Mohammed Kazim1, Varsha Kothari2, Shivam Priyadarshi3, Tuhin Mistry4, Rajeev Prajapati5, Rajni Mathur2
1Assistant professor, Department of Anesthesiology, Malabar Medical College, Kozhikode (India)
2Professor; 5Senior Resident
Department of Anesthesiology, SMS Medical College, Jaipur (India)
3Professor of Urology, SMS Medical College, Jaipur (India)
4Senior Resident, Department of Anesthesiology, AIIMS, Raipur (India)
Correspondence: Dr. Mohammed Kazim, H. No 8-1126, Ashowk Chowk, Near Bamboo Bazar Gulbarga, Karnataka 585104 (India); E-mail: dr.mdkazim88@gmail.com
ABSTRACT:
Aims and Background: To prolong postoperative analgesia many adjuvants has been used opioids and alpha-2 agonists are very popular among them. This study was aimed at comparing the sensory, motor, hemodynamic, sedative and analgesic properties of epidural administration of fentanyl and dexmedetomidine as an adjuvant to ropivacaine.
Methodology: With Institutional ethical committee clearance this study was conducted at our hospital. After obtaining informed and written consent, a total of 60 patients scheduled for elective percutaneous nephrolithotomy (PCNL) were randomly allocated into two groups of 30 each. Patients of both genders, aged 21-60 y, ASA physical status I and II were enrolled. Group RD received 28 ml of inj ropivacaine 0.5% + dexmedetomidine 1 μg/kg and Group RF received 28 ml of ropivacaine 0.5% + inj fentanyl 1 μg/kg epidurally. Hemodynamic parameters, sedation scores, and time to onset of sensory loss, complete motor blockade, two segmental dermatomal regression and time of first rescue analgesic were recorded. Data were compiled systematically and analyzed using unpaired t-test, Chi‑square and Mann-Whitney U test. P < 0.05 was considered significant.
Results: The demographic profile of patients was comparable in both groups. Onset of sensory analgesia up to T10 was 6.8 ± 2.8 min vs. 8.7 ± 2.7 min and time to reach maximum motor block was 19.8 ± 5.8 min vs. 23.9 ± 4.9 min in Group RD and Group RF respectively, which was significantly less in the Group RD. Postoperative analgesia was significantly prolonged in the Group RF as compared to Group RD, e.g. 394.5 ± 36.5 vs. 268.5 ± 28.3 min respectively. Sedation scores were better in the Group RD and highly significant on statistical comparison (P < 0.001). Incidence of hypotension, nausea and vomiting was high in the Group RF, while incidence of dry mouth was higher in the Group RD.
Conclusion: Dexmedetomidine is a better adjuvant than fentanyl when added to epidural ropivacaine in terms of early onset of sensory and motor block, prolonged postoperative analgesia and better sedation with less side effects.
Key words: Epidural Anesthesia; Ropivacaine; PCNL; Dexmedetomidine; Fentanyl
Citation: Kazim M, Kothari V, Priyadarshi S, Mistry T, Prajapati R, Mathur R. A comparative study to assess the effect of dexmedetomidine and fentanyl as an adjuvant to ropivacaine for epidural anesthesia in percutaneous nephrolithotomy. Anaesth, Pain & Intensive Care 2017;21(1):59-64
Declaration: The data have been presented in part at 63rd ISACON,Jaipur; Dec 2015
Received: 26 Dec 2016; Reviewed: 18, 25 Feb 2017; Corrected & accepted: 24 Mar 2017
INTRODUCTION:
Pain in the postoperative period is one of the major factors that impede recovery from anesthesia and surgery. Percutaneous nephrolithotomy (PCNL) can be performed under general anesthesia (GA) or regional anesthesia. PCNL under epidural anesthesia has some unique advantages over GA, such as lesser postoperative pain, lower dose requirement for analgesic drugs, and avoidance of the side effects from multiple medications during GA.1-7 Thus, epidural anesthesia has many advantages of providing analgesia for prolonged duration with repeated top-ups and also it is the preferred technique of choice for providing excellent postoperative analgesia.
Ropivacaine is a S-enantiomer with less cardiotoxic effect and with less propensity to block motor fibers. Hence this drug is a better alternative to bupivacaine. Combination of opioids and local anesthetic (LA) for epidural anesthesia and analgesia has been used in many studies with reported benefits like decreasing the dose of LA, rapid onset and decreasing side effect of each drug when used alone.8 Epidural fentanyl has been commonly used in neuraxial blockades as a better alternative to morphine to attenuate the side effects like respiratory depression. The adjuvants like central alpha-2 agonists acts by opioid independent mechanism. Dexmedetomidine is a selective alpha-2 agonist with sympatholytic, sedative, amnesic and analgesic properties and so the opioid sparing analgesia can be achieved. Keeping in mind all pharmacological profile of these drugs, we conducted a study with the aim of comparing the sensory, motor, analgesic and sedative properties of dexmedetomidine and fentanyl as an adjuvant to epidural ropivacaine.
METHODOLOGY:
It was a hospital based double blind, randomized comparative study, done in a tertiary care centre. After approval from the institutional ethical committee and review board, written informed consent was obtained from each patient for performance of epidural anesthesia after complete explanation about the study. We included 60 patients undergoing PCNL who were randomly allocated into two groups of 30 patients in each. Patients of either sex with age between 20-60 years and ASA physical status l and II were included and patients with any contra indication to regional anesthesia and allergy to local anesthetics were excluded from the study.
Patients were premedicated with inj. ranitidine 50 mg IV and midazolam 1 mg IV one hour prior to the procedure. Baseline vital signs like NIBP, pulse rate, respiratory rate and SpO2 were recorded. After securing an 18 G IV cannula, preloading was done with 10-15 ml/kg lactated ringer solution.
Patients were positioned in left lateral decubitus position assisted by OT staff. Lumbar epidural puncture was performed with 18G Tuohy needle in L1-L2 interspace. The identification of the epidural space was done with loss of resistance technique using normal saline; a test dose of 3 ml of 2% lignocaine plus adrenaline (1:200,000) was given and epidural catheter secured at 3-5 cm in epidural space. The patients were allocated to groups by using lottery method and study drug was loaded by one colleague who was unaware of study design and was administered by the lead author.
The drugs were given slowly over one minute with negative aspiration and in incremental doses. A total of 28 ml of inj ropivacaine 0.5% + dexmedetomidine in Group RD, and an equal volume of ropivacaine 0.5% + fentanyl 1 mg/kg in Group RF, diluted to make a total of 30 ml volume respectively.
After injecting patients were turned supine and vital signs were recorded. The patients were given 4 L/min of oxygen by face mask. Sensory and motor parameters were assessed after every 1 min and patient was given prone position only after desired grade of sensory and motor level achieved and surgery was started 30 min after epidural injection. The following parameters were observed
- Time to onset of sensory block at T10
- Maximum sensory level achieved
- Time taken to achieve the maximum sensory level
- Time taken to complete motor blockade
- Time taken to two segmental dermatomal regression
- Sensory regression to S2
- Total duration of analgesia
Grading of motor block was done by modified Bromage score, e.g. 0 = no block; 1 = inability to raise extended leg; 2 = inability to flex knees; 3 = inability to flex ankles and feet.
The pain score was determined by numerical rating scale (NRS), in which the patient marks the score on a scale numbered from 0 to 10 [0 = no pain, 1-3 = mild pain, 4-6 = moderate pain,7-9 = severe pain, 10 = worst imaginable pain].
Sedation was also assessed at intervals of 10 min intraoperatively and at intervals of 1 hour during postoperative period using Ramsay sedation scale, e.g.
1 = anxious and agitated or restless, 2 = cooperative, oriented and tranquil, 3 = responding to commands only, 4 = brisk response to a light glabellar tap or auditory stimulus, 5 = asleep, sluggish response to light glabellar tap or auditory stimulus and 6 = no response to painful stimulus.
The various side effects were noted and managed accordingly.
The sample size was calculated as 26 subjects in each group at alpha error of 0.05 and power 80% assuming difference in mean of complete motor block from a pilot study done on 10 patients in each group and considering 10% drop out 30 patients were included in each group.
Statistical analysis: It was performed with IBM SPSS Statistics for Windows, Version 21 (SPSS Inc., Chicago, IL, USA). The categorical data were presented as numbers (percent) and were compared among groups using Chi square test. The quantitative data were presented as mean ± standard deviation and were compared by Student’s unpaired t-test. Probability was considered to be significant if less than 0.05.
RESULTS:
In our study 60 ASA I and II grade patients posted for PCNL were chosen and randomly divided into two groups of 30 each. The demographic data (age, weight and BMI) were comparable in both the groups without any significant difference (p < 0.05).
Table 1: Demographic parameters [mean ± SD]
| Parameter | Group RD
(n=30) |
Group RF
(n=30) |
p value |
| Age (y) | 37.2 ± 11.6 | 37.7 ± 12.8 | 0.882 |
| Weight (kg) | 67.6 ± 8.2 | 63.8 ± 10.7 | 0.130 |
| BMI (kg/m2) | 24.27 ± 2.96 | 23.06 ± 4.15 | 0.197 |
| ASA (l/ll) | 22/8 | 27/3 | – |
The time of onset of sensory block at T10 in Group RD was earlier compared to Group RF (6.8 ± 2.2 min vs. 8.7 ± 1.8 min) and time to reach maximum motor block (19.8 ± 5.8 min vs 23.9 ± 4.9 min) was also earlier but the maximum level reached in both the groups were comparable (Table 2 & 3).
Table 2: Initial block parameters [mean ± SD]
| Parameter (min) | Group RD
(n=30) |
Group RF
(n=30) |
p value |
| Sensory onset at T10 | 6.8 ± 2.2 | 8.7 ± 1.8 | 0.0004 |
| Time taken for maximum sensory block | 15.7 ± 1.8 | 16.4 ± 2.3 | <0.01 |
| Time taken to reach maximum motor block | 19.8 ± 2.5 | 23.9 ± 2.4 | 0.225 |
Table 3 Postop block parameters: [mean ± SD]
| Parameter (min) | Group RD
(n=30) |
Group RF
(n=30) |
p value |
| Time taken for sensory
regression to S1 |
150.6 ± 8.9 | 129.0 ± 9.5 | < 0.01 |
| Time taken for 2 segment Regression |
150.6 ± 8.9 | 129.0 ± 9.5 | < 0.01 |
| Time taken for regression to lowest Bromage l | 251.8 ± 21.5 | 178.9 ± 15.1 | < 0.01 |
| Time to first rescue analgesia | 394.5 ± 20.5 | 268.3 ± 13.1 | < 0.01 |
There were no statistically significant differences in mean heart rate and mean arterial pressure at different time periods between the two groups (Figures 1 & 2).
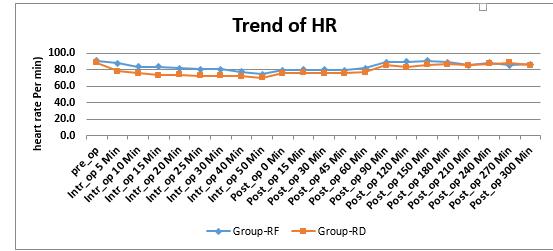
Figure 1: Comparative changes in heart rates
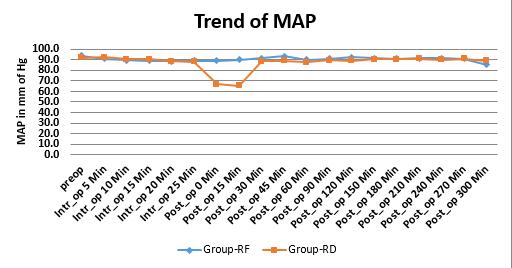
Figures 2: Comparative changes in mean blood pressures
In postoperative block characteristics time for regression of motor block to Bromage l (251.8 ± 21.5 min vs. 178.9 ± 15.1 min) and time for 2 segmental regression (150.6 ± 8.9 min vs. 129.0 ± 9.5 min) observed and which were significantly prolonged in the Group RD in comparison to Group RF. Duration for rescue analgesia was also prolonged in Group RD (394.5 ± 36.5 min vs. 268.5 ± 28.3 min) when compared to Group RF (Table 3).
The Ramsay sedation score which was used in this study showed a better score in RD group (Figure 3).
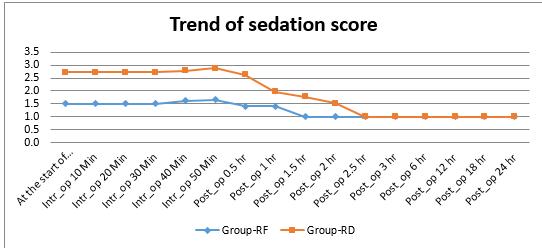
Figure 3: Comparison of Ramsay sedation scores
Table 4: Comparison of side effects
| Side-effects | Group RD
(n=30) |
Group RF
(n=30) |
p value |
| Nausea | 2(6.6) | 4(13.2) | 0.049 |
| Vomiting | 3(10) | 5(16.3) | 0.447 |
| Shivering | 0 | 1(3.3) | |
| Hypotension | 3(10) | 1(3.3) | 0.447 |
| Bradycardia | 1(3.3) | 0 | |
| Dry Mouth | 3(10) | 0 | |
| Pruritus | 0 | 1(3.3) |
Figures in bracket are in percentage
The differences in the frequency of side effects were non-significant (Table 4).
DISCUSSION:
Percutaneous nephrolithotomy is a minimally invasive surgery which is an accepted treatment for large renal and upper ureteric calculi, though GA is the preferred mode of anesthesia for PCNL but because of possibility of fluid absorption and electrolyte imbalance, especially in staghorn stones and also in morbid obese patients and COPD regional anesthesia(RA) may be a good alternative then GA1, also the early mobilization and decreased postoperative nausea vomiting and better postoperative analgesia with RA when compared to GA.2
Various adjuvants has been used in various studies to shorten the onset and prolong the action of LA e.g. morphine, fentanyl, sufentanyl, magnesium, ketamine, calcitonin, clonidine and dexmedetomidine.8,9 The use of neuraxial opioids is associated with side effects such as nausea, pruritus, respiratory depression and urinary retention, so α-2 agonists are being extensively studied as an alternative to opioid adjuvants.3,4
In our study we found out that RD grp had early onset of motor as well as sensory blockade compared to RF which is in concordance with the earlier studies.10-19
Duration of motor block as well as the time taken for two segmental regression was higher in Group RD but the highest sensory level achieved was same in both the groups, Bajwa et al10 concluded that dexmedetomidine was a better adjuvant in terms of prolonging the duration of 2 segmental regression and providing better intraop and postop analgesia.
Hemodynamic parameters were comparable in both the groups, though heart rate was decreased in RD group 40 min after the drug administration but that was not significant, in one patient we used atropine to treat the bradycardia (< 60/min). Mean arterial blood pressure remained stable in both groups and statistically not significant and so was the consumption of vasopressors.
In one of the earlier studies conducted by Rastogi et al also reported about the hemodynamic stability, prolongation of duration of analgesia, and good sedation with dexmedetomidine.16
Total duration of analgesia was prolonged in the RD group and the rescue analgesia was given when VAS score was 4. We took rescue analgesia as the end point of the study and after that we gave inj.diclofenac aqueous. Babu et al.18 conducted a study to compare epidural ropivacaine with dexmedetomidine and ropivacaine with clonidine for postoperative analgesia and concluded that dexmedetomidine prolongs the analgesic duration as well as decreases the consumption of rescue analgesics in the postoperative period.
In PCNL surgery prone position is given, that will be uncomfortable position for patient without any sedation in regional anesthesia, so alpha-2 agonist is quite helpful which produces its sedative action via presynaptic alpha-2 adrenoreceptors in the locus ceruleus, which leads to inhibition of release of norepinephrine and hence its beneficial effect. Dexmedetomidine causes the cooperative sedation which is unique because arousal and response to commands maintained despite deep level of sedation. In our study significant difference was observed in subjective sedation score during intraoperatively and prolonged up to 2 hr 30 min postoperatively in Group RD.
In our study incidence of nausea and vomiting was comparable in both the groups and it was non-significant but in one study by Bajwa et al10 nausea and vomiting was more in fentanyl group compared to dexmedetomidine. Dry mouth which is known side effect of alpha-2 agonist was seen only in one patient in RD group in our study which is similar to previous studies. Respiratory depression was not seen in both the groups which shows that fentanyl is less depressant compared to the other opioids like morphine.20
CONCLUSION:
Dexmedetomidine is a better adjuvant to epidural ropivacaine when compared to fentanyl, with early onset and prolonged duration of sensory and motor blockade with better hemodynamic stability and intraoperative sedation and also analgesic sparing effect in the postoperative period.
Conflict of interest: None declared by the authors
Authors Contribution:
MK: conduction of study and preparation of manuscript
VK: conduction of study and proof reading
SP: conduction of study and statistical data analysis
TM: statistical data analysis and proof reading
RP: conduction of study
RM: preparation of manuscript and proof reading
REFERENCES:
- Aravantinos E, Karatzas A, Gravas S, Tzortzis V, Melekos M. Feasibility of percutaneous nephrolithotomy under assisted local anaesthesia: a prospective study on selected patients with upper urinary tract obstruction. Eur Urol. 2007 Jan;51(1):224-7. [PubMed] [Free full text]
- Kumawat T, Kothari V, Priyadarshi S, Mistry T, Morwal S. Study comparing the efficacy and safety of epidural anesthesia versus general anesthesia in patients undergoing percutaneous nephrolithotomy. Ain-Shams J Anaesthesiol. 2016;9:353–357. [Free full text]
- Chiary A, Lorber C, Eisnach JC, Wildling E, Krenn C, Zavrsky A, et al. Analgesic and hemodynamic effects of intrathecal clonidine as the sole analgesic agent during first stage of labor. Anesthesiology. 1999 Aug;91(2):388-96. [PubMed] [Free full text]
- Arian SR, Ruehlow RM, Uhrich TD, Ebert TJ. The efficacy of dexmedetomedine versus morphine for post operative analgesia after major inpatient surgery. Anesth Analg. 2004 Jan;98(1):153-8. [PubMed]
- Sarvana Babu MS, Verma AK, Agarwal A,Tyagi CM, Upadhyay M, Tripathi S.A comparative study in the post-operative spine surgeries: Epidural ropivacaine with dexmedetomidine and ropivacaine with clonidine for post –operative analgesia. Indian J Anaesth. 2013 Jul;57(4):371-6. doi: 10.4103/0019-5049.118563. [PubMed] [Free full text]
- Singh V, Sinha RJ, Sankhwar SN, Malik A. A prospective randomized study comparing percutaneous nephrolithotomy under combined spinal-epidural anesthesia with percutaneous nephrolithotomy under general anesthesia. Urol Int. 2011;87(3):293–8. doi: 10.1159/000329796 [PubMed]
- Ozalp G, Guner F, Kuru N, Kadiogullari N. Postoperative patient-controlled epidural analgesia with opioid bupivacaine mixtures. Can J Anaesth.1998 Oct;45(10):938-42. [PubMed]
- Bakshi U, Chatterjee S, Sengupta S , Gupta D. Adjuvant Drugs In Central Neuraxial Analgesia- A Review. The Internet J Anesthesiol. 2009;26. [Free full text]
- Bajwa SJ, Arora V, Kaur J, Singh A, Parmar SS. Comparative evaluation of dexmedetomidine and fentanyl for epidural analgesia in lower limb orthopedic surgeries. Saudi J Anesth. 2011 Oct;5(4):365-70. doi: 10.4103/1658-354X.87264. [PubMed] [Free full text]
- Thimmappa M, Madhusudhana R, PotliS, Karthick D comparative study of epidural ropivacaine 0.75% alone with ropivacaine plus clonidine and Ropivacaine plus dexmedetomidine for lower Abdominal and lower limb surgeries. World Journal of Pharmacy and Pharmaceutical Sciences 2014 3(4):1218-30. [Free full text]
- Kaur J, Bajwa SJ. Comparison of epidural butorphanol and fentanyl as adjuvants in the lower abdominal surgery: A randomized clinical study. Saudi J Anaesth. 2014;8:167-71 doi: 10.4103/1658-354X.130687.. [PubMed] [Free full text]
- Aantaa R, Kanto J, Scheinin M, Kallio A, Scheinin H. Dexmedetomedine, an alpha 2- adrenoreceptor agonist, reduces anaesthetic requirements for patients undergoing minor gynaecologic surgery. Anaesthesiology. 1990 Aug;73(2):230-5. [PubMed]
- Coskuner I, Tekin M, Kati I, Yagmur S, Elcicek K. Effects of dexmedetomedine on duration of anaesthesia and wakefulness in bupivacaine epidural block. Eur J Anaesthesiol. 2007 Jun;24(6):535-40. [PubMed]
- Arian SR, Ruehlow RM, Uhrich TD, Ebert TJ. The efficacy of dexmedetomedine versus morphine for post operative analgesia after major inpatient surgery. Anesth Analg. 2004 Jan;98(1):153-8. [PubMed]
- Bhawana Rastogi, VP singh, Deepti Mangla, Kumkum Gupta, Manish Jain, MN Pandey. Dexmedetomidine as an adjuvant to epidural 0.75% ropivacaine in patients undergoing infraumbilical surgery: A Clinical Study. Glob Anaesth Perioper Med. 2015;1(1): 19-23. [Free full text]
- Gupta K, Rastogi B, Gupta PK, Jain M, Gupta S,Mangla D. Epidural 0.5% levobupivacaine with dexmedetomidine versus fentanyl for vaginal hysterectomy: A prospective study. Indian J Pain 2014;28:149-54. [Free full text]
- Sarvana Babu M, Verma AK, Agarwal A, Tyagi CM, Upadhyay M, Tripathi S.A comparative study in the post-operative spine surgeries: Epidural ropivacaine with dexmedetomidine and ropivacaine with clonidine for post –operative analgesia. Indian J Anaesth. 2013;57:371-6. doi: 10.4103/0019-5049.118563.[PubMed] [Free full text]
- Neogi M, Bhattacharjee DP, Dawn S, Chatterjee N. A comparative study between clonidine and dexmedetomidine used as adjuncts to ropivacaine for caudal analgesia in paediatric patients. J Anaesthesiol Clin Pharmacol. 2010;26:149–53.
- Gehling M, Tryba M. Risks and side effects of intrathecal morphine combined with spinal anaesthesia:a meta-analysis. Anaesthesia. 2009 Jun;64(6):643-51. [PubMed] [Free full text]

