Tomoki Nishiyama, MD, PhD
Department of Anesthesiology, Harada Hospital, 1-13-3, Toyooka, Iruma, Saitama, 358-0003, Japan
Correspondence: Tomoki Nishiyama, MD, PhD, Department of Anesthesiology, Harada Hospital, 1-13-3, Toyooka, Iruma, Saitama, 358-0003, (Japan); Tel: +81-4-2962-1251; E-mail: nishit-tky@umin.ac.jp
ABSTRACT
Objective: In bariatric surgery, arterial carbon dioxide (PaCO2) and oxygen (PaO2) pressures are important but sometimes difficult to measure. The purpose of the present study was to investigate whether transcutaneous carbon dioxide (tcPCO2) and oxygen (tcPO2) pressures can be used to monitor PaCO2 and PaO2, respectively, in laparoscopic bariatric surgery.
Methodology: This non-blind, comparadive study was conducted at operating room in the city hospital. Ten adult obese (Body Mass Index (BMI) > 35) patients for laparoscopic bariatric surgery (Bariatric group), and 10 normal weight (BMI < 30) adult patients for open gastric surgery (Control group) were studied.
After an epidural catheter insertion at T6-7 or T 7-8, anesthesia was induced with midazolam, propofol, fentanyl, and vecuronium, and was maintained with continuous propofol and remifentanil, intermittent vecuronium and epidural lidocaine. After anesthesia induction, a radial artery catheter was inserted. The electrode of transcutaneous monitor was put on the chest ipsilateral to a radial artery catheter. Pressure controlled ventilation was used in both groups.
During surgery at four random points in each patient samples were drawn for arterial blood gas analysis, and measurements of end-tidal carbon dioxide (EtCO2), tcPO2 and tcPCO2 were performed.
Results: TcPCO2 and PaCO2 in the control group had good correlation, while no correlation was found in the bariatric group. TcPO2 and PaO2, tcPCO2 and EtCO2, and PaCO2 and EtCO2 had no correlation in both groups. The bias and limits of agreement of tcPCO2 – PaCO2, tcPO2 – PaO2, EtCO2 – tcPCO2, and PaCO2 – EtCO2 were larger in the bariatric group than the control group.
Conclusion: Our study concludes that TcPO2 and tcPCO2 cannot be surrogate measurements of PaO2 and PaCO2, respectively in laparoscopic bariatric surgery.
Key words: Obesity; Bariatrics; Bariatric surgery; Laparoscopic surgery; Blood Gas Analysis; Blood Gas Monitoring, Transcutaneous; Oximetry, Transcutaneous; Oxygen Partial Pressure Determination, Transcutaneous; Carbon Dioxide Partial Pressure Determination, Transcutaneous
Citation: Nishiyama T. Can transcutaneous carbon dioxide and oxygen pressure predict arterial carbon dioxide and oxygen pressure during laparoscopic bariatric surgery? Anaesth Pain & Intensive Care 2016;20(2):131-136
Received: 01 January 2016; Reviewed: 6 April 2016; Corrected: 7, 12 April 2016; Accepted: 01 May 2016
INTRODUCTION
The frequency of bariatric surgery is increasing with the ever-increasing number of morbidly obese patients. Laparoscopic procedures are preferred to decrease respiratory depression by postsurgical pain and to get good surgical field.1 In mechanically ventilated morbidly obese patients, functional residual volume decreases and closing capacity becomes high, which leads to a ventilation perfusion mismatch and increased intrapulmonary shunt.2 Therefore, monitoring of arterial oxygen (PaO2) and carbon dioxide (PaCO2) pressures is quite important during general anesthesia. However, in morbidly obese patients, inserting arterial catheter is sometimes difficult and PaO2 and PaCO2 could not be measured continuously. End-tidal CO2 (EtCO2) and percutaneous oxygen saturation (SpO2) are now usually used to monitor CO2 and O2, respectively, during general anesthesia. SpO2 is sometimes difficult to measure in morbidly obese patients due to thick skin. In morbidly obese patients, reduced functional residual volume with ventilation perfusion mismatch makes EtCO2 incorrect measurement of PaCO2.3
Transcutaneous O2 (tcPO2) and CO2 (tcPCO2) pressures are less invasively monitored. There are some studies to investigate whether tcPCO2 could be used as a surrogate measure of PaCO2 in surgery of morbidly obese patients.4,5 In addition, tcPCO2 has been shown to be more accurate to predict PaCO2 than EtCO2 in laparoscopic surgery.6,7 However, there is no study of tcPO2 in surgery of obese patients. Only our previous study8 investigated tcPO2 in laparoscopic surgery. In that study, tcPO2 had not always good correlation with PaO2.
The purpose of the present study was to investigate whether tcPCO2 and tcPO2 can be used to monitor PaCO2 and PaO2, respectively, in laparoscopic bariatric surgery.
METHODOLOGY
After the approval of the ethics committee of the hospital and informed consent from each patient, 10 adult obese (Body Mass Index (BMI) > 35) patients for laparoscopic bariatric surgery (Bariatric group), and 10 normal weight (BMI < 30) adult patients for open gastric surgery (Control group) were enrolled in this study. Those who had severe cardiac, pulmonary, vascular, renal, or liver disease, or who had drug abuse or smoking habit were excluded.
Premedication was not given. An epidural catheter was inserted at T6-7 or T7-8. It was performed using ultrasound guidance in the bariatric group. Anesthesia was induced with midazolam, propofol, and fentanyl. Oro-tracheal intubation was facilitated with vecuronium. Anesthesia was maintained with continuous propofol and remifentanil, and intermittent administration of vecuronium and epidural lidocaine. After anesthesia induction, a radial artery catheter was inserted into right radial artery to perform blood gas analysis. Pressure controlled ventilation was used in both groups basically to keep normal tidal volume as calculated by ideal body weight starting at 10 breaths per minute with 100% oxygen. Then respiratory rate and inspiratory pressure were changed for the study.
The electrode of TCM4TM (Radiometer, Copenhagen, Denmark) heated at 43 degrees Celsius was put on the chest ipsilateral to a radial artery catheter. At four random points during surgery in each patient, samples were drawn for arterial blood gas analysis, then measurements of end-tidal carbon dioxide pressure (EtCO2), percutaneous oxygen (tcPO2) and carbon dioxide (tcPCO2) pressure were noted.
Power analysis was performed to detect R2 value of 0.75 with the power of 0.95 (G PowerTM software, University Mannheim, Germany). Statistical analysis was performed with chi-square test and factorial analysis of variance for demographic data. A p-value less than 0.05 was considered to be significant difference. To judge the accuracy of tcPCO2 and tcPO2, the Bland-Altman plot and linear regression analysis were performed.
RESULTS
The power analysis showed that 10 patients were necessary to detect R2 of 0.75. Therefore, we included 10 patients in each group. Demographic data were not different between the two groups except for body mass index (Table 1).
Table 1: Demographic data
| Parameter | Obese Group | Control Group |
| Male/Female | 4/6 | 5/5 |
| Age (years) | 39.2 (21-60) | 44.8 (25-62) |
| Height (cm) | 169.1 (153.0-181.0) | 167.8 (158.9-174.0) |
| Body weight (kg) | 144.4 (102.3-206.0)* | 65.5 (55.5-72.0) |
| Body mass index (kg/m2) | 50.8 (40.3-82.5)* | 23.2 (22.0-24.1) |
| Duration of anesthesia (min) | 285 (165-385) | 262 (155-375) |
Data given as number of the patients or mean with range in the parenthesis.
*: P < 0.05 vs. Control group
TcPCO2 and PaCO2 in the control group had good correlation (Figure1-1), while no correlation was found between tcPCO2 and PaCO2 in the bariatric group (Table 2, Figure 1-2). TcPO2 and PaO2 (Figure 3), tcPCO2 and EtCO2, and PaCO2 and EtCO2 had no correlation in both groups (Table 2), while coefficient of determination (R2) of these were higher in the control group than the bariatric group.
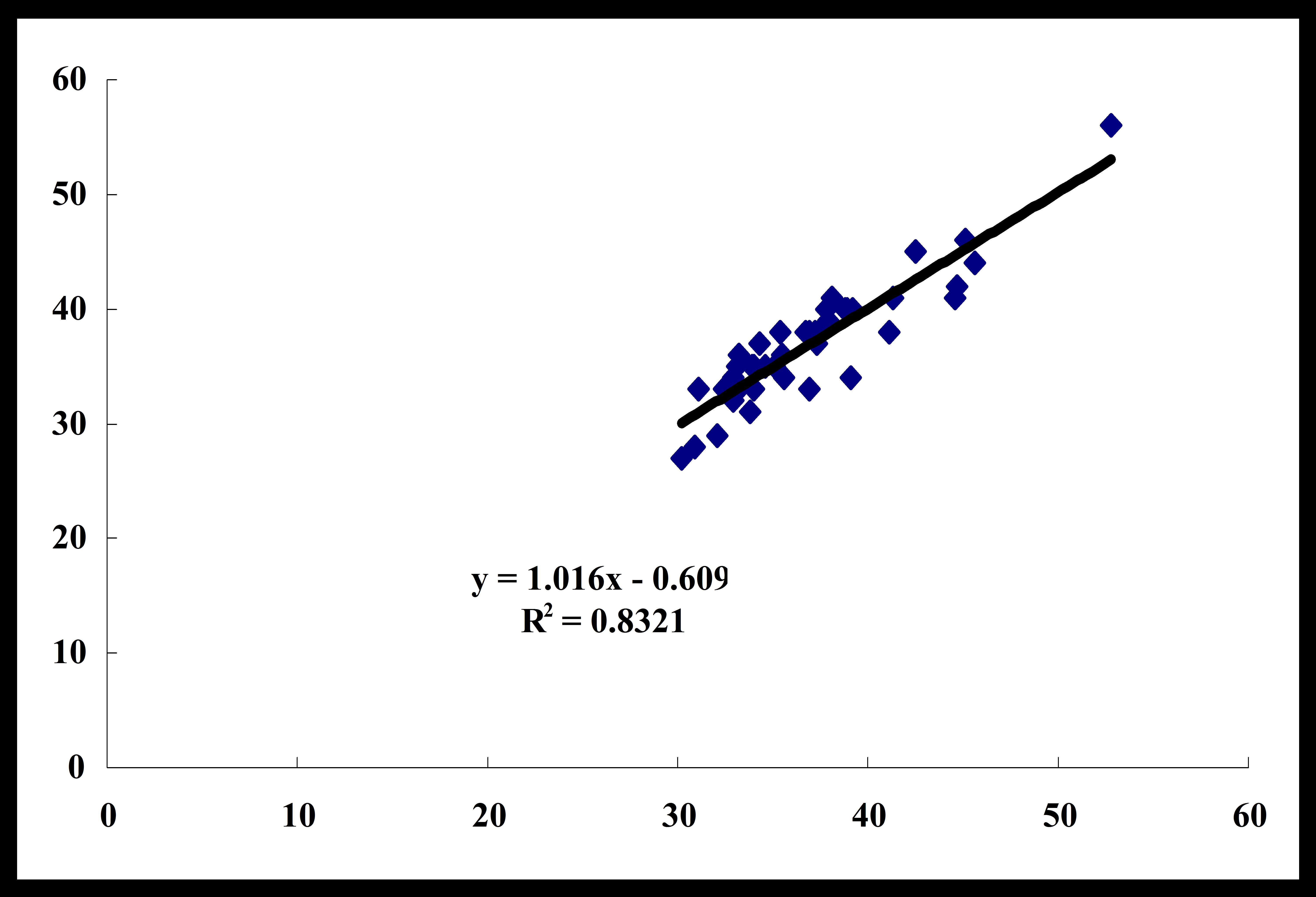
Figure1-1: Correlation between tcPCO2 and PaCO2 – Control group
Positive correlation was found.
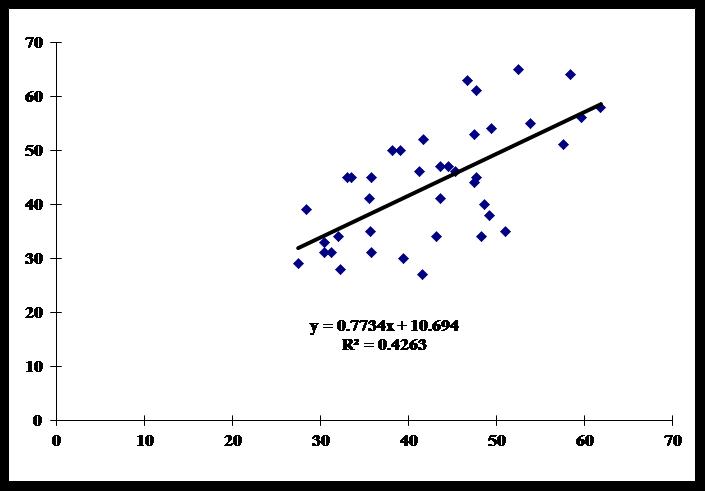
Figure1-2: Correlation between tcPCO2 and PaCO2 – Bariatric group
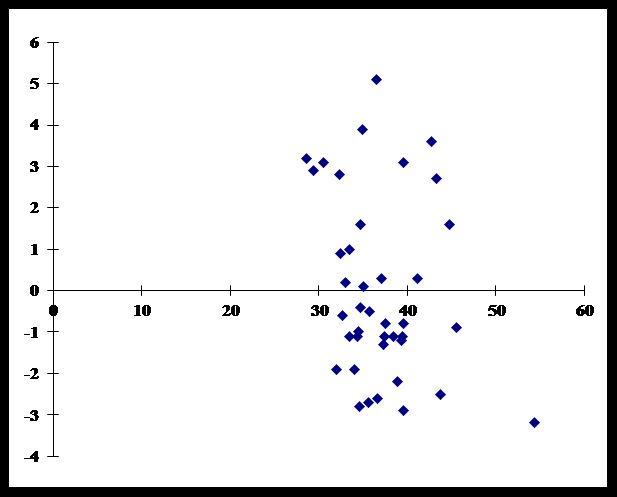
Figure 2-1: Bland-Altman plot of tcPCO2 and PaCO2 – Control group
Low bias and good limits of agreement were found.
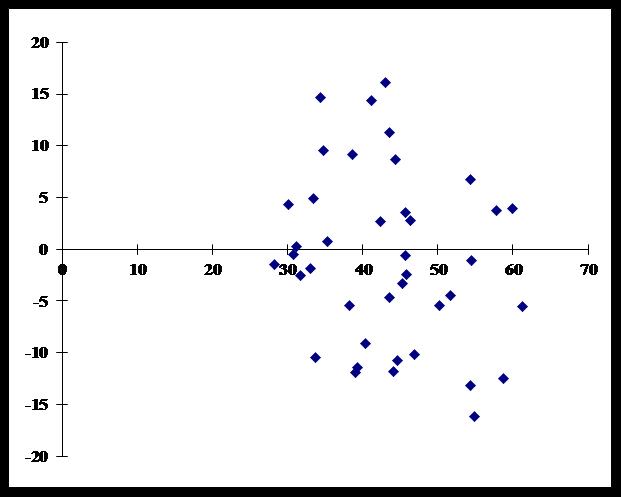
Figure 2-2: Bland-Altman plot of tcPCO2 and PaCO2 – Bariatric group
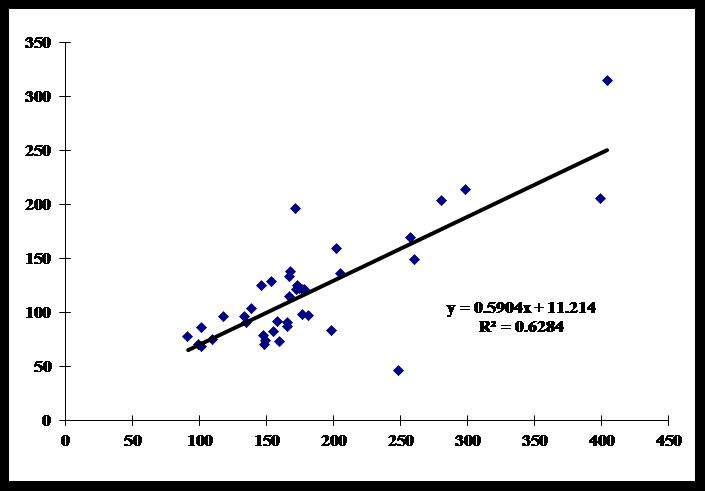
Figure 3-1: Correlation between tcPO2 and PaO2 – Control group
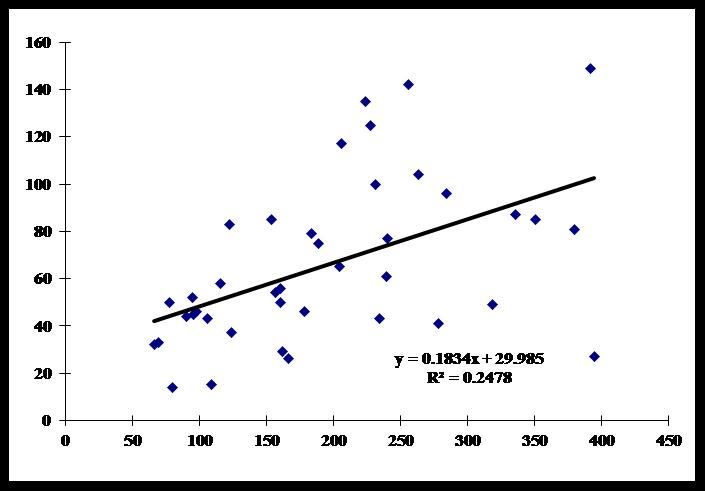
Figure 3-2: Correlation between tcPO2 and PaO2 – Bariatric group
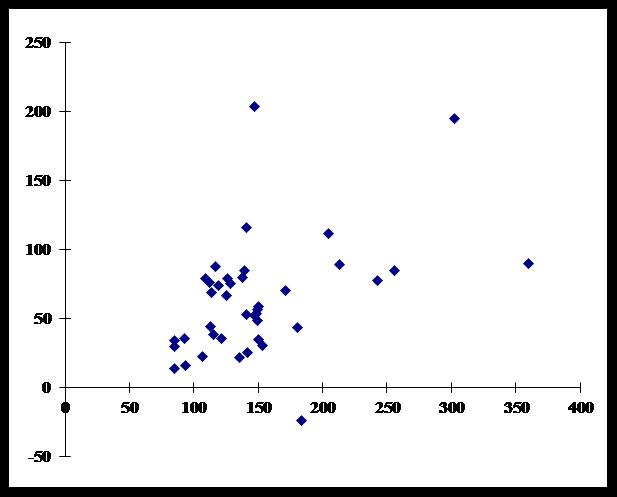
Figure 4-1: Bland-Altman plot of tcPO2 and PaO2 – Control group
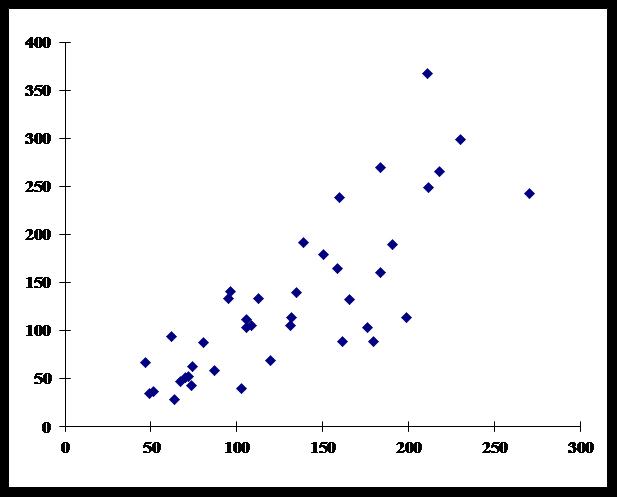
Figure 4-2: Bland-Altman plot of tcPO2 and PaO2 – Bariatric group
The bias and limits of agreement were small enough to be surrogate measurement for tcPCO2 and PaCO2 in the control group (Figure 2-1). The bias and limits of agreement of tcPCO2 – PaCO2, tcPO2 – PaO2, EtCO2-tcPCO2, and PaCO2-EtCO2 were larger in the bariatric group than the control group (Table 2, Figure 2-2, 4-1, 4-2).
Table 2: Correlation coefficient, bias, and limits of agreement
| R2 | Bias | Limits of agreement | |
| Control | |||
| PaO2-tcPO2 | 0.63 | 67.6 | -6.1, 141.4 |
| PaCO2-tcPCO2 | 0.83 | -0.95 | -4.3, 2.5 |
| EtCO2-tcPCO2 | 0.48 | -5.1 | -11.9, 1.6 |
| PaCO2-EtCO2 | 0.66 | 4.2 | -1.6, 10.0 |
| Bariatric | |||
| PaO2-tcPO2 | 0.25 | 147.4 | -31.2, 326.1 |
| PaCO2-tcPCO2 | 0.43 | -2.2 | -18.7, 14.3 |
| EtCO2-tcPCO2 | 0.27 | -10.5 | -24.3, 3.2 |
| PaCO2-EtCO2 | 0.31 | 8.3 | -3.6, 20.3 |
DISCUSSION
The present study showed that tcPO2 and tcPCO2 had no correlation and had large bias and limits of agreement with PaO2 and PaCO2, respectively in laparoscopic bariatric surgery.
For measurement of tcPCO2, chest probe was proved to be better than ear probe to get good correlation with PaCO2.2 When the electrode of the TCM was put on the chest, tcPO2 and tcPCO2 well correlated with PaO2 and PaCO2, respectively in our previous study.10 Therefore, we used chest probe. The electrode of the TCM should be heated to 43º C to measure tcPO2 and tcPCO211 as we did in the present study.
There are some limitations of this study. We used pressure controlled ventilation in both groups, while the pressure settings were quite variable. In some cases, ephedrine was administered to increase blood pressure as a bolus. We could not control body temperature strictly, while we used warming blankets. However, catecholamine, respiratory support or hypothermia did not have any influence on the accuracy of tcPCO2 measure.12 In addition, it should take 1 or 2 minutes for tcPCO2 to reflect PaCO2, but no strict delay was noticed.13 Therefore, after drawing the blood for arterial blood gas analysis, we measured tcPCO2, tcPO2, and EtCO2, but this might not be enough for the necessary time lag.
In laparoscopic surgery, tcPCO2 correlated well with PaCO2 except for during abdominal inflation, EtCO2 correlated well with PaCO2 only before inflation, and tcPO2 correlated well with PaO2 except for early phase of inflation in our previous study.8 TcPCO2 and EtCO2, and tcPO2 could not be surrogate measurement of PaCO2 and PaO2, respectively in laparoscopic surgery.8 EtCO2 may not reflect changes in PaCO2 during inflation because of changes in alveolar dead space, consequent to reduced cardiac output, increased ventilation-perfusion mismatching.14 The CO2 pneumoperitoneum results in the further decrease of functional residual capacity and greater degree of intrapulmonary shunt, which diminishes the accuracy of EtCO2. The CO2 partial pressure was at its highest 30 minutes after pneumoperitoneum and was stable 60 minutes after pneumoperitoneum.15 Therefore, as in our results, EtCO2 did not correlate well with PaCO2.
The relation between tcPCO2 and PaCO2, and tcPO2 and PaO2 are different in different phases of pneumoperitoneum. However, in the present study, we measured these at random, not according to the time course of the pneumoperitoneum because the purpose of this study was to know whether tcPCO2 and tcPO2 could be used to monitor PaCO2 and PaO2, respectively, not to know the difference according to the phases of pneumoperitoneum.
TcPCO2 and tcPO2 did not correlate with PaCO2 and PaO2, respectively, when PaCO2 > 56 mmHg and PaO2 > 115 mmHg.16 Almost all of the data in the present study showed PaO2 > 115 mmHg, but PaCO2 < 56 mmHg. Therefore, tcPCO2 should correlate well with PaCO2, but it was not in the present study.
TcPCO2 was reported to be better than EtCO2 to estimate PaCO2 in obese patients undergoing open4 and laparoscopic5 bariatric surgery. Dion et al showed that both tcPCO2 and EtCO2 had good correlation and lower bias and precision with PaCO2 in laparoscopic bariatric surgery.17 The differences between tcPCO2 and EtCO2, and EtCO2 and PaCO2 in their study were quite smaller than those in our present study, and also than those in our previous studies in non-obese patients.8-11 Although we could not know why they had so small differences, but from all of our data including non-obese subjects, we could not say that tcPCO2 and EtCO2were accurate measurements of PaCO2 during general anesthesia, especially in obese patients.
Bernhardt et al. showed that PjCO2 (5.5 + 0.9 x EtCO2 – 2.1 x tidal volume (L)) could be used for accurate estimation of PaCO2 in morbidly obese adults.18 However, this calculation is complicated not to be done instantly. Therefore, this is not clinically useful.
There has been no studies of tcPO2 in bariatric laparoscopic surgery. A thicker epidermal layer led to greater difference between PtcO2 and PaO2.12 Adiposity impairs the diffusion of oxygen through the skin.19 Therefore, out results showed tcPO2 could not show PaO2.
CONCLUSION
On the basis of the results of our study, we conclude that tcPO2 and tcPCO2 cannot be surrogate measurements of PaO2 and PaCO2, respectively in laparoscopic bariatric surgery.
Conflict of interest: Nil
REFERENCES
- Mason EE. Surgery in the obese. Lancet 2003;361:2001-2. [PubMed]
- Hedenstierna G, Santesson J. Breathing mechanics, dead space and gas exchange in the extremely obese, breathing spontaneously and during anaesthesia with intermittent positive pressure ventilation. Acta Anaesthesiol Scand. 1976;20:248-54. [PubMed]
- Oberg B, Poulsen TD. Obesity: an anaesthetic challenge. Acta Anaesthesiol Scand 1996;40:191-200. [PubMed] [Free full text]
- Griffin J, Terry BE, Burton RK, Ray TL, Keller BP, Landrum AL, et al. Comparison of end-tidal and transcutaneous measures of carbon dioxide during general anaesthesia in severely obese adults. Br J Anaesth 2003;91:498-501. [PubMed] [Free full text]
- Liu S, Sun J, Chen X, YU Y, Liu X, Liu C. The application of transcutanelus CO2 pressure monitoring in the anesthesia of obese patients undergoing laparoscopic bariatric surgery. PLoS ONE. 2014;9:e91563. doi: 10.1371/journal.pone.0091563 [PubMed] [Free full text]
- Xue Q, Wu X, Jun J, Yu B, Zheng M. Transcutaneous carbon dioxide monitoring accurately predicts arterial carbon dioxide partial pressure in patients undergoing prolonged laparoscopic surgery. Anesth Analg 2010; 111: 417-20. doi: 10.1213/ANE.0b013e3181e30b54.[PubMed]
- Ozyuvaci E, Demircioglu O, Toprak N, Topacoglu H, Sitilci T, Akyol O. Comparison of transcutaneous, arterial and end-tidal measurements of carbon dioxide during laparoscopic cholecystectomy in patients with chronic obstructive pulmonary disease. J Int Med Res 2012; 40: 1982-7. [PubMed]
- Nishiyama T. Transcutaneous carbon dioxide and oxygen pressure in laparoscopic surgery. The Internet Journal of Anesthesiology 2014, 33 , No.1. [Free full text]
- Nishiyama T, Kohno Y, Koishi K. Comparison of ear and chest probes in transcutaneous carbon dioxide pressure measurements during general anesthesia in adults. J Clin Monit Comput 2011; 25: 323-8. doi: 10.1007/s10877-011-9311-3. [PubMed]
- Nishiyama T, Nakamura S, Yamashita K. Comparison of the transcutaneous oxygen and carbon dioxide tension in different electrode locations during general anaesthesia. Eur J Anaesthesiol 2006;23:1049-54. [PubMed]
- Nishiyama T, Nakamura S, Yamashita K. Effects of the electrode temperature of a new monitor, TCM4, on the measurement of transcutaneous oxygen and carbon dioxide tension. J Anesth 2006;20:331-4. [PubMed]
- Rodriguez P, Lellouche F, Aboab J, Buisson BC, Brochard L. Transcutaneous arterial carbon dioxide pressure monitoring in critically ill adult patients. Intensive Care Med 2006;32:309-12. [PubMed]
- Kuzuta T, Kamide M, Kagawa S. Transcutaneous PCO2 (TcPCO2) reflects PaCO2 of previous 1 or 2 minutes. Jpn J Anesthesiol 2012;61:638-42. [PubMed]
- Nyarwaya JB, Mazoit JX, Samii K. Are pulse oximetry and end-tidal carbon dioxide tension monitoring reliable during laparoscopic surgery ? Anaesthesia 1994;49:775-8. [PubMed] [Free full text]
- Girardis M, Broi UD, Antonutto G, Pasetto A. The effect of laparoscopic cholecystectomy on cardiovascular function and pulmonary gas exchange. Anesth Analg 1996;83:134-40. [PubMed]
- Cuvelier A, Grigoriu B, Molano LC, Muir JF. Limitations of transcutaneous carbon dioxide measurements for assessing long-term mechanical ventilation. Chest. 2005; 127: 1744-8. [PubMed]
- Dion JM, McKee C, Tobias JD, Herz D, Sohner P, Teich S, Michalsky M. Carbon dioxide monitoring during laparoscopic-assisted bariatric surgery in severely obese patients: transcutaneous versus end-tidal techniques. J Clin Monit Comput 2015;29:183-6. doi: 10.1007/s10877-014-9587-1. [PubMed]
- Bernhardt V, Lorenzo S, Babb TG, Zavorsky GS. Corrected end-tidal PCO2 accurately estimates PaCO2 at rest and during exercize in morbidly obese adults. Chest 2013;143:471-7. [PubMed] [Free full text]
- Nishiguchi BK, Yu M, Suetsugu A, Jiang C, Takiguchi SA, Takanishi DM Jr. Determination of reference ranges for transcutaneous oxygen and carbon dioxide tension and the oxygen challenge test in healthy and morbidly obese subjects. J Surg Res 2008;150:204-11. [PubMed]

