Shashank Chitmulwar, MD1, Charulata Deshpande, MD, DA2
1Resident; 2Professor
Department of Anesthesiology, Topiwala National Medical College & BYL Nair Charitable Hospital, Mumbai, Maharashtra, (India)
Correspondence: Dr. Charulata Deshpande, 2/24, Haji Ali Govt. Colony, K. Khadye Marg, Mumbai-400 034, Maharashtra, (India); Phone: +91-022-23542972, Mobile: 09322655611, 09820345856; E-mail: desh56@hotmail.com
ABSTRACT
Background & Objective: A number of supraglottic airway devices (SADs) are being used for airway management and newer devices are being introduced. This study compared insertion characteristics of two SADs namely LMA Supreme (LMAS) and Laryngeal tube with suction (LTS) in short duration surgery, including insertion success rate, ease of insertion, time taken to insert and the number of attempts required to secure the airway.
Methodology: This prospective analytical cohort study compared the insertion characteristics for two devices in short duration surgeries. Sixty six ASA Class I and II patients were divided into two groups of 33 each.
Insertion characteristics of the two airway devices were assessed for insertion success rate, ease of insertion, number of insertion attempts, time required for successful insertion and leak pressure. Ease and time for insertion of Ryle’s tube, hemodynamic and respiratory parameters during and immediately post insertion as well as postoperative airway morbidity (sore throat, dysphagia and hoarseness) was also compared.
Statistical analysis: Data was analyzed with SPSS statistical software. Statistical significance: p value < 0.05 was considered to be statistically significant.
Results: Both LMAS and LTS secured effective airway in less than 30 sec. LTS was inserted in first attempt in 69.7% patients compared to 84.8% in LMAS group. LTS was easy to insert with no resistance in 42.4% patients and LMAS in 69.7% patients. Mean time for establishment of an effective airway was 24.06 ± 2.54 sec and 20.39 ± 2.19 sec with LTS and LMAS respectively while for Ryle’s tube (RT) insertion it was 18.70 ± 2.40 and 17.27 ± 2.30 sec. LMAS was associated with lower leak pressure and thus lower incidence of laryngotracheal complications.
Conclusion: Both LMAS and LTS are useful alternatives to endotracheal intubation and provide effective and safe airway within 30sec. Success rate of insertion at first attempt is higher with LMAS. The LMAS was easier and faster to insert than the LTS and RT insertion was easier and faster through LMAS. The airway leak pressure was higher with LTS. Both devices are associated with minimal hemodynamic response. Incidence of post-operative airway morbidity was less with LMAS. LMAS was found to be a reliable and better airway management option for patients undergoing short surgical procedures under general anesthesia.
Key words: Supraglottic airway devices; Supreme LMA; Laryngeal Tube with suction; Leak pressure
Citation: Chitmulwar S, Deshpande C. Comparison of insertion characteristics between LMA- Supreme and Laryngeal tube with suction in patients undergoing short duration surgery: a prospective analytical cohort study. Anaesth Pain & Intensive Care 2017;21(2):187-193
Received: 5 Dec 2016, Reviewed: 25 Oct, 22 Nov 2016, Corrected: 12 Mar 2017, Accepted: 19 Apr 2017
INTRODUCTION
A number of supraglottic airway devices (SADs) have been introduced in airway management, and offer a simple and effective alternative to endotracheal intubation.1-3
There has been a rapid rise in day care surgery throughout the world. In our institute the percentage of day care surgeries is around 15-20%. With increase in the popularity of the day care surgeries, SADs have become more popular among anesthesiologists as they are less invasive and can be used in a spontaneously breathing patient without the use of a muscle relaxant. This leads to shorter stay in post-anesthesia care unit and early discharge from hospital.4-6
LMA Supreme (LMAS) and Laryngeal Tube with Suction (LTS) are second generation SAD that provide gas tight seal and have a gastric drainage facility thus overcoming the disadvantage of the risk of aspiration with the use of classic LMA. LMAS is widely accepted in the airway management during short duration elective surgical procedures.5,6 We wanted to evaluate and compare the insertion success rate, insertion characteristics as well as the quality of airway secured using LTS in patients presenting for short duration surgeries at our hospital. We compared these findings with LMAS.
METHODOLOGY
This study was conducted at a tertiary health care center during the period July 2013 to February 2015.
After obtaining permission from the institutional ethics committee and written informed consent 66 ASA grade I & II patients of both sexes, between 18-60 years of age, with BMI of < 30 kg/m2 scheduled for elective surgeries lasting for less than 2 h, were recruited in this study.
The exclusion criteria was: Patients with less than 2.5cm mouth opening, abnormality of neck or cervical spine disease, history of hoarseness, gastro-oesophageal reflux disease , active or a recent history of upper respiratory infection , obstructive sleep apnea and increased risk of aspiration.
We tested the hypothesis that these devices did not differ in insertion characteristics when used to achieve airway without use of muscle relaxant.
The primary objective of the study was to assess and compare LMAS and LTS with respect to insertion success rate. The secondary objectives were to also compare ease of insertion of the device, time taken for the insertion of the device, number of attempts required for securing the airway, leak pressure, ease of insertion of gastric tube, time taken for insertion of gastric tube and any post-operative laryngo-tracheal complications like post-operative sore throat, dysphagia, and hoarseness.
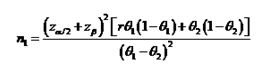
Sample size was calculated on the basis of the anticipated difference in success rate of insertion between the two devices, we used published data of success rate for insertion from a previous study2. In this study, the insertion success rate was 70% for LTS and 95% for LMA Supreme. Assuming the power of study 80% and significance level of 0.05, we calculated a sample size of 33 patients per group with a total of 66 patients using following formula
Although use of both LMAS and LTS is a standard practice in our hospital as an alternative to endotracheal intubation, the availability of these two devices depends on presence of department funds for purchase of these devices and the availability of ethylene oxide gas sterilization facility for LTS. Thus the allocation of a patient to a particular group depended on which device was available on the day of surgery. A convenience sampling method was therefore used to select and classify the patients depending upon which device was available for use. Group 1 had LMAS of appropriate size inserted and Group 2 had LTS of appropriate size inserted.
All patients were assessed the day before surgery, and the device to be inserted was explained to the patient All patients were investigated as per the institutional protocol with complete blood count, chest X-ray, random blood sugar and blood urea, serum creatinine, serum electrolyte, serum bilirubin liver enzymes and ECG in all patients above 40 years of age.
On the day of surgery, An appropriate sized SAD to be inserted was prepared. We used the appropriate size of airway device as per manufacturer’s recommendation. All insertions were made by an anesthesiologist with minimum two year experience and who had inserted each SAD at least 50 times. Only two attempts were allowed for insertion of the device. If there was failure to secure airway in two attempts, the patient was intubated with appropriate sized endotracheal tube. We also observed for any incidence of desaturation, coughing, bronchospasm or vomiting.
In the operating room the intravenous access was secured. Standard monitoring was with pulse oximeter, non-invasive blood pressure monitor, Cardioscope™ for ECG monitoring, capnometer and cuff pressure monitor.
The same standard balanced anesthesia technique and standard monitoring was used for both groups. All the SADs were inserted by the same qualified anesthesiologist without using a muscle relaxant. All patients were premedicated with IV glycopyrrolate 0.004 mg/kg, IV midazolam 0.03 mg/kg, IV ondansetron 0.08mg/kg and IV fentanyl 2 mcg/kg. After pre-oxygenation, anesthesia was induced with IV propofol 2.5-3 mg/kg. Adequate depth of anesthesia was confirmed when there was no motor response to jaw thrust.3
Patients were given the sniffing position to allow introduction of SADs. Semi sniffing position was given for insertion of LTS.
LMAS size 3 was used for small adult weighing 30-50KG, four for medium adult weighing 50-70 kg and five for large adult weighing 70-100 kg
LTS size 3 was used for small adult with height < 150 cm, 4 for medium adult with height of 155-180 cm 50-70 kg and 5 for large adult with height of > 180 cm
The efficacy of the device to achieve a secure airway was assessed by the following parameters.
Success rate at insertion was assessed as percentage of patients with successful insertion in first and second attempts.
Ease of insertion of the device was assessed by using a subjective scale4,5 of 1─4 [1-Very easy (no resistance), 2-Easy (mild resistance), 3-Difficult (moderate resistance), 4-Very difficult (inability to insert the device)]. Time taken for insertion of the selected device was counted as the time from the moment the face mask was removed until the first capnography upstroke on the capnometer after insertion of the device. Number of insertion attempts required to secure the airway was documented.
The leak pressure around the cuff was graded as follows: The intra-cuff pressure was measured using a hand held aneroid Portex manometer and the cuff pressure was maintained at 60 cmH2O. The air volume used to inflate the cuff was adjusted (either increased or decreased) to achieve the intra-cuff pressure of 60 cmH2O. The pressure limit of the anesthesia circuit was set to 40 cmH2O, the adjustable pressure limiting valve was closed and airway pressure was increased steadily with a continuous flow of oxygen (3 l/min). Leakage was defined as air escape audible with a stethoscope placed on the larynx, and leak pressure was defined as the airway pressure at which leakage was first detected. It was graded as 1- < 20 cmH2O, 2 as 20-30 cmH2O, 3 if > 30 cmH2O.
Ease of insertion of gastric tube was graded on 1-3 scale: 1- Easy, 2- Difficult, 3- Unable to pass.5 Time taken for insertion for gastric tube was counted from the start of the gastric tube insertion to the confirmatory insufflation of air into stomach heard on auscultation over epigastrium
The safety of the device was assessed by hemodynamic parameters (heart rate and mean arterial pressure) at baseline, at insertion, and in immediate post insertion period. Respiratory parameters i.e. oxygen saturation and end tidal carbon dioxide (EtCO2) were measured after insertion and throughout surgery. Any incidence of coughing, laryngospasm, desaturation and vomiting was also noted.
Incidence of postoperative complications was noted: Sore throat, dysphagia and hoarseness at one hour and 24 hours, grading of sore throat was done on a sore throat scale i.e. 0 – no sore throat, 1 – mild sore throat (complaint of sore throat only on asking), 2 – moderate sore throat (complaint of sore throat on his own), 3 – severe sore throat (associated with throat pain).
The patient was excluded from the study if number of attempts of insertion of the SAD was more than 2 or there was lack of square wave capnograph tracing on connection of circuit or inadequate tidal volume or excessive gastric insufflation and was considered as failed case. In these patients endotracheal tube was used to secure the airway.
RESULTS
A total of 66 patients were studied with 33 patients in each group. Analysis of results between the groups was done using Chi-square test and Fischer’s exact test. For statistical significance p value < 0.05 was considered to be statistical significant.
Both groups were comparable with regards to age, sex, weight, and ASA grade and baseline hemodynamic parameters with no statistically significant difference between the two groups (Table 1).
Table 1: Comparison of ASA grade, Demographic & Haemodynamic Parameters
| Variables | Group | Statistics | p-value | ||||
| Mean | SD | Median | IQR | Chi-Square | Fisher’s Exact | ||
| Age (yrs) | LTS | 35.82 | 10.46 | 34.00 | 17.50 | Unpaired t test | 0.169 |
| LMAS | 32.33 | 9.90 | 32.00 | 17.00 | Difference is not significant | ||
| Weight kg | LTS | 55.58 | 7.56 | 56.00 | 14.50 | Unpaired t test | 0.133 |
| LMAS | 52.88 | 6.81 | 52.00 | 11.00 | Difference is not significant | ||
| ASA Grade | LTS | ASA I: 20 | ASAII: 13 | 0.108 | 0.180 | ||
| LMAS | ASA I: 26 | ASA II: 7 | Difference is not significant | ||||
| Sex | LTS | 12 Females | 21 Males | 0.215 | 0.321 | ||
| LMAS | 17 Females | 16 Males | |||||
| Preop Pulse Rate | LTS | 77.52 | 12.71 | 76.00 | 21.00 | Unpaired t test | 0.247 |
| LMAS | 74.03 | 11.51 | 70.00 | 15.50 | Difference is not significant | ||
| Preop MAP | LTS | 76.30 | 12.58 | 7.81 | 78.00 | Unpaired t test | 0.466 |
| LMAS | 77.93 | 10.46 | 76.00 | 15.50 | Difference is not significant | ||
Comparison of Number of Attempts at Insertion and Insertion Success Rate: LTS was inserted in first attempt in 69.7% patients compared to 84.8% in LMAS group. This difference in the success rate at first attempt was statistically significant with a p value of 0.01.
Second attempt was required in 30.3% patients from LTS group compared to 15.2% patients from
LMAS group. The difference in the number of attempts was statistically insignificant with a p
Value of 0.142. The overall success rate was 100% in both groups.
Comparison of ease of insertion: In LTS group, the device was very easy to insert with no resistance in 42.4% patients, easy with mild resistance in 36.4% patients and difficult with moderate resistance in 21.2% patients.
In LMAS group the device was very easy to insert with no resistance in 69.7% patients, easy with mild resistance in 30.3% patients and difficult with moderate resistance in 0 % patients. This difference was statistically significant with a p value of 0.009.
Comparison of Leak Airway Pressure: In LTS group, the airway leak pressure was less than 20 cmH2O in 45.5% and 20-30 cmH2O in 54.5% patients. In LMAS group, the airway leak pressure was less than 20 cmH2O in 81.8% and 20-30 cmH2O in 18.2%. This difference was statistically significant with a p value of 0.002.
Comparison of Ease of RT insertion:
In LMAS group, RT was easy to pass in 87.9% patients and difficult in 12.1% patients. In LTS group, RT was easy to pass in 81.8% patients and difficult in 18.2% patients. The difference was statistically not significant with a p value of 0.492.
Comparison of Time for Effective Airway and Ryle’s Tube Insertion:
TFEA (time for effective airway- time from the moment the face mask was removed until the first capnography upstroke after insertion) and TFRT (time for RT- from the start of gastric tube insertion to confirmatory insufflation of air into stomach heard on auscultation over epigastrium) were monitored. Mean time for airway device insertion was 24.06 ± 2.54 sec and 20.39 ± 2.19 sec in LTS and LMAS groups respectively while time for RT insertion was 18.70 ± 2.40 sec and 17.27 ± 2.30 sec in LTS and LMAS group respectively. The difference in both these parameters was statistically significant with p value of 0.000 for TFEA and 0.017 for TFRT.
Comparison of Post-operative Sore Throat at One Hour:
Sore throat at 1 hour – No sore throat was noted in 93.9% cases in LMAS and 69.7% in LTS group. Mild sore throat was noted in only 6.1% cases in LMAS and in 24.2% cases in LTS group. Moderate sore throat was noted in 0% cases in LMAS and 6.1% cases in LTS group. Thus 28.3% patients from LTS group had some degree of sore throat while only 6.1% patients had sore throat in LMAS group. Severe sore throat was not found in any of the patients from either group. This difference in the incidence of mild sore throat at 1 hour (24% for LTS and 6% for LMAS) was found to be statistically significant using Pearson Chi – Square test (P=0.034).
Comparison of Post-Operative Sore Throat at 24 Hour:
No sore throat was present in 97% cases in LMAS and 87.9% in LTS group while mild sore throat was present in 3% case in LMAS and in 12.1% in LTS group. Moderate and severe sore throat was not found in any cases 24 hour after surgery in either of the group. This difference was not found to be statistically significant with a p value of 0.163 using Pearson Chi – Square test.
Comparison of Post-Operative Dysphagia:
We evaluated and graded dysphagia as nil, mild and severe 2. Dysphagia was not noted in any patient in LMAS group while mild dysphagia was noted in 5 patients (15.2%) in LTS group and this difference was found to be statistically significant (p=0.02). Hoarseness was present in one patient in each group (3%) and it was statistically insignificant (p=1.000).
Heart rate, MAP, SPO2 and ETCO2 was noted and compared at following times in both groups: preoperative, pre-induction, at insertion, 5, 10, and 15 min after insertion. No statistical significant difference was observed between the two groups at any time with a p value of > 0.05 for all outcomes at all periods.
DISCUSSION
SADs have become popular in airway management as a missing link between the facemask and the endotracheal tube in terms of both anatomical position and degree of invasiveness. These devices are often the first to be used in securing airway in emergency situations and in difficult to ventilate and intubate patients, both in-hospital and out-of-hospital1. Their less invasive nature and the ability to introduce them without muscle relaxation makes them an attractive option to secure airway in short duration and day care surgeries as the recovery if faster.2-5
This prospective cohort study compared Supreme LMA and LTS with respect to the insertion characteristics and achievement of a secure airway. In this study the airway could be secured in all patients with in two attempts and the overall insertion success rate was 100%. The insertion success rate at first attempt was statistically and clinically higher with LMAS. However the difference in the number attempts was not statistically significant.
In a randomized study, Russo et al compared I gel, LMAS and LTS in 120 patients. The first time insertion success rate was 72% in LMAS and 53% in LTS2. Beleña, et al studied the efficacy of Supreme LMA in 140 female patients undergoing gynecological laparoscopic surgeries. In 123 patients, insertion was successful in the first attempt (87.8%), in 16 patients in the second attempt (11.4%), and in one patient in the third attempt (0.7%).6 Cook, et al evaluated LMAS in 100 non-paralyzed patients in terms of insertion characteristics.7 In 90% patients it was successful in the first attempt and in 10% of patients in second attempt.
All the above mentioned studies indicate that the success rate at first insertion attempt with LMAS is clinically higher. Results from our study also show that LMAS has higher insertion success rate at first attempt as compared to LTS.
Henlin et al8 found LMAS very easy to insert in 61.4% patients, easy to insert in 30.7% patients and difficult to insert in none of the patients. In LTS group, it was very easy in only 16.3% patients, easy in 43.9% patients, and difficult in 13.3% patients. The results of our study are similar to the results of these investigators.
Leak airway pressure was determined as a function of cuff pressure for the SAD with inflatable cuffs (LMAS and the LTS). A higher oropharyngeal leak pressure is an indicator of efficacy and safety of cuff seal when using SADs. Our study showed that LTS had better sealing pressure and has better efficacy of the seal and fit with the anatomy of supraglottic region.
Henlin et al also showed that airway leak pressure was higher in the LTS which was statistically significant.8
Ease of insertion of a drainage tube is an indicator of proper positioning of an SAD. Ryle’s tube can be inserted with ease only if the SAD sits on the tip of upper esophagus in case LMAS and if the esophageal cuff is properly positioned in the upper esophagus in case of LTS. In our study, the RT insertion was faster through LMAS
The time required for achieving the effective airway (TFEA) showed that it took longer to achieve secure airway with LTS as compared to LMAS. Russo et al found insertion time in LMAS group as 11 ± 9 sec and 14 ± 10 sec in LTS group (p = 0.173) which was statistically insignificant2. However this study does not mention the criteria chosen for measuring the time interval as well as who did the insertions. Thus it is difficult to compare our results with the results of this study.
Henlin et al8, defined insertion time as the time from SAD preparation (removal of SAD from the package, lubrication etc.) to confirmation of effective ventilation with a visible ETCO2 tracking on the monitor. The study found the average insertion time for LMAS group as 70.4 ± 32.5 sec and for LTS group was 107.3 ± 67.9 sec respectively and this difference was statistically significant. Our study too found that it takes longer to achieve effective airway with LTS as compared to LMAS. Thus LMAS is better than LTS with respect to Time needed to secure effective airway.
Cook et al7 found median insertion time of LMAS to be 18 ± 8 sec3which is similar to the time taken for successful LMAS insertion from our study.
Thus LMAS is easier to insert, takes shorter time for securing airway and requires fewer attempts at successful insertion than LTS. As LMAS is preformed to closely mimic the anatomy of the upper airway it has more success rate even in the hands of inexperienced anesthesiologist.
A statistically higher incidence of sore throat was found at one hour with LTS in the immediate postoperative period (p=0.034). This could be attributed to higher leak pressure in LTS group as compared to LMAS group. The leak pressure is an important factor which predicts postoperative airway morbidity. Incidence and severity of postoperative sore throat is known to be markedly reduced with lower cuff pressure and leak pressures.
A statistically higher incidence of mild dysphagia was noted in LTS group. There was no difference in the incidence of hoarseness between the two groups. This shows that LTS leads to higher incidence of post-operative airway morbidity as compared to LMAS.
The hemodynamic parameters such as pulse rate and mean arterial pressure and SpO2 as well as EtCO2 were compared and no statistical significant difference was observed between the two groups during the entire observation period with respect to these parameters.
Gupta et al compared I-gel and supreme LMA, and observed no significant difference in mean heart rate (beat/min) and arterial pressure (mmHg) between the 2 groups (p-value > 0.05).9
Dahaba et al also assessed the hemodynamic response to insertion of Proseal laryngeal mask airway (PLMA) and LTS in 60 patients4 and concluded that the LTS produces a greater and more sustained hemodynamic response than does the PLMA (p < 0.005). In our study we did not find any statistically or clinically significant difference in the hemodynamic parameters in both the groups.
LIMITATIONS
The nature of the study did not allow blinding regarding the airway inserted; this could have led to researcher bias. We also did not use a fibreoptic bronchoscope to visualize the larynx. We do not routinely do a fibreoptic bronchoscopy as it is a time consuming procedure and it reduces the patient turnover in our department dealing with heavy patient load.
CONCLUSION
In this study we found that both LMAS and LTS are easy and effective alternatives to endotracheal intubation. Both the SADs secured effective airway in less than 30 seconds.
The insertion success rate at first attempt was higher with and LMAS was easier to insert as compared to LTS. Time for effective airway was shorter with the use of LMAS. The time for Ryle’s tube insertion was also shorter through LMAS suggesting better anatomical positioning LTS was associated with higher leak pressure and a higher incidence of laryngo-tracheal complications.
Conflict of Interest: None declared by the authors
Author Contributions:
SC-Conduction of study
CND-concept and manuscript editing
REFERENCES
- Ramaiah R., Das D., Bhananker SM, Joffe A.M. Extraglottic airway devices: A review. Int J of Critical illness and Injury science, Jan- March 2014; 4(1):77-87. doi: 10.4103/2229-5151.128019. [PubMed] [Free full text]
- Russo SG, Cremer S, Galli T, Eich C, Bräuer A, Crozier TA, et al. Randomized comparison of the I-gel, the LMASupreme, and the Laryngeal Tube Suction-D using clinical and fiberoptic assessments in elective patients. BMC Anesthesiology 2012, 12(18) :2-9. [Free full text]
- Drage MP, Nunez J, Vaughan RS, Asai T. Jaw thrusting as a clinical test to assess the adequate depth of anaesthesia for insertion of the laryngeal mask. Anaesthesia, 1997;51 (12): 1167-70. [PubMed] [Free full text]
- Dahaba AA, Prax N, Gaube W, Gries M, Rehak PH, Metzler H. Haemodynamic and catecholamine stress responses to the Laryngeal Tube-Suction Airway and the Proseal Laryngeal Mask Airway. Anaesthesia, April 2006, 61(4): 330–334. [PubMed] [Free full text]
- Richez B, Saltel L, Banchereau F, Torrielli R, Cros AM. A new single use supraglottic airway device with a noninflatable cuff and an esophageal vent: an observational study of the i-gel. Anesth Analg 2008; vol 106:1137-9. doi: 10.1213/ane.0b013e318164f062. [PubMed]
- Beleña JM, Núñez M, Gracia JL, Pérez JL, & Yuste J. The Laryngeal Mask Airway Supreme: safety and efficacy during gynaecological laparoscopic surgery. SAJAA. 2012; 18(3): 143-147. [Free full text]
- Cook TM, Gatward JJ, Handel J, Hardy R, Thompson C, Srivastava R, Clarke PA. Evaluation of the LMA Supreme in 100 non-paralysed patients. Anesthesia, May 2009; 64 (5) :555-62. doi: 10.1111/j.1365-2044.2008.05824.x. [PubMed] [Free full text]
- Tomas H, Sotak M, Kovaricek P, Tyll T, Balcarek L, Michalek P. Comparison of Five 2nd-Generation Supraglottic Airway Devices for Airway Management Performed by Novice Military Operators, BioMed Res Int. 2015;201898. [Free full text]
- Gupta V, Mehta N, Gupta S, Mahotra K. Comparative evaluation of supraglottic airway devices I-gel and Supreme LMA in patients undergoing surgery under general anesthesia. Ind J Clin Anaesth. 2015;2(2):86-91. [Free full text]

