewed: 27 June, 16 August 2016; Corrected: 29 June, 5 September 2016; Accepted: 30 September 2016
INTRODUCTION
Stranger anxiety and fear of separation from parents is common in pediatric patients.1 Preanesthetic medication in children should aim at relieving the stress response with preservation of hemodynamic parameter, facilitate the induction of anesthesia without prolonging the recovery and to produce amnesia.2 Therefore, pediatric pain management is challenging and one of the hallmark of modern anesthesiology. Numerous premedicants have been used through various routes; each route having its own merits and demerits.
Dexmedetomidine is a highly selective α2-adrenoceptor agonist which is eight times more α2 to α1-receptor selective than clonidine (1620:1 versus 200:1).3 As an α2-adrenoceptor agonist, dexmedetomidine has both sedative and analgesic effects without respiratory depression.4 The α2-adrenoceptor agonists achieve sedative effect through α2-adrenoceptors in the locus ceruleus in central nervous system. In addition, the delivery has extended to extra vascular routes including oral, buccal, transdermal, intramuscular and intranasal administration.5,6,7 These favorable properties have encouraged its use for a wide range of clinical conditions such as an anesthetic adjunct, postoperative sedation and pediatric premedication.5 81.8% (72.6–92.1%) of the nasally delivered medication actually ends up in the blood stream. The relatively large and well vascularized surface of the nasopharyngeal mucosa results in rapid absorption of delivered drug. The brain and nasal mucosa has neural connection which delivers the drugs to central nervous system.8,9,10 High first-pass metabolism of drug can be avoided by nasal administration.11
Thus, we conducted a study to compare the effects of transnasal dexmedetomidine and oral midazolam as premedicant in children undergoing cardiac catheterization for diagnostic and/or therapeutic procedure.
METHODOLOGY
After obtaining the local ethics committee approval and written informed consent from parents, 61 patients of either sex selected, between the ages 2-10 years. We examined the sedative and analgesic efficacy of intranasal dexmedetomidine and oral midazolam, in children undergoing cardiac catheterization for diagnostic and/or therapeutic procedural sedation like ASD device closure, VSD device closure, PDA device closure, balloon dilatation of aortic and pulmonary valve or cath angiography to decide operability of patient for surgical procedure. All patients were kept nil by mouth before the procedure. The oral group received midazolam 0.5 mg ̷ kg oral formulation and the intranasal group received dexmedetomidine 2µg ̷ kg diluted with 1 ml of distilled water, 0.5 ml in each nostril, by mucosal drug atomiser in the supine position. Patient with known allergy, oral and nasal deformity, mental retardation, A-V block, hepatorenal dysfunction, severe pulmonary hypertension, heart failure were excluded from study.
Patient were kept in cath lab recovery and connected to standard monitors. Baseline heart rate (HR), blood pressure (BP) and oxygen saturation (SpO2) were measured before premedication and Readings were taken at 15-min intervals up to 60 min, until child was separated from the parents. Premedication was given approximately 60min before induction of anesthesia. After the transnasal dose, sedation status was evaluated with 6-point score scale, and Behavior score and the ease of separation score were assessed with 4-point score scale by the blind observer.5 Mode of procedural IV sedation was decided by the attending anesthesiologist. A satisfactory sedation scores were considered in between 1 and 4 and unsatisfactory when rated 5 or 6. Children with scores of 1 or 2 were considered as a satisfactory behavior and separation scores and considered as unsatisfactory when behavior and separation scores were 3 or 4. The onset of action is defined as the time from the administration of the drug to the beginning of drowsiness. Children were also observed constantly for any side effect like nausea, vomiting, pruritus.
When procedure was finished, the child was placed in the recovery position and allowed to wake up naturally in the post cath ward. The time to achieve Aldrete score of 10, to be discharged from cath lab recovery, was recorded when child was awake, with vital signs within 20% of baseline values.
Statistical Analysis: Statistical analysis was done with the help of SPSS software. Sample size of 61 patients was calculated to be enrolled in the study. Quantitative data were presented with the help of mean and standard deviation. Comparison among study groups was done with the help of unpaired T-test. Levene’s test was used for equality of variances and t-test for equality of means. P value < 0.05 was taken as a level of significance.
Table 1: Evaluation scales
| Sedation score
1. Does not respond to mild prodding or shaking 2. Responds only mild prodding or shaking 3. Responds only after name is called loudly or repeatedly 4. Lethargic response to name spoken in normal tone 5. Appear asleep but respond readily to name spoken in normal tone 6. Appear alert and awake, response readily to name spoken in normal tone |
| Behavior scores
1. Calm and cooperative 2. Anxious but reassurable 3. Anxious and not reassurable 4. Crying, or resisting |
| Separation score
1. Patient unafraid, cooperative, asleep Excellent 2. Slight fear or crying, quite with reassurance 3. Moderate fear, crying not quite with reassurance 4. Crying need for restraint |
Result
Both the groups were comparable with regard to age and weight. In the present study, we assessed the onset, sedation, behavior, separation score and hemodynamic using the evaluation scale (Table 1). Three patient resisted intranasal drug administration were also included in study.
Table 2: Demographic profile
Weight (kg)**17.58 ± 6.6919.07 ± 6.760.391
| Variable | Group D
(N=31) |
Group M
(N=30) |
P Value |
| Male* | 27(87.1%) | 19(63.3%) | 0.06 |
| Female* | 4(12.1%) | 11(36.7%) | 0.06 |
| Age (Years)** | 6.16 ± 2.37 | 5.83 ± 2.77 | 0.62 |
*N(%); **mean ± SD
Comparison of demographic profile of patients in groups, shows that mean age was 6.16 ± 2.37 yr and 5.83 ± 2.77 yr in group D and group M respectively. Mean weight was 17.58 ± 6.69 kg and 19.07 ± 6.76 kg in two groups respectively which is comparable and not significant.
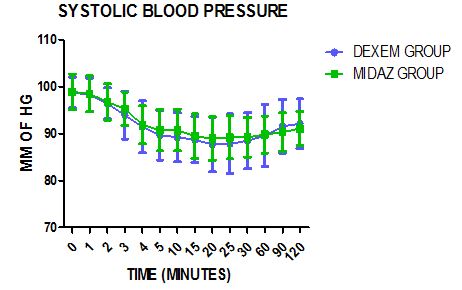
Figure 1: Systolic blood pressure
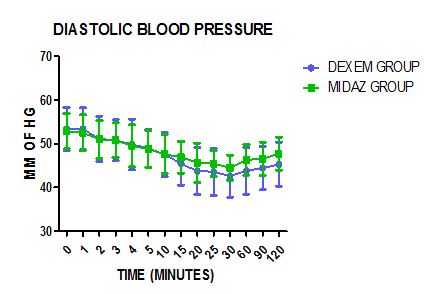
Figure 2: Diastolic blood pressure
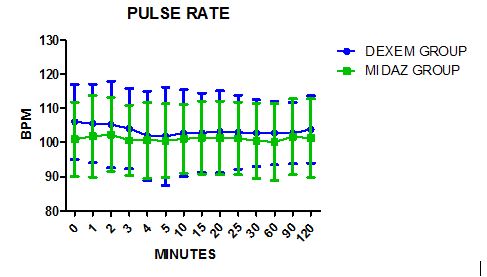
Figure 3: Pulse rate
Figures 1, 2 and 3 show the comparison of preoperative vital signs in midazolam group and dexmedetomidine group. It suggest that mean systolic blood pressure, diastolic blood pressure and pulse rate are comparable and the difference is not statistically significant. The vital signs remained stable and comparable in both the groups throughout 120 min.
Table 3: Comparative analysis of sedation data in two groups (Mean ± SD, P < 0.05 Significant)
| Parameter | Group D
(N=31) |
Group M
(N=30) |
P Value |
| Onset of Action | 20.3 ± 4.39 | 27.03 ± 3.39 | .000 |
| Sedation Score Induction | 3.03 ± 0.48 | 4.03 ± 0.41 | .000 |
| Sedation Score 15 | 4.52 ± 0.68 | 5.4 ± 0.56 | .000 |
| Sedation Score 30 | 2.29 ± 0.64 | 3.33 ± 0.66 | .000 |
| Behavior Score Induction | 2.1 ± 0.4 | 2.83 ± 0.38 | .000 |
| Behavior Score 15 | 2.58 ± 0.5 | 3.6 ± 0.49 | .000 |
| Behavior Score 30 | 1.58 ± 0.5 | 2,57 ± 0.50 | .000 |
| Separation Score | 1.58 ± 0.5 | 2.67 ± 0.48 | .000 |
| Aldrete score of 10 | 55.16 ± 9.68 | 57.17 ± 2.84 | 0.28 |
As shown in table no 3, mean time for onset of action was 20.3 ± 4.39 and 27.03 ± 3.39 in group D and group M respectively. It was found that difference was significant and the time of onset of action is faster in group D than group M. Sedation score and Behavior score at 15 min in group D is satisfactory while group M is unsatisfactory, and statically significant at 30 min and at induction in group D than group M. Separation scores is also satisfactory in intranasal group. Time to achieve Aldrete score of 10 (time to be discharged from cath lab recovery) was similar in both groups. There were no children had reduction of spo2 below 95%.Two children in the intranasal group had bradycardia, one had hypotension and one children of the oral group had bradycardia. None of the patients required any pharmacological intervention.
Discussion-
Premedication is commonly used in pediatric patients to relieve the separation anxiety, to improve patient comfort & to make the procedure smooth and efficient. Intranasal medication offers a truly “needleless” solution to drug delivery. This route is easy, convenient, painless, comfortable, and avoids destruction by hepatic first pass metabolism. Dexmedetomidine is colorless, odorless, does not cause mucosal stimulation, and it has very good sedative, anxiolytic, causing no respiratory depression making it suitable for intranasal administration.12,13 In comparison, midazolam causes respiratory depression, excessive sedation, delirium, prolonged recovery time and so on.
Drugs absorbed via the nasal mucosa riches the vascular plexus of the nose, which directly enter the circulation and it also absorbed through the olfactory mucosa into the CSF – giving rapid brain levels of the drug.14,15
Particle size 10-50 microns adheres best to the nasal mucosa. Smaller particles pass on to the lungs, larger particles form droplets and run-out of the nose. Broad 30 micron spray ensure excellent mucosal coverage,16 and hence results in better absorption.17
In our study, we found that 2 µg/kg dexmedetomidine had statistically significantly faster onset i.e. 20 minutes. Telon et al. also used 2 μg/kg intranasal dexmedetomidine, and they observed that dexmedetomidine was more effective than oral midazolam as a preoperative sedative and the onset of action was 15 minutes.18 Yuen et al shows that 1 μg/kg intranasal dexmedetomidine has onset of sedation of approximately 25 minutes.19
We observed that the intranasal group achieved a better sedation score and behavior score of 3 or more at 15 min, 30 min and at induction than oral midazolam group. The separation scale was lower and statistically significant in group D.
Yuen compare the effects intranasal dexmedetomidine (0.5 µg/kg and 1 µg/kg) with oral midazolam (0.5 mg/kg) as a premedication for minor surgery in 96 children of 2- 12 years old. The results showed that children were significantly more sedated with intranasal dexmedetomidine than oral midazolam. There were no differences in parental separation acceptance and behavior score at induction or wake-up behavior score. 5
Yuen et al. also studied 116 children between 1 and 8 years of age, who received an intranasal dexmedetomidine of either 1 µg/kg and/or 2 µg/kg as a premedication. They observed adequate sedation in 53% of the children in the lower dose group at the time of induction versus 66% in the higher dose group.12 Cimen and colleagues enrolled 62 children (2–6 years of age) scheduled to undergo minor elective surgery into a randomized, double-blind trial comparing buccal and intranasal dexmedetomidine as a pre-induction sedative; 1 µg/kg dose of dexmedetomidine was given in both groups, 45 minutes prior to anesthetic administration. Sedation scores were significantly higher in the intranasal group, beginning at the 10 minutes and continuing until the final assessment at 45 minutes. Ease of parental separation was considered satisfactory in 75.5% of the intranasal group, compared to only 16.2% of the buccal group.20
In the present study, there was a no statistically significant decrease in SBP, DBP and HR from baseline up to 60 min after the administration of intranasal dexmedetomidine and oral midazolam. There was no significant reduction in SpO2 below 95% in both groups.
CONCLUSION
Thus from the results of our study, it is concluded that premedication with intranasal dexmedetomidine had statistically significantly faster onset, and lower sedation, behavior and separation scores, compared to oral midazolam. Moreover, 2 µg/kg dose of intranasal dexmedetomidine has faster onset of action than 1 µg/kg.
Acknowledgement-
We thank Dr. Antony Jorge, DM (Cardiac anesthesia), Sri Jayadeva Institute of Cardiology, Bangalore, for his statistical assistance.
Conflict of interest: Nil declared.
Authors’ contribution: Both authors took equal part in conduct of study and manuscript preparation
REFERENCES
- Kossowsky J, Wilhelm FH, Roth WT, Schneider S. Separation anxiety disorder in children: disorder-specific responses to experimental separation from the mother. J Child Psychol Psychiatry. 2012;53(2):178–87. [PubMed] DOI:10.1111/j.1469-7610.2011.02465.x
- Morgan-Hughes JO,Bangham JA. Preinduction behaviour of children. 1990;45(6):427-35. [PubMed] DOI:10.1111/j.1365-2044.1990.tb14326.x
- Bhana N, Goa KL, McClellan KJ. Dexmedetomidine.Drugs. 2000;59(2):263–8. [PubMed]
- Tsifansky, Michael D, Schmitt, Carol G, Muñoz, Ricardo A. Dexmedetomidine: do we know enough?.Pediatr Crit Care Med. 2007;8(5):492-3. [PubMed] DOI:10.1097/01.PCC.0000269380.66845.21
- Yuen VM, Hui TW, Irwin MG, Yuen MK. A comparison of intranasal dexmedetomidine and oral midazolam for premedication in pediatric anesthesia: a double-blinded randomized controlled trial.Anesth Analg, 2008;106(6):1715-21. [PubMed] DOI:10.1213/ane.0b013e31816c8929
- Anttila M,Penttilä J, Helminen A, Vuorilehto L, Scheinin H. Bioavailability of dexmedetomidine after extravascular doses in healthy subjects. Br J Clin Pharmacol. 2003;56(6):691-3. [PubMed] DOI: 10.1046/j.1365-2125.2003.01944.x
- Kivisto KT, Kallio A, Neuvonen PJ. Pharmacokinetics and pharmacodynamics of transdermal dexmedetomidine. Eur J Clin Pharmacol. 1994;46(4):345-9. [PubMed] DOI:10.1007/BF00194403
- Illum L. Transport of drugs from the nasal cavity to the central nervous system. Eur J Pharm Sci. 2000;11(1):1-18. [PubMed]
- Mathison S, Nagilla R, Kompella UB. Nasal route for direct delivery of solutes to the central nervous system: fact or fiction? J Drug Target. 1998;5(6):415-41. [PubMed] DOI: 10.3109/10611869808997870
- Thorne RG, Frey WH 2nd. Delivery of neurotrophic factors to the central nervous system: pharmacokinetic considerations. Clin Pharmacokinet. 2001;40(12):907-46. [PubMed] DOI: 10.2165/00003088-200140120-00003
- Knoester PD, Jonker DM, Van Der Hoeven RT, Vermeij TA, Edelbroek PM, Brekelmans GJ, et al.Pharmacokinetics and pharmacodynamics of midazolam administered as a concentrated intranasal spray. A study in healthy volunteers. British Journal of Clinical Pharmacology. 2002;53(5):501-7. [PubMed]
- Yuen VM, Hui TW, Irwin MG, Yao TJ, Chan L, Wong GL, Shahnaz MH, et al. A randomised comparison of two intranasal dexmedetomidine doses for premedication in children. Anaesthesia. 2012 Nov;67(11):1210–6. [PubMed] DOI: 10.1111/j.1365-2044.2012.07309.x.
- Ghali AM, Mahfouz AK, Al-Bahrani M. Preanesthetic medication in children: a comparison of intranasal dexmedetomidine versus oral midazolam. Saudi J Anaesth. 2011;5(4):387–91. [PubMed] DOI: 10.4103/1658-354X.87268
- Walberg EJ, Wills RJ, Eckhert J. Plasma concentrations of midazolam in children following intranasal administration.Anaesthesiology. 1991;74(2):233–45. [PubMed]
- Rey E, Delaunay L, Pons G, Murat I, Richard MO, Saint-Maurice C et al. Pharmokinetics of midazolam in children – comparative study of intranasal and intravenous administration.Eur J Clin Pharm. 1991;41:355–7. [PubMed] DOI: 10.1007/BF00314967
- Holsti M, Dudley N, Schunk J, Adelgais K, Greenberg R, Olsen C, et al. Intranasal midazolam versus rectal diazepam for the home treatment of acute seizure in paediatric patients with epilepsy.Arch Pediatr Adolesc Med. 2010;164(8):747-53. [PubMed] DOI: 10.1001/archpediatrics.2010.130.
- Wolfe TR, Bernstone T. Intranasal drug delivery: an alternative to intravenous administration in selected emergency cases. J Emerg Nurs. 2004;30(2):141–7. [PubMed] [Free Full Text] DOI: 10.1016/j.jen.2004.01.006
- Talon MD, Woodson LC, Sherwood ER, Aarsland A, McRae L, Benham T. Intranasal dexmedetomidine premedication is comparable with midazolam in burn children undergoing reconstructive surgery. J Burn Care Res. 2009;30(4):599–605. [PubMed] doi: 10.1097/BCR.0b013e3181abff90
- Yuen VM, Hui TW, Irwin MG, Yao TJ,Wong GL,Yuen MK. Optimal timing for the administration of intranasal dexmedetomidine for premedication in children. Anesthesia. 2010;65(9):922–9. [PubMed] DOI: 10.1111/j.1365-2044.2010.06453.x
- Cimen ZS, Hanci A, Sivrikaya GU,Kilinc LT,Erol MK. Comparison of buccal and nasal dexmedetomidine premedication for pediatric patients. Pediatr Anesth. 2013;23(2):134–8. [PubMed] DOI: 10.1111/pan.12025

