AKM Akhtaruzzaman*, Md. Wahidur Rahman**, D. K. Bhowmick***, M. F. A. Begum****
Akhtaruzzaman AKM, Rahman MW, Bhowmick DK, Begum MFA.
*Professor of Neuroanesthesia, ***Assistant Professor
Department of Anesthesia, Pain & Intensive Care Medicine, Bangabandhu Sheikh Mujib Medical University,Shahbag, Dhaka-1000 (Bangladesh)
**PG Trainee DA, ****Assistant Professor, Obstetrics & Gynecology
Sir Salimullah Medical College & Mitford Hospital, Dhaka (Bangladesh), drwahidur@gmail.com
Correspondence: AKM Akhtaruzzaman, Professor of Neuroanesthesia, Department of Anesthesia, Pain and Intensive Care Medicine, Bangabandhu Sheikh Mujib Medical University, Shahbag, Dhaka-1000 (Bangladesh); E-mail: mili@bol-online.com; Phone: 880181922019
ABSTRACT
Peripheral nerve lesions are a complication of operative procedures under both general and regional anesthesia. The study incorporates a case of twenty eight year old woman who developed left foot drop after removal of a McDonald cervical suture followed by Caesarean section under subarachnoid block (SAB). Intra-operatively, she was put in lithotomy position for removal of the McDonald cervical suture. Her neurological deficit gradually recovered over the next ten months. We suggest that intra-operative positioning for cervical suture removal may have caused this injury.
Key words: Foot drop; Lithotomy position; Operative positioning
Citation: Akhtaruzzaman AKM, Rahman MW, Bhowmick DK, Begum MFA. Foot drop after subarachnoid block for removal of McDonald cervical suture and Cesarean section. Anaesth Pain & Intensive care 2014;18(1):52-55
INTRODUCTION
Subarachnoid block (SAB) is a very popular obstetric anesthetic modality with a reasonable safety margin. Serious neurologic complications directly attributable to neuraxial anesthesia are rare. In a 2-year prospective study Scott and Tunstall found eight neurological deficits in 14856 obstetric spinal blocks (5.4 in 10 000).1 All their cases were reversible neuropathies. In a more recent survey of 71,053 regional anesthetic procedures performed in France, there were 24 neurological injuries following SAB with an incidence of 6 in 10,000 and 6 following epidural block with an incidence of 2 in 10,000.2 Neurological deficits are often associated with childbirth. Postpartum foot drop was first described in 1838.3 Obstetric palsies are estimated to be three to four times more common than deficits caused by regional anesthesia.4,5 The first step during clinical evaluation of such neurological deficit should exclude a spinal cord, nerve root or other central nervous system pathology and examine for peripheral nervous system involvement. Although history and examination may indicate the site of injury, but differentiation between peripheral and central causes requires sophisticated investigations like nerve conduction studies and magnetic resonance imaging. The study describes a case of foot drop with sensory loss that occurred in a woman who underwent removal of a McDonald cervical suture and Caesarean section under SAB.
CASE REPORT
A 28-year-old G6P1 lady at 37 weeks of gestation was scheduled for an elective lower segment Caesarean section (LSCS). She previously had multiple miscarriages and, because of this, a McDonald cervical suture had been inserted during the thirteenth week of gestation. The patient had remained mostly bed-bound during the late stages of her pregnancy because of the risk of miscarriage.
The woman was otherwise well with no significant drug history or pre-existing neurological disorder. In particular, there was no history of previous lower extremity pain, back pain, numbness or weakness. Her height was 150 cm and she weighed 54 kg. Preoperative laboratory findings, including coagulation studies, were normal.
In the operating room, using a 25-gauge Quincke type spinal needle with the patient in sitting position, lumbar puncture was performed at the L3-L4 interspace using the midline approach. Free flow of clear CSF was obtained on the second attempt. During insertion of the needle, the patient did not complain of any paresthesiae. A total volume of 2.5 ml consisting of 10 mg of 0.5% hyperbaric bupivacaine with 25 µg of fentanyl was administered. While administering the drug the needle bevel was kept cephalad.
After confirmation of reasonable sensory and motor block, surgery was commenced. At first the lady was put in the lithotomy position for removal of McDonald cervical suture, which took one hour. Later she was put in the supine position and LSCS was performed which lasted 40 minutes. There were no intraoperative anesthetic problems and there was no significant intraoperative hypotension.
Figure 1: Left foot drop
Postoperatively, after approximately five hours, she noticed difficulty in moving her left leg with loss of sensation over the antero-lateral aspect of the same limb. The right lower limb was normal.
On examination, there was an obvious left-sided foot drop. Sensory examination revealed a loss of non-discriminative sensation (pain, light touch and temperature) over the left L5, S1 territory. There was also reduced vibration perception (tested with a 128 Hz tuning fork over the left lateral malleolus) and reduced joint position sense (tested on the left big toe). Motor examination revealed a complete loss of ankle dorsiflexion and plantar flexion (0/5) on the left side. While the left ankle jerk was normal.
The patient was referred to a neurologist who started her on oral prednisolone (1mg/kg) and oral vitamin-B1, B2, B6 complex. Regular neurological examination was performed to observe for any progressive weakness: however the patient’s neurological symptoms and signs remained static. On the following day, magnetic resonance imaging was performed, which showed a rounded focal T1W iso- to hyper and T2W hyper intense area in T12 vertebrae, but the scan was otherwise unremarkable with no evidence of a hematoma.
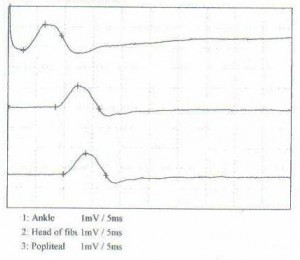
On the twelfth post-operative day, the patient was discharged with an ankle foot splint and physiotherapy advice. She was followed up after one month and a nerve conduction study and electromyograph (EMG) were performed. These showed electrophysiological findings consistent with a left peroneal neuropathy (below knee, axonal injury), affecting both superficial and deep peroneal branches. There were signs of early reinnervation. On examination, there was some improvement in motor power (3/5 ankle dorsiflexion). The patient was advised to continue with the physiotherapy.
Figure 2: Motor conduction study: left peroneal nerve
On follow-up after ten months she was found to have undergone a complete recovery with no residual neurological deficit.
DISCUSSION
Neurological complications like paraesthesia, cauda equina syndrome and paraplegia following SAB are rare but have been reported in the literature.6-10 Causes include direct needle injury, local anesthetic drug toxicity and management-related factors.6-9 Direct trauma by spinal needle injury is usually related to multiple attempts resulting in spinal cord or nerve root injuries.8 Kane reported that haematomata secondary to needle trauma can lead to spinal cord compression and paraplegia.7 In this case, based on the preoperative laboratory examination, the patient did not have haemostatic abnormalities. Postoperatively the MRI scan did not show any lesions, such as haematoma in the lumbar region. Local anesthetic drugs can directly irritate nerve roots by osmotic effects.11
The most important management-related factor is hypotension, which can induce spinal cord ischemia and thrombosis of the spinal arteries.8 In our patient there was no recorded event of significant hypotension.
Figure 3: Leg holders used in this particular patient
Anaesthetized patients undergoing surgical procedures in lithotomy position are prone to develop lower extremity nerve injury. A 1994 retrospective review of the rate and type of motor neuropathies that occurred in 198,461 consecutive patients who underwent procedures while they were in a lithotomy position found the most commonly involved nerves were the common peroneal (81%), sciatic (15%) and femoral (4%).12 The common peroneal nerve is particularly vulnerable to injury due to its superficial course along the head of the fibula. The most common mechanism of peroneal nerve injury is external compression classically from pressure exerted by inappropriate leg positioning in stirrups.13 If a patient develops a postoperative neurological deficit it is important to investigate the deficit properly to define the nature of injury and to seek the possible etiology. Immediate magnetic resonance imaging is the current gold standard to rule out central lesions. The clinical diagnosis of foot drop is less reliable and neurophysiological evaluation would have been useful to identify a peripheral lesion.14 Electrophysiological studies are useful to determine the level and type (axonal, demyelinating) of injury. The timing of electrophysiology studies is important for obtaining an accurate diagnosis. It is best to perform nerve conduction studies 10–14 days after the injury to obtain an informative result.15
The rate and extent of recovery from such neurological injury can be variable. Auroy et al. prospectively monitored neurologic complications in more than 103,000 regional anesthesia cases. All deficits were present within 48 hours after anesthesia. Most were transient with recovery occurring between two days and three months.2 Axonal damage tends to resolve more slowly and often causes permanent impairment of nerve function.16 In our patient, who had an axonal lesion , a complete recovery occurred within ten months of the incident.
CONCLUSION
During childbirth, serious neurological complications directly attributable to SAB or epidural anesthesia are rare. Peripheral nerve injuries can occur as a result of malpositioning of the patient on the operating table with consequent stretching and/or compression of nerves.
If a patient is scheduled to undergo surgery by SAB, careful enquiries should be made about any neurological symptoms or signs and a detailed examination must be carried out if necessary with proper documentation. If a patient shows a persistent neurological deficit post-operatively, a careful neurologic exam should be performed and a MRI scan should be done within hours. Neurophysiological investigations (nerve conduction studies and EMG) can often provide useful diagnostic and prognostic information. Preventive measures should be taken by acknowledging all the contributing factors which can lead to a neurological injury. Meticulous care should be taken to position an anaesthetized patient before proceeding to surgery and the anaesthetist should check the positioning and pressure points. To avoid such injury it is essential to understand the general principles of operative positioning, have sufficient personnel for positioning, and the use of proper padded devices.
Acknowledgement: We are highly grateful to Dr Wayne Morriss, Chair, Education Committee – WFSA for his continuous encouragement and correction of the manuscript before submission.
REFERENCES
- Scott DB, Tunstall ME. Serious complications associated with epidural/spinal blockade in obstetrics: a two-year prospective study. Int J Obstet Anesth 1995;4:133–9.[PubMed]
- Auroy Y, Narchi P, Messiah A, Litt L, Rouvier B, Samii K. Serious complications related to regional anesthesia: results of a prospective survey in France. Anesthesiology 1997;87:479-86. [PubMed] [Free Full Text]
- Beatty TE. Second report of the new Lying-in-Hospital, Dublin. Dublin J Med Sci 1838;12:273-313.
- Donaldson J O. Neuropathy. In: Donaldson J O. Neurology of pregnancy (2nd edition). Philadelphia: WB Saunders. 1989:23-59
- Loo CC, Dahlgren G, Irestedt L. Neurological complications in obstetric regional anesthesia. Int J Obstet Anesth 2000;9:99-124. [PubMed]
- 6. Faccenda KA, Finucane BT. Complications of regional anesthesia. Drug Saf 2001;24:413-42. [PubMed]
- Horlocker TT. Complications of spinal and epidural anesthesia. Anesthesiol Clin North America 2000;18:461-85. [PubMed]
- Kane RE. Neurologic deficits following epidural or spinal anesthesia. Anesth Analg 1981;60:150-61. [PubMed]
- Nicholson MJ, Everson UH. Neurologic complications of spinal anesthesia. J Am Med Assoc 1946;132:679-85. [PubMed]
- Seigne TD. Aseptic meningitis following spinal analgesia. Anesthesia 1970;25:402-7. [PubMed]
- Noble AB, Murray JG. A review of the complications of spinal anesthesia with experience in Canadian teaching hospitals from 1959 to1969. Can Anaesth Soc J 1971;18:5-17. [PubMed]
- Warner MA, Martin JT, Schroeder DR, Offord KP, Chute CG. Lower-extremity motor neuropathy associated with surgery performed on patients in a lithotomy position. Anesthesiology 1994;81:6-12. [PubMed] [Free Full Text]
- Wilbourne AJ. Iatrogenic nerve injuries. Neurol Clin 1998;16:55–82. [PubMed]
- Tsen LC. Lower extremity neurologic complications of labor, delivery and central neural analgesia and anesthesia. Problems in Anesthesia 1999;11:344-358.
- Parry GJ. Electrodiagnostic studies in the evaluation of peripheral nerve and brachial plexus injuries. Neurol Clin 1992;10:921-34. [PubMed]
- Katirji B, Wilbourn AJ, Scarberry SL, Preston DC. Intrapartum maternal lumbosacral plexopathy. Muscle Nerve 2002;26:340-7. [PubMed]