Rajeev Sharma, MD1, Sushmita Bairagi, MBBS2, Sashmita Das3, Jyotika Kumar2
1Associate Professor; 2Post Graduate Trainee; 3Registrar
Department of Anesthesiology, Lady Hardinge Medical College & Associated Hospitals, New Delhi, (India)
Correspondence: Dr Rajeev Sharma, M.D, Associate Professor, Lady Hardinge Medical College & Associated Hospitals, New Delhi -110001, (India); Phone: +919990587318; E-mail: rajeevkrsharmaji@gmail.com
ABSTRACT:
Rhino-orbito-cerebral mucormycosis is an aggressive and potentially lethal invasive fungal infection. Surgical debridement and amphotericin B remain the mainstay of treatment, however, associated side effects of amphotericin B like nephrotoxicity, hypokalemia, hypertension and arrhythmias need to be addressed. We discuss the anesthetic management of a 47 year old male with uncontrolled diabetes diagnosed with left sinoorbital mucormycosis posted for surgical debridement. The patient received amphotericin B and insulin preoperatively. Nephrotoxicity due to amphotericin B led to hypokalemia in this patient. We also discuss the role of liposomal formulation in preventing hypokalemia and other side effects associated with use of amphotericin.
Key words: Mucormycosis; Hypokalemia; Amphotericin B
Citation: Sharma R, Bairagi S, Das S, Kumar J. Amphotericin B induced hypokalemia in a diabetic patient with rhino-orbitocerebral mucormycosis. Anaesth Pain & Intensive Care 2017;21(1):90-93
Received: 28 Dec 2016; Reviewed & Accepted: 5 Mar 2017
INTRODUCTION:
Rhino-orbito-cerebral mucormycosis is a fulminant, opportunistic fungal infection commonly seen in diabetes.1 The classic presentation is involvement of nasal mucosa with invasion into paranasal sinuses, orbit and the central nervous system.1 Management includes aggressive surgical debridement, systemic antifungal therapy with amphotericin B (AmB) and treating the underlying comorbidities.2 The nephrotoxic side effect of AmB sometimes requires its discontinuation. Lipid formulation of AmB are better tolerated and used mainly in patients who have already altered renal function.3
CASE REPORT:
A 45 years old male farmer weighing 70 kg presented to the ophthalmology department of our hospital with fever since last10 days, nasal stuffiness associated with bleeding since 6 days, pain and protrusion of left eye since 6 days and diplopia with complete loss of vision in left eye since 2 days. A family history of diabetes was found but the patient had never been evaluated for the same. He was diagnosed one month back with hypertension and was taking oral amlodipine 5 mg and olmesartan 40 mg daily.
Ophthalmologic examination revealed proptosis (Figure 1) and complete loss of vision in left eye with loss of pupillary reflex. MRI showed extensive bilateral ethmoid and left maxillary sinusitis (Figure 2 and 3).

Figure 1: Preoperative photograph of patient showing swelling and proptosis of left eye
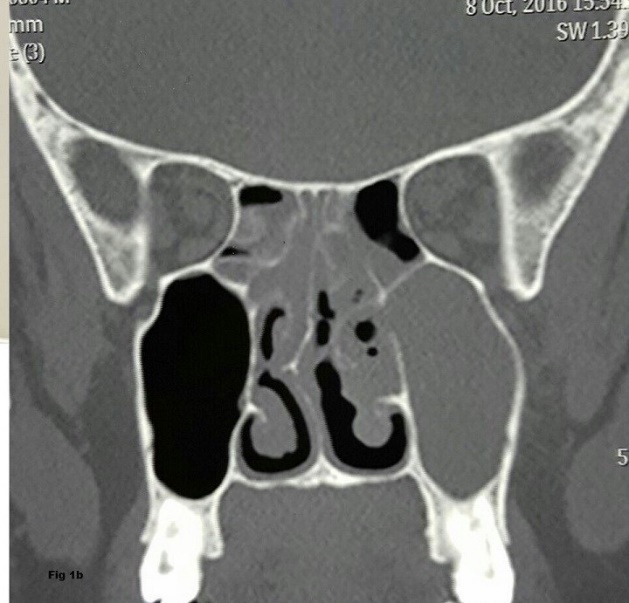
Figure 2: MRI image showing infiltration of maxillary sinus
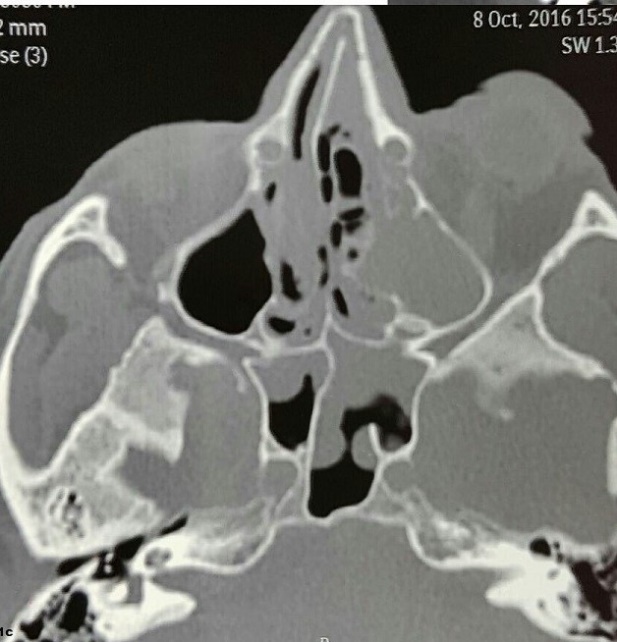
Figure 3: Infiltration of ethmoid sinus and optic nerve compression
Deviation of nasal septum towards the right side with obliteration of sinus drainage channels was also seen. Frontal and sphenoethmoidal recess was obliterated and left optic nerve compression was reported (Figure 3). Fasting blood sugar was 15.5 mmol/L and HbA1c level was 14.4. He was started on regular subcutaneous insulin which needed to be increased to 18 units per day in three divided doses. The baseline blood urea was 30 mg/dl, serum creatinine was 0.8 mg mg/dl and serum potassium levels (K+) was 4.2 meq/L. Urine sugar was positive but ketones were negative. Otolaryngology consultation was done, nasal swabs were sent for histopathological examination and AmB 1mg/kg/day IV was started along with amoxicillin and clavulanic acid combination 1.2 g 8 hourly. Fungal hyphae were seen on histopathological examination of nasal swabs and a diagnosis of rhino-orbitocerebral mucormycosis was made.
Patient was sent for pre-anesthetic examination for endoscopic surgical debridement after 2 days when the blood sugar charting became normal. Routine investigations were normal except for serum potassium which had decreased to 2.6 meq/L and serum creatinine 1.8 mg/dl. On the day before surgery, AmB was stopped and liposomal inj. AmB 300 mg was started; inj caspofungin 50 mg IV OD and potassium chloride syrup were also added.
On examination, patient was conscious, oriented, responding to verbal commands. Pulse rate was 92/ min, blood pressure was 140/90 mmHg. His fasting blood sugar was 5.5 mmol/l, Na+ – 135 meq/l, K+– 2.6 meq/L, urea-31 mg/dl and serum creatinine – 1.8 mg/dl. Arterial blood gas report showed pH- 7.50, PCO2 – 29.9, PO2 – 106, HCO3 – 23.2. Electrocardiogram and chest x ray were normal.
A written informed consent was taken. Electrocardiogram, noninvasive blood pressure, Pulse Oximeter monitors were attached. Right sided ulnar nerve was used for neuromuscular monitoring using train of four (TOF) ratio. Patient was premedicated with inj. fentanyl 150 micrograms IV and induction was achieved using inj. propofol 140 mg IV. Inj. rocuronium bromide 45 mg was administered after ensuring adequate mask ventilation using oxygen, nitrous oxide and sevoflurane. Orotracheal intubation was performed using a size 8.0 cuffed endotracheal tube on direct laryngoscopy at TOF value of 0. Pharyngeal packing was done around the endotracheal tube.
Anesthesia was maintained using oxygen, nitrous oxide and sevoflurane. Rocuronium was repeated using Train of Four (TOF) ratio. Two IV lines were used for fluid administration. On one side, normal saline infusion was started and on the other side an infusion containing 5% dextrose with 8 unit regular insulin and 20 meq KCl at 100 ml/h was given. Intraoperative blood pressure was in range of 130-140 mmHg systolic and 70-80 mmHg diastolic; blood sugar levels were in range 5.5- 7.7 mmol/L.
Extensive endoscopic surgical debridement was performed in ethmoid and maxillary sinuses and typical mucor infested tissues were removed. Anterior and posterior ethmoidectomy and uncenectomy was done, maxillary osteum was widened and fungal debris was removed. Surgical duration was 90 min. Paracetamol 1 g IV was given for pain relief. On completion of surgery the pharyngeal pack was removed. Inj. ondansetron 8 mg IV was given as antiemetic. Neuromuscular block was reversed with inj. glycopyrrolate 0.6 mg and inj. neostigmine 3.5 mg IV. Tracheal extubation was performed at TOF ratio of 0.9. The patient was monitored in the postoperative unit and later shifted to the ward. Liposomal AmB, insulin and other drugs were continued. The patient showed significant clinical improvement (except for the vision in the left eye which did not improve during hospital stay) his hypokalemia and creatinine gradually improved and was discharged from the hospital after 2 weeks. Consent has been taken from the patient for publication of details.
DISCUSSION:
Rhino orbitocerebral mucormycosis is an opportunistic fungal infection. This fungus thrives in acidic pH and glucose rich medium enhances its growth as it impairs neutrophil chemotaxis and decrease phagocytosis.1,2 This is the reason it is usually seen in diabetic patients. The earliest sign is facial edema, proptosis, chemosis and extraocular muscle paresis, periorbital edema and mucopurulent rhinorrhea.1 Infection spreads rapidly from sinus to orbit to CNS. It occurs by angioinvasion, propagating thrombosis and associated with tissue infarction and necrosis.1 With intracranial extension, MRI is the imaging modality of choice.
Treatment includes extensive surgical debridement, high doses of systemic amphotericin B and control of underlying disease.3 Amphotericin B has its side effects and toxicity that will sometimes requires discontinuation of therapy despite a life-threatening systemic fungal infection.4 Amphotericin B administration causes proinflammatory cytokine production. The acute toxicity includes nausea, vomiting, fever, hypertension or hypotension, and hypoxia.4
Its principal adverse effect is nephrotoxicity. Risk factors of amphotericin B nephrotoxicity include male gender, high average daily dose of amphotericin B (≥ 35 mg/day) diuretic use, body weight ≥ 90kg5, concomitant use of nephrotoxic drugs and abnormal baseline renal function. Clinical manifestation of AmB nephrotoxicity includes renal insufficiency, hypokalemia, hypomagnesemia, metabolic academia and polyuria due to nephrogenic diabetes insipidus.
Our patient was treated with AmB since the day of admission. Liposomal AmB was not available initially and could be added a day before surgery only. The serum K+ level decreased to 2.6 meq/l and Creatinine increased to 1.8 mg/dl which may be due to the nephrotoxic effect of AmB. Studies indicate that renal function is impaired in more than 80% of patients treated with AmB, with 15% of patients requiring hemodialysis.6 The anesthetic management of patients with acute tubular necrosis leading to development of acute renal failure is of particular concern for anesthesia providers. Anesthetic management aims at maintenance of an adequate mean arterial pressure while concomitantly avoiding further renal insults. A heightened awareness for renal, electrolyte, hemodynamic, and respiratory aberrancies is warranted for anesthesia providers when treating patients receiving AmB therapy. AmB induced hypokalemia may enhance the effect of skeletal muscle relaxants when administered concomitantly serum potassium levels should be closely monitored.
Hypokalemia can lead to prolonged duration of action of non depolarising neuromuscular blocking agents and lead to delayed or incomplete recovery after the surgery.7 Hypokalemia also predisposes to arrhythmias and paralytic ileus.7 We used neuromuscular monitoring (TOF) to give optimum doses of rocuronium to avoid these complications.
Since, hypokalemia denotes an intracellular deficit of K+, it important not to aim at its rapid correction in short time period. There were no ECG changes of hypokalemia and we did not aim to correct the levels in the 90 min duration surgery. The patient received oral K+ supplementation preoperatively and low concentration of potassium chloride was given as part of GKI regimen (Glucose-Potassium-Insulin) for diabetes mellitus.
AmB lipid preparations are more tolerable, more efficacious and less nephrotoxic. But due to high cost and relative paucity of clinical data lipid formulations are generally used as second line therapy.
To conclude, we emphasize the importance of adequate blood sugar control, need for urgent surgical debridement, and knowledge about the important side effects of AmB like nephrotoxicity and hypokalemia and its relevance to neuromuscular block and knowledge about the better safety profile of Liposomal AmB in treatment of patients with rhino-orbitocerebral mucormycosis patients.
Conflicts of Interests: None
Financial Disclosures: None
Author contribution: RS: Concept, conduct, writing, editing
SB: Conduct, data
SD: Conduct, data, editing
JK: Conduct, data
REFERENCES:
- Nithyanandam S, Jacob MS, Battu RR, Thomas RK, Correa MA, D’Souza O. Rhino-orbito-cerebral mucormycosis. A retrospective analysis of clinical features and treatment outcomes. Indian J Ophthalmol. 2003 Sep;51(3):231-236. [PubMed] [Free full text]
- Ferguson BJ. Mucormycosis of nose and paranasal sinuses. Otolaryngol Clin North Am. 2000 Apr;33(2):349-65. [PubMed]
- Peterson KL, Wang M, Canalis RF, Abemayor E. Rhinocerebral mucormycosis: evolution of the disease and treatment options. Laryngoscope. 1997 Jul;107(7):855-62. [PubMed]
- Laniado-Laborin R, Cabrales Vargas MN. Amphotericin B: side effects and toxicity. Rev Iberam Mycol. 2009 Dec 31;6(4):223-227. doi: 10.1016/j.riam.2009.06.003. [PubMed]
- Fisher MA, Talbot GH, Maislin G, McKeon BP, Tynan KP, Strom BL. Risk factors for Amphotericin B-associated nephrotoxicity. Am J Med. 1989 Nov;87(5):547–52. [PubMed]
- Wong KC, Schafer PG, Schultz JR. Hypokalemia and anesthetic implications. Anesth Analg. 1993 Dec;77(6):1238-60. [PubMed]
- Walsh TJ, Finberg RW, Arndt C, Hiemenz J, Schwartz G, Bodenstiener D, et al. Liposomal amphotericin b for empirical therapy in patients with persistent fever and neutropenia. National Institute of Allergy and Infectioiou Diseases Mycoses Study Group. N Engl J Med. 1999 Mar;340(10):764–71. [PubMed] [Free full text]




 Facebook
Facebook Twitter
Twitter GooglePlus
GooglePlus Youtube
Youtube